Purpose/Background
Anastomotic leak (AL) is a devastating complication of colo-rectal surgery. Reported incidence varies from 1- 30%. According to ISGRC 2010, AL is a defect at anastomotic site leading to communication between intraluminal and extraluminal compartments. Diagnosis is based on clinical, radiological, or endoscopic findings. AL is associated with significant morbidity (>20%) and mortality (~10%) rates. This study evaluated the risk factors for AL following colo-rectal surgeries, and its impact on morbidity and mortality.
Methodology:
This prospective observational study, conducted at a tertiary care teaching hospital in India. Patients undergoing colo-rectal surgery involving anastomosis were included in study. Preoperative investigations and postoperative outcome parameters were recorded. Patients with proximal diversion were excluded from the study. Postoperative complications occurring within 30 days were noted. Following parameters were studied-
1) Patient factors: Age, gender, comorbidity, serum albumin, haemoglobin etc.
2) Operative factors: Duration of surgery, blood loss, vasopressor support, blood transfusion.
3) Disease related factors: Malignant/Benign pathology, emergency/elective.
These factors were analysed using univariate and multivariate analysis.
Results/Outcomes:
65 patients were included in our study. Patient characteristics shown in table 1. Mean preoperative haemoglobin and albumin was 10.15+/-2.314 g and 3.68 +/-0.704 g/dl respectively. Mean duration of surgery 3.62 +/- 0.779 hours. AL was seen in 8/65 (12.3%). Grade A leak in 2 (3.1%) patients, grade B in 1 (1.5%) and grade C in 5 (7.7%) patients. Mean preoperative albumin was 2.96 +/- 0.82 g/dl in AL whereas 3.78+/- 0.63 g/dl in patients without AL (p value = 0.002). Similarly, mean albumin level on day 3 of surgery was 2.1+/- 0.59 g/dl in AL group whereas it was 2.75+/- 0.48 g/dl in patients without AL (p value = 0.001). Also, mean postoperative day 3 CRP level was significantly higher in patients with AL as compared to those without AL (76.1+/-12.1mg/dl versus 46.6+/-18.0 mg/dl respectively) (p value = 0.001). Operative blood loss of more than 200 ml was also significantly associated with AL (p value = 0.007). Mean hospital stay in AL group was 16.8 +/-14.2 days versus 8.5 +/- 5.7 days, in no AL. A total of 4 mortalities occurred in our study, out of which 3 (75%) patients had AL. No significant difference in incidence of AL was seen between open or laparoscopic, emergency or elective, benign or malignant pathologies as well as age or gender.
Conclusion/Discussion:
The incidence of AL in our study was 12.3%. Preoperative serum albumin, postoperative day 3 serum albumin and CRP level differ significantly in cases of AL versus no leak. AL increased morbidity, mortality and hospital stay. Increased operative blood loss also increased the chances of developing AL.
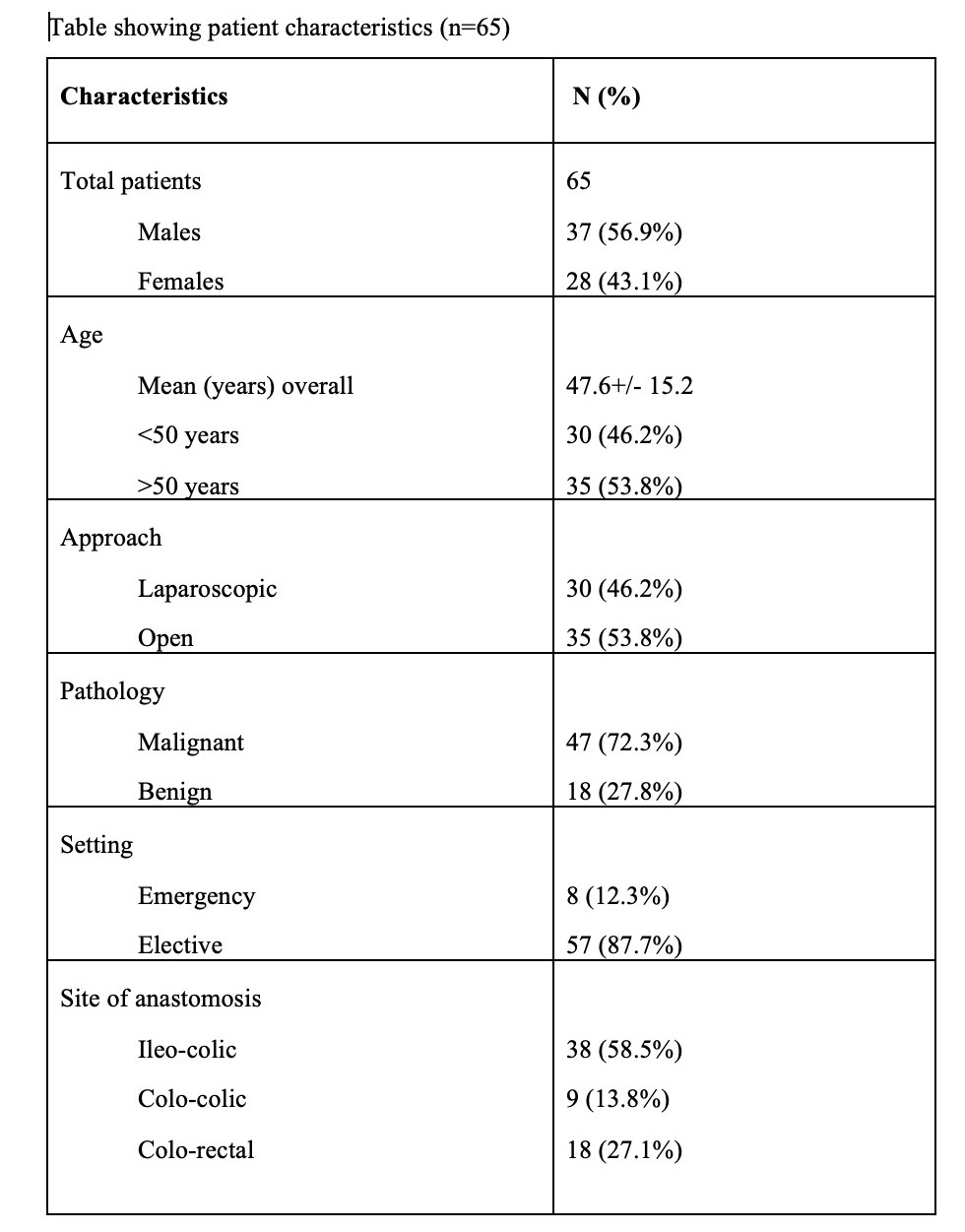
TABLE DEPICTING CHARACTERSTICS OF PATIENTS UNDER STUDY