Introduction: Postoperative opioid use has demonstrated increased length of stay, readmission, mortality, and hospital costs, thus identifying techniques for reducing postoperative pain is critical for improving outcomes. Minimally invasive surgery is accepted as having many advantages over an open approach, yet there is considerably less evidence comparing robotic surgery vs. laparoscopy. Specifically, data comparing pain and opioid requirements in patients undergoing these two types of minimally invasive surgery are lacking. Here, we compare postoperative pain scores and opioid requirements in patients who underwent colorectal resections by the laparoscopic versus the robotic approach, using a rigorous matching protocol.
Methods: We performed a retrospective study of patients who underwent robotic versus laparoscopic colorectal resections in our health system from 2018-22, excluding emergent or open cases. The outcomes of interest were postoperative average pain scores, up to postoperative day 5, as obtained by routine nursing care, and opioid requirements, reported as morphine milligram equivalent (MME). Power calculations were performed to ensure an ideal sample size was obtained. Categorical variables were compared using the chi-square test. Continuous variables were measured at 5 time points from baseline between the groups. The daily pain scores and MME were used as outcomes in separate linear mixed effect models with unstructured covariance between time points. Propensity score weighting was used to adjust for potential group imbalances. A p-value less than 0.05 was considered statistically significant.
Results: A total of 578 patients were included, with 367 patients in the laparoscopic (L) arm and 211 patients in the robotic (R) arm. The laparoscopic group had a higher proportion of patients with inflammatory bowel disease (IBD) (L 37% vs R 4%, P<0.001), extracorporeal anastomosis (L 57% vs R 42%, P<0.001), and intraoperative drain placement (L 53% vs R 31%, P<0.001). There was no difference between the groups with regards to acetaminophen or ketorolac use on all postoperative days (POD), length of stay, or adverse events. When adjusted for preoperative covariates including age, sex, BMI, history of IBD, history of chronic pain, procedure type, type of anastomosis, nonopioid pain medication use, and presence of drain, patients in the robotic arm had lower average pain scores on POD 0-5 (P=0.02) and significantly less opioid requirements on POD 0-5 (P=0.004) (Figure 1 and 2).
Conclusion: The robotic platform offers the benefit of decreased pain and reduced opioid requirements postoperatively when compared to laparoscopy for colorectal surgery. Benefits of postoperative recovery should be heavily weighed when considering a surgical approach for patients who require colorectal resections for a wide range of pathologies.
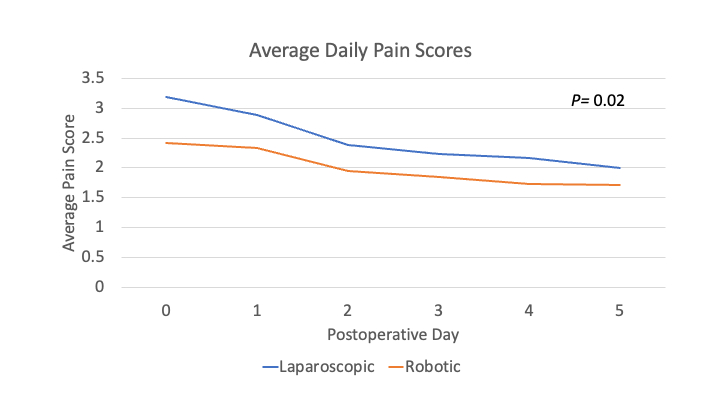
Figure 1: Average daily pain scores reported for postoperative days 0-5 between patients who underwent laparoscopic vs robotic colorectal resections.
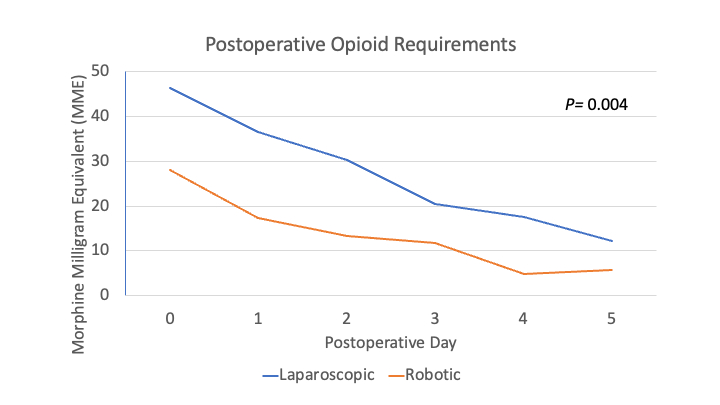
Figure 2: Daily opioid requirements, as measured by morphine milligram equivalents, for postoperative days 0-5 between patients who underwent laparoscopic vs robotic colorectal resections.