Purpose: This study aimed to determine population-based survival analysis for patients undergoing curative resection for rectal, sigmoid, and rectosigmoid cancers on the basis of the documented anatomical colorectal segment and stages over the last two decades.
Methods: Patients who underwent curative surgery for non-metastatic adenocarcinoma of the rectum, sigmoid, and rectosigmoid between 2000 and 2020 were identified using the Surveillance, Epidemiology, and End Results (SEER) database according to the International Classification of Diseases (ICD) coding system. Demographics, clinical and pathologic factors were compared for 3 different anatomical location, stages and time periods. Kaplan-Meier survival analysis was conducted for each location and stages, and curves were compared with the log-rank test.
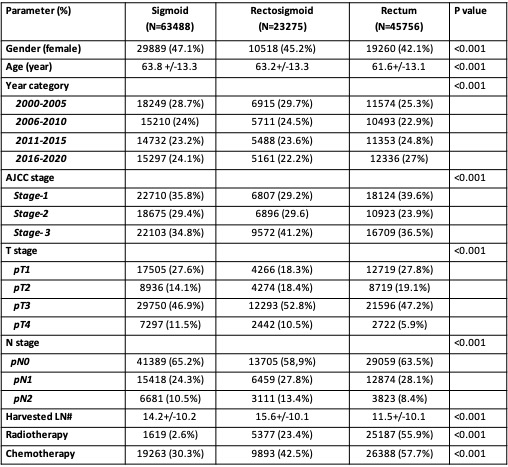
Results: A total of 132519 patients met the inclusion criteria and distribution of patients for each group is as follows: Rectum: 45756 (34.5%), Sigmoid colon:63488 (48%), and Rectosigmoid colon: 23275 (17.5%). The incidence of rectosigmoid colon cancer decreased throughout the study periods compared to rectum and sigmoid colon. Patients with sigmoid colon cancer were significantly older (63.8 +/-13.3) and more likely to be female [N=29889 (47.1%)] compared to the other sites (p< 0.001). Patients with rectosigmoid colon cancer were higher rates of advanced stage (stage-3: 42.1%), lymph node positivity (LN+) (41%) and pT3/4 stages (63%) compared to sigmoid colon (stage-3: 35%, LN+: 35%, pT3/4: 58%) and rectum (stage: 37%, LN+: 37%, pT3/4: 53%) (p< 0.001). Chemotherapy (CTx) and radiotherapy (RTx) rates were significantly higher in the rectum group (CTx: 57.7%, RTx: 55.9%) compared to the rectosigmoid (CTx: 43.5%, RTx: 23.4%) and sigmoid colon (CTx: 30.3%, RTx: 2.6%) (p< 0.001). During the study period, 10% improvement for stage-2 and 3 patients for each sites (p< 0.05). Multivariable (MV) cox regression analysis was performed to assess whether the factors independently affect long-term survival for the entire cohort. It was shown that gender (hazard ratio [HR]= 1.2, p< 0.001), primary cancer site (p< 0.001), year category (p< 0.001), age (HR= 1.06, p< 0.001), stage (p< 0.001), degree of differentiation (p< 0.001) and CT status (p< 0.001) were independently associated with worse survival. After MV analysis, rectum had worse overall survival rate than rectosigmoid and sigmoid colon.
Conclusion: This large population-based, comprehensive registry study demonstrates significant survival disparities between rectosigmoid and sigmoid colon cancer. Further studies defining distinct landmarks between rectal and colon cancers may improve best treatment approaches and improved cancer care and survival.