Background: Pneumocystis Jirovecii (PJ) is an opportunistic fungus that usually causes pneumocystis pneumonia (PCP) in immunocompromised patients such as patients with human immunodeficiency virus (HIV) infection, hematological malignancies, and organ transplant recipients. Extrapulmonary PJ infection is exceedingly rare. The commonly reported sites of the extrapulmonary disease are spleen, lymph nodes, kidneys, and eyes. Immune reconstitution inflammatory syndrome (IRIS) is defined as the paradoxical worsening of a preexisting infection following the initiation of antiretroviral therapy (ART) in patients with HIV infection. We present a case of IRIS secondary to PJ presenting as recurrent small bowel obstruction in a newly diagnosed HIV patient treated with ART.
Case: A 71-year-old lady with past medical history of hypothyroidism and adrenal insufficiency presented with a 4-month history of gradual cognitive decline. Work-up revealed an incidental finding of HIV infection with a viral load of more than 2,000,000 copies/mL and a CD4 count of 24/microL. She was diagnosed with HIV/AIDS-associated encephalopathy and discharged on ART (bictegravir, emtricitabine & tenofovir alafenamide) and trimethoprim-sulfamethoxazole prophylaxis. Three weeks later, the patient presented with nausea, vomiting, and abdominal pain. Upper endoscopy revealed signs of gastritis. The patient was discharged on pantoprazole 40mg. Two days later, the patient presented with similar symptoms. A CT abdomen and pelvis scan showed partial small bowel obstruction (SBO) with a transition point in mid-jejunum. The patient was treated conservatively with significant improvement and was discharged home. Two days later, she presented again with vomiting and crampy abdominal pain. A repeat CT scan of the abdomen and pelvis revealed recurrent SBO (Figure. 1). The patient did not have any apparent risk factors for SBO. This time, the patient had a laparoscopy with subsequent laparotomy which revealed an area of small bowel narrowing with inflammation and a mass in the surrounding mesentery. GMS staining of the resected small bowel and mesenteric lymph nodes showed presence of organisms morphologically consistent with PJ (Figure. 2). The specimen was sent for PCR which confirmed the diagnosis. The patientís history of recent ART initiation, improving CD4 count, significant reduction of viral load to 2,000 copies/mL, SBO, and a tissue diagnosis of PJ were consistent with the diagnosis of IRIS. The patient was treated with high doses of trimethoprim/sulfamethoxazole and prednisone with significant improvement.
Discussion: Extrapulmonary PJ is exceedingly rare. To our knowledge, this is the first reported case of PJ presenting as IRIS in the small bowel. In the setting of recent initiation of ART, new symptoms and signs should always prompt the consideration of IRIS.
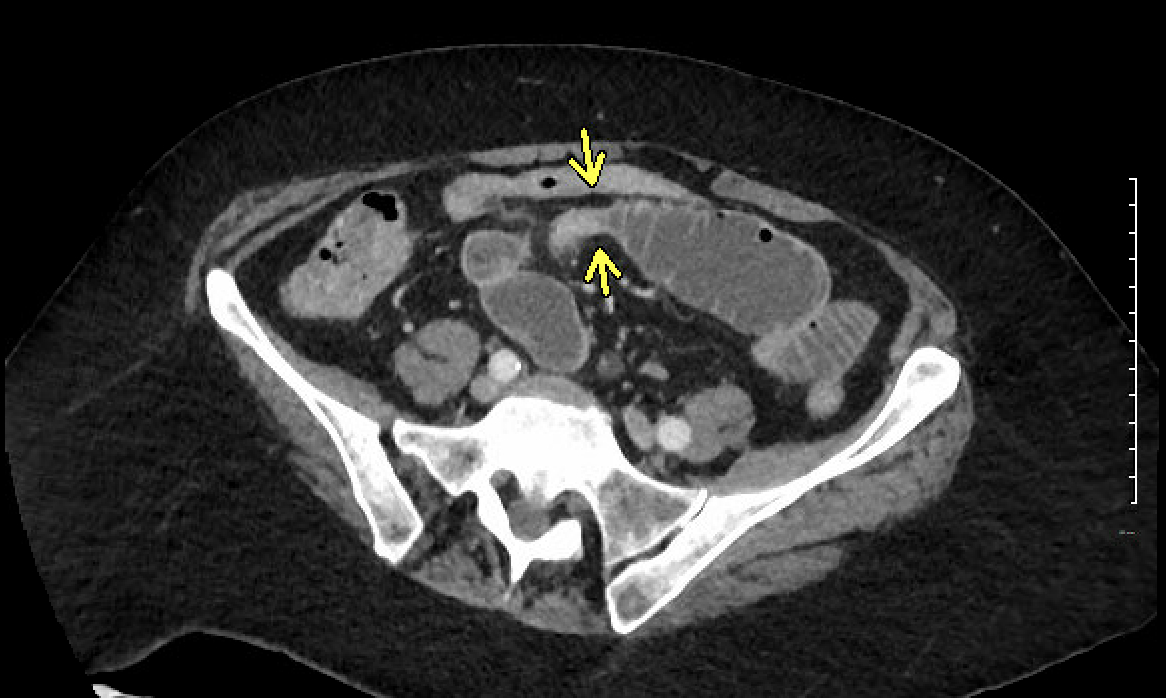
Figure.1 : Dilated small bowel loop with an abrupt transition point.
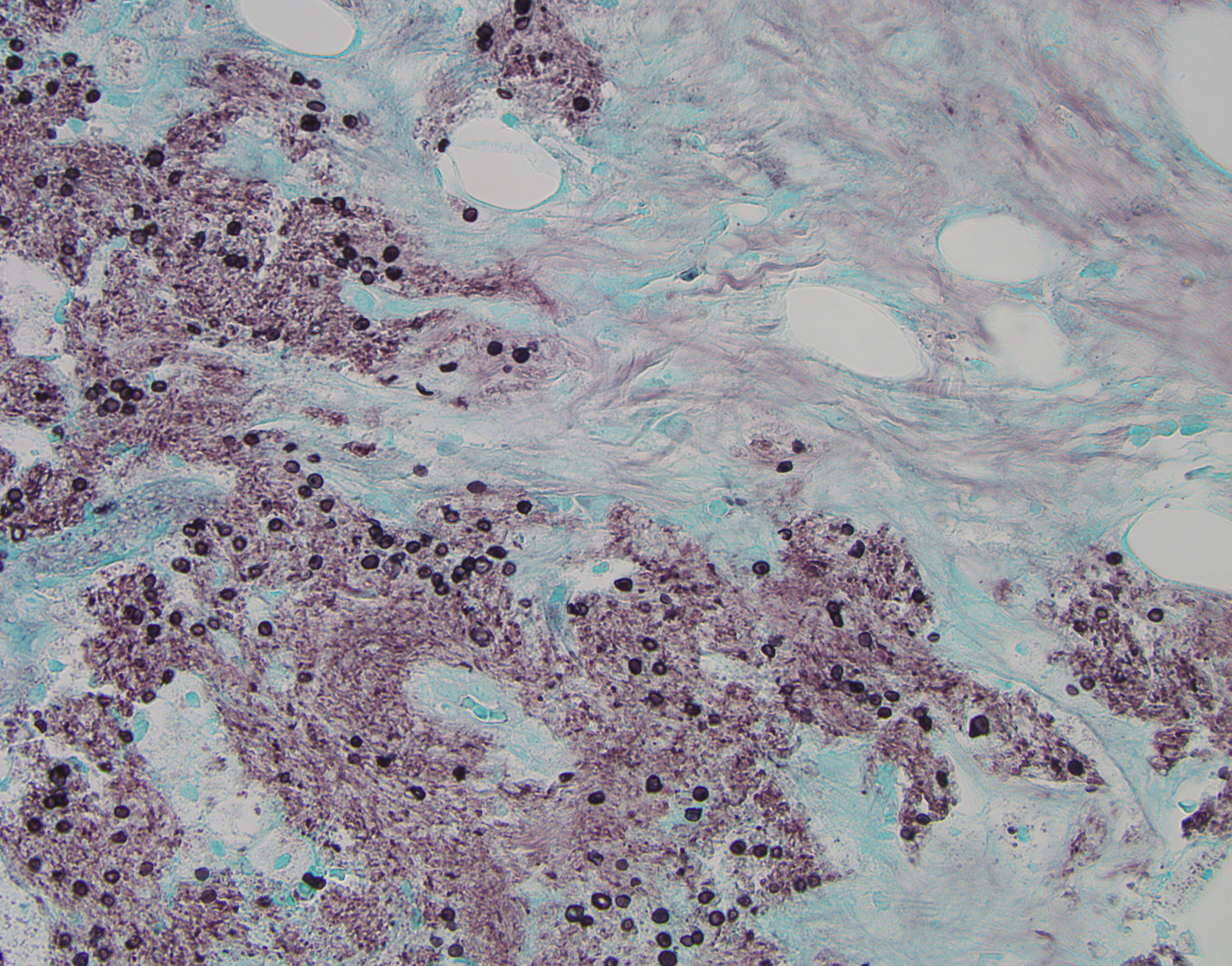
Figure. 2 : GMS stain showing multiple yeast-like organisms with round to oval shaped cysts morphologically consistent with pneumocystis Jirovecci