Introduction
Chronic inflammation, as is typically found in ulcerative colitis (UC), can predispose to worse surgical outcomes than for conditions like cancer or familial adenomatous polyposis. We sought to investigate the differences between UC patients undergoing ileo-anal pouch anastomosis (IPAA) and those undergoing the same procedure for other indications.
Methods
All patients undergoing a one-stage IPAA operation between 2006-2020 were identified from the National Surgical Quality Improvement Program database. Patients were divided into two groups based on their underlying diagnosis: UC and Other. The groups were compared for their preoperative characteristics as well as intraoperative and postoperative outcomes. Multivariate regressions were performed to find predictors of reoperation, readmission, death, and length of stay (LOS).
Results
There were 3901 UC and 2577 Other patients. Other indications included cancer (45%), benign neoplasm (25%), Crohn’s disease (6%), diverticulitis (3%), and functional disorder (5%).
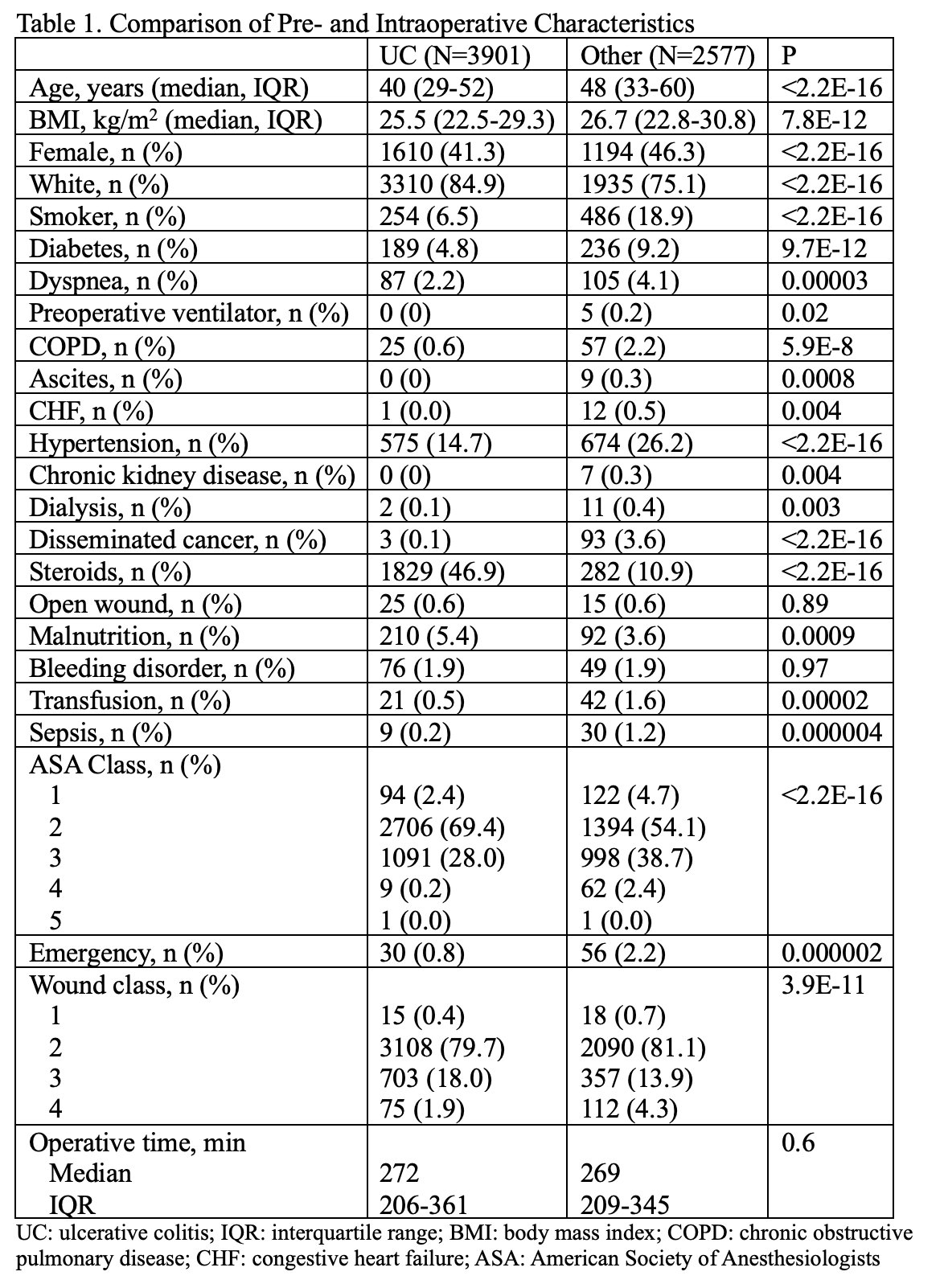
UC patients were significantly younger (median age 40 years [interquartile range, IQR 29-52] vs 48 [IQR 33-60], P<0.001), had lower BMI (25.5 vs 26.7 kg/m2, P<0.001) with more males (59 vs 54%, P<0.001). Significantly more UC were white (85 vs 75%, P<0.001).
Fewer UC patients had smoking history, diabetes, dyspnea, chronic obstructive pulmonary disease, hypertension, or disseminated cancer but were more likely to be on steroids (47 vs 11%, P<0.001) and be malnourished (5.4 vs 3.6%, P<0.001). UC was more likely to be American Society of Anesthesiologists class 1 or 2 (72 vs 59%, P<0.001). UC was less likely to undergo surgery for emergent indications (0.8 vs 2.2%, P<0.001) and more likely to have contaminated or dirty wounds (20 vs 18%, P<0.001). Operative time did not differ significantly between the two groups, with median being 269 minutes for UC (IQR 209-345) and 272 for Other (IQR 206-361, P=0.6).
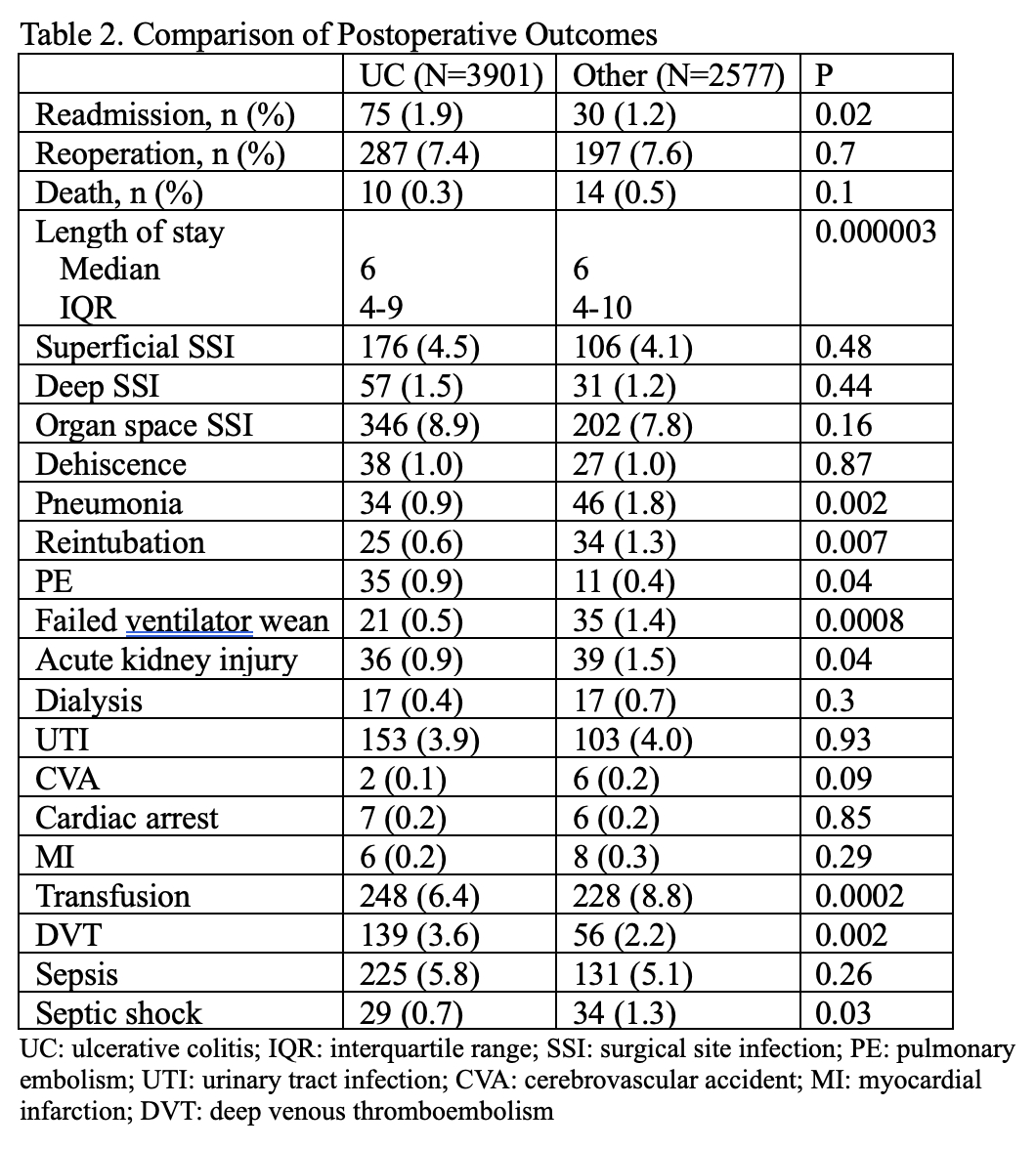
After surgery, UC had shorter LOS by almost a full day (mean 7.6 vs 8.4 days, P<0.0001). UC had slightly higher rates of readmission (1.9 vs 1.2%, P=0.02) but reoperation (7.4 for UC vs 7.6% for Other, P=0.7) and death (0.3 vs 0.5%, P=0.1) were comparable between the two groups on univariate analysis. UC had higher rates of postoperative deep venous thromboses (3.6 vs 2.2%, P=0.002) but lower pneumonia, reintubation, septic shock, and transfusion. On multivariate analysis, UC was a predictive factor for readmission (ß=0.55, 95% CI 0.1-1.0), but not for reoperation, death, or LOS.
Conclusion
Patients with UC tend to undergo restorative proctocolectomy with IPAA at a younger age than for other indication, with comparable or lower rates of complications. However, they have a higher likelihood of readmission despite being younger and healthier at baseline; this should be taken into consideration during preoperative planning and counseling.