Background:
In recent years, colorectal surgery has witnessed significant advancements, yet a comprehensive understanding of resource utilization implications in emergency and elective settings remains limited. Therefore, this study aims to compare the impact of emergency and elective colectomies on healthcare resource utilization in patients with diverticular disease.
Methods:
This retrospective, multi-center analysis utilizes the TrinetX database and focuses explicitly on adult patients who underwent colectomy procedures between 2008 and 2018, resulting in 9,514 cases. These cases were categorized into two distinct groups: emergency colectomy cases (EM, n = 6,976) and elective colectomy cases (EL, n = 2,538). To ensure comparability, patients were matched for age, gender, and chronic comorbidities, including diabetes, hypertension, heart failure, and cirrhosis, resulting in a final cohort of 2,537 patients. These matched patients were then evaluated for outcomes for up to 5 years using a measure of association analysis and odds ratio.
Results:
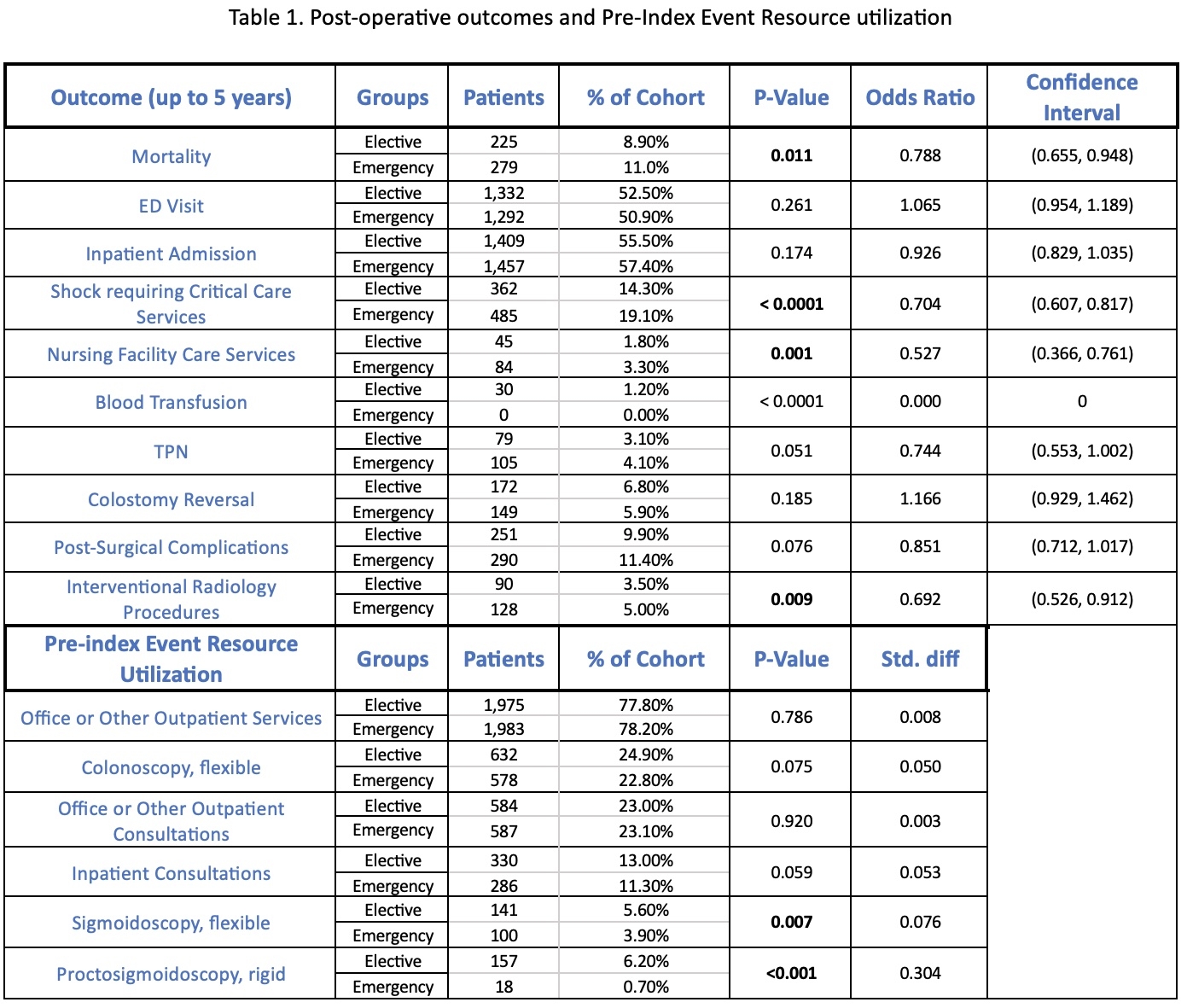
The analysis revealed a notable discrepancy in overall mortality rates, with a higher incidence observed in the emergency setting (EM) at 11.0% compared to elective cases (EL) at 8.90%. Moreover, EM patients exhibited a statistically significant increase in the incidence of shock requiring critical care services, utilization of nursing facility care services, and the need for interventional radiology procedures. Conversely, there were no statistically significant distinctions observed in emergency department (ED) visits, inpatient admissions utilization, colostomy reversals, or the incidence of post-surgical complications. Interestingly, EM patients displayed a diminished propensity to have undergone screening sigmoidoscopy or proctosigmoidoscopy within the year preceding the index event (for a comprehensive overview of outcomes, please refer to Table 1).
Conclusion:
Our findings underscore a disparity in healthcare resource utilization for patients undergoing colorectal surgery, particularly colectomies in emergency settings. Not only do these patients experience significantly higher mortality rates, but they also rely more extensively on hospital resources for up to 5 years compared to those in elective scenarios. This association is further linked to reduced use of outpatient screening prior to surgery among patients in the emergency setting. A more comprehensive understanding of pre-index event care may reveal potential avenues to mitigate resource utilization challenges for patients presenting emergently with diverticular disease.