Introduction:
Chest tubes are common procedures, especially in critical care. Typically, these procedures are relatively safe when proper landmark identification is coupled with ultrasound guidance. However, if placed without confirmation of the correct location, the procedure can easily become dangerous, particularly if inserted into the abdominal cavity. This case represents the first recorded instance in the literature where a chest tube entered the liver parenchyma and the resulting portal vasculature, coursing intraluminally through the inferior vena cava, with the distal end ultimately lodging within the atriocaval junction in the right atrium.
Description of the Case:
The patient was a 75-year-old female admitted to the cardiovascular intensive care unit for fluid overload and resultant dyspnea in the setting of congestive heart failure. Cross-sectional imaging revealed a right-sided pleural effusion.
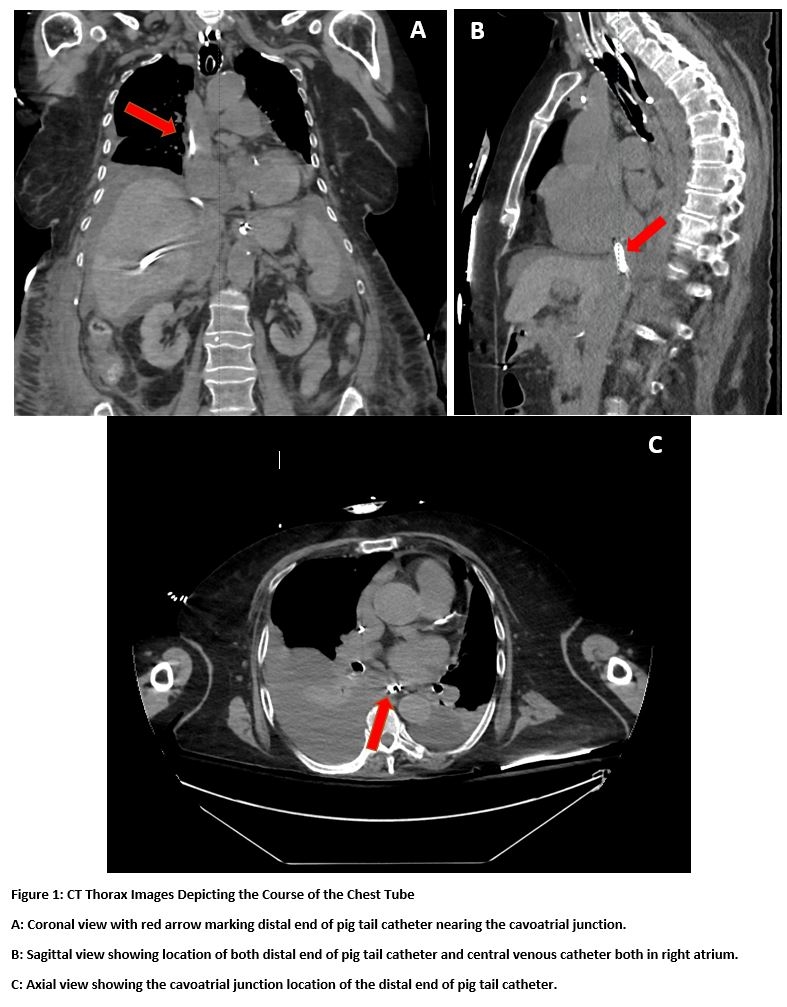
During the placement of a pigtail chest tube, landmark guidance was utilized; however, ultrasound confirmation of the correct location was not performed. The chest tube was inserted, resulting in an immediate return of frank blood, initially thought to indicate a hemothorax. The patient promptly became hypotensive upon transitioning to gravity suction. A bedside radiograph was conducted, revealing penetration into the liver parenchyma. Cross-sectional imaging unveiled the distal end of the chest tube at the atriocaval junction.
Cardiothoracic, trauma, and abdominal transplant surgery were consulted. A specific strategy for removal was determined after a literature review indicated that previous cases were successfully managed with the gradual extraction.
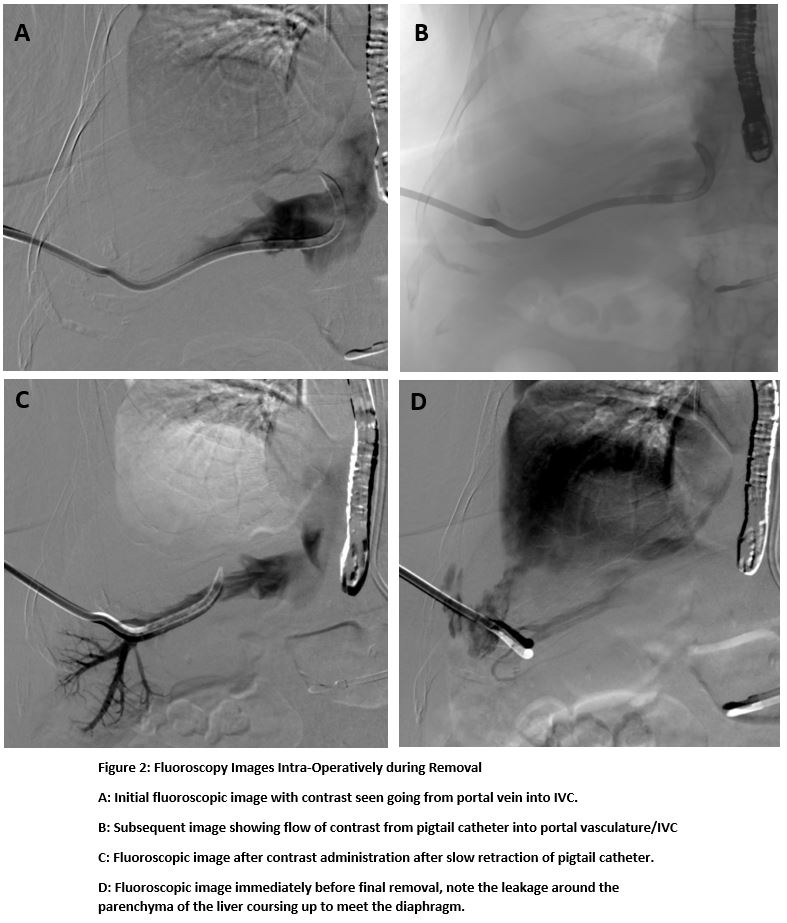
The patient was taken to the operating room, where the pigtail catheter was retracted under fluoroscopy. Multiple contrast administrations were introduced through the chest tube intra-procedurally to assess not only for intrahepatic vasculature damage but also to ensure that the tube had not penetrated the atriocaval junction into the pericardial space. The procedure was well tolerated with the chest tube being successfully removed with no immediate complications.
Discussion:
Intrahepatic chest tube placement is an exceedingly rare complication. A literature review conducted to date has uncovered only five previously documented cases. Management for these past episodes has predominantly involved conservative therapy, with some cases requiring coil embolization of the liver parenchyma.
Instances such as the one detailed in this case underscore the critical importance of ensuring proper positioning before engaging in invasive procedures. Additionally, we posit that this case serves as a compelling demonstration of the significance of literature review when dealing with rare complications. Insights gained from prior successes or failures can offer valuable guidance in managing such uncommon situations.