Introduction:
Frequently regarded as an “abdominal cocoon”, encapsulating peritoneal sclerosis (EPS) is a rare inflammatory condition of the peritoneum. EPS is marked by a fibrocollagenous membrane that encases the small intestine, causing recurrent small bowel obstructions. Although commonly linked to long-term peritoneal dialysis, medications, autoimmune conditions, ovarian disorders, and infections such as abdominal tuberculosis have also been identified as culprits. Notably, many cases are idiopathic. Diagnosis is based on clinical features and is confirmed by radiography or laparotomy. Patients with mild symptoms are managed conservatively, while those with evidence of intestinal obstruction require surgical intervention including membrane excision, adhesiolysis, and, in some cases, bowel resection.
Case:
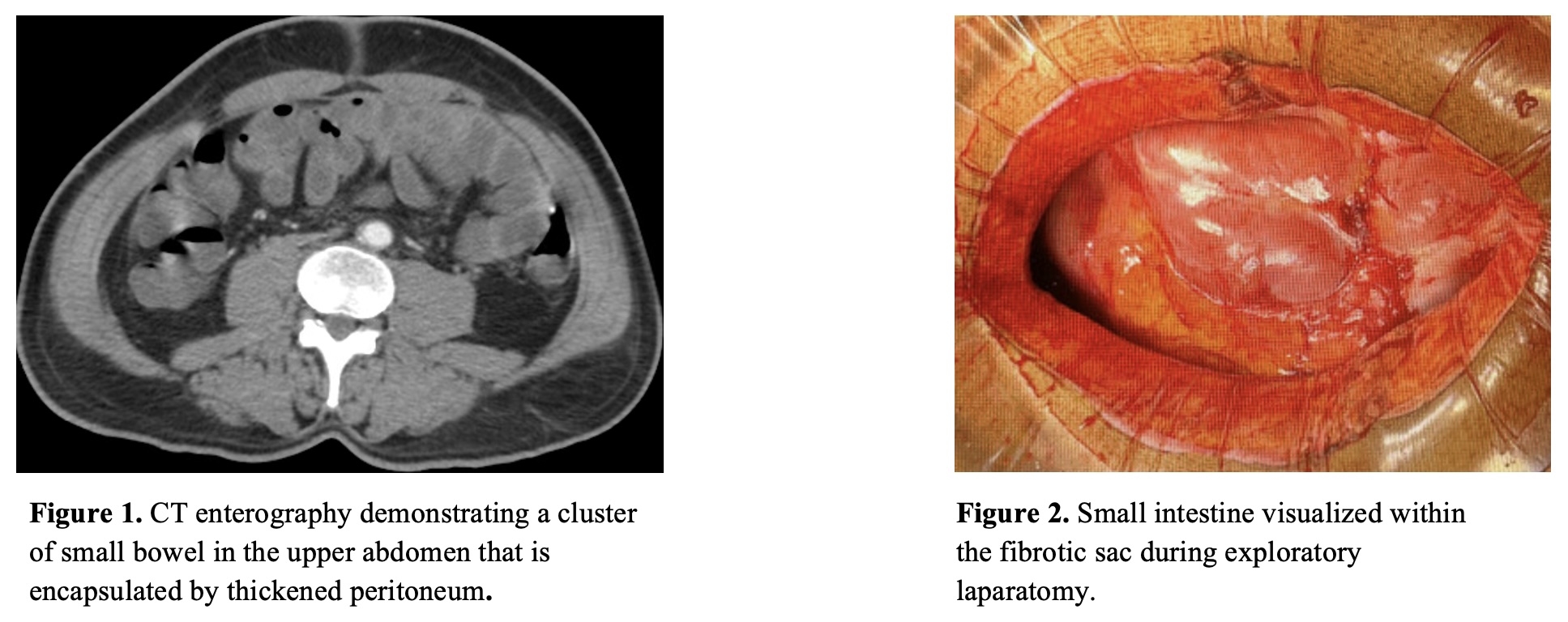
A 51 year-old male with a history of hypertension, type 2 diabetes, and hypothyroidism presented with three months of decreased appetite, nausea, vomiting, constipation, and unintentional weight loss. Physical exam was notable for left lower quadrant abdominal tenderness without rebound or guarding. CT abdomen and pelvis demonstrated gastric and proximal small bowel dilation without a discrete transition point as well as a cluster of bowel within the upper abdomen. Due to concern for partial small bowel obstruction, a nasogastric tube was placed with mild symptomatic improvement. Total parenteral nutrition was also initiated due to concern for malnutrition. CT enterography subsequently demonstrated persistent clustering of bowel in the upper abdomen encapsulated by thickened peritoneum (Figure 1). Since he did not have a history of peritoneal dialysis, the initial differential included autoimmune and infectious etiologies. However, infectious workup, including two consecutive quantiferon tuberculosis assays, and autoimmune workup were negative. A diagnostic laparoscopy with peritoneal biopsy revealed fibroconnective tissue with chronic inflammation and dense fibrosis. An exploratory laparotomy was then pursued for worsening nausea and abdominal pain. The dense sac overlying the small bowel was released via adhesiolysis (Figure 2). One week postoperatively, he was able to tolerate a low residue diet with return of bowel function. During follow-up three months later, he expressed continued improvement and resolution of symptoms.
Discussion:
This was a case of idiopathic EPS leading to small bowel obstruction that was managed with adhesiolysis of the encapsulating peritoneal sac. Since idiopathic EPS is rare and not associated with other conditions, clinicians must maintain a high index of suspicion when patients without a history of surgery or hernias present with features of intractable abdominal pain, weight loss, constipation, and poor oral intake. A thorough history should be obtained to identify patients with established risk factors.