Introduction:
The Health Insurance Marketplace was initiated on October 1, 2013, as part of the Affordable Care Act (ACA) implementation. Research on ACA coverage expansion and cancer care has focused mainly on dependent coverage expansion (DCE) and Medicaid expansion. Our aim was to evaluate whether the ACA marketplace affected surgical outcomes in patients with gastrointestinal (GI) cancer and whether its impact was moderated by race.
Methods:
Patients diagnosed with 12 GI cancers from 2011-2017 in the National Cancer Database were categorized into three groups: before the ACA marketplace (2011-2012, period 1), immediately after inception (2014-2015, period 2), and two years afterwards (2016-2017, period 3). Our main outcomes were focused on the oncologic standard of care, as defined by negative resection margin, adequate lymphadenectomy, and receipt of indicated adjuvant chemotherapy and/or radiotherapy.
Results:
Across the three time periods, 147,891 patient records were available to evaluate margin status and adjuvant therapy, while 121,734 patient records were available for adequate lymphadenectomy analyses. Compared to before the ACA marketplace inception, uninsured patients decreased from 2.8% in 2011-12 to 1.6% in 2016-17 (p < 0.001). There were fewer patients diagnosed with Stage 4 cancer after the ACA marketplace versus before (7.3% vs. 10.2%, p < 0.001).
On multivariate analysis, Black and Asian patients were less likely to have negative margins in period 1 as compared to period 2 (OR 0.79, [95% CI 0.69-0.91]), whereas White patients were more likely to have negative margins in period 3 as compared to period 2 (OR 1.18, [95% CI 1.11-1.126]). With regards to adequate lymphadenectomy, Asian patients were more likely to have an inadequate lymphadenectomy in period 1 as compared to period 2 (OR 1.35, [95% CI 1.14-1.60]). Hispanic patients also saw decreased inadequate lymphadenectomies, but only in period 3 (OR 0.88, [95% CI 0.78-0.99]). Both White and Black patients saw reductions in inadequacy of lymphadenectomy over time, likely related to improved quality of care.
Surgery for pancreas (OR 0.80, [95% CI, 0.67-0.97]) and peritoneal (OR 0.50, [95% CI, 0.34-0.71]) cancers were less likely to have negative margins in period 1 as compared to period 2, while anal cancer (OR 0.78, [95% CI, 0.62-0.97]) had decreased inadequate lymphadenectomy in period 3. Patients with esophagus (OR 0.63, [95% CI, 0.45-0.90]), bile duct (OR 0.77, [95% CI 0.62-0.96]), and pancreatic (OR 0.81, [95% CI, 0.67-0.97]) cancers were less likely to receive adjuvant therapy in period 1 as compared to period 2.
Conclusions:
The ACA marketplace had an impact on cancer outcomes in GI cancer patients treated by surgery, some of which varied based on race/ethnicity. Further studies are warranted to understand why the marketplace had these effects.
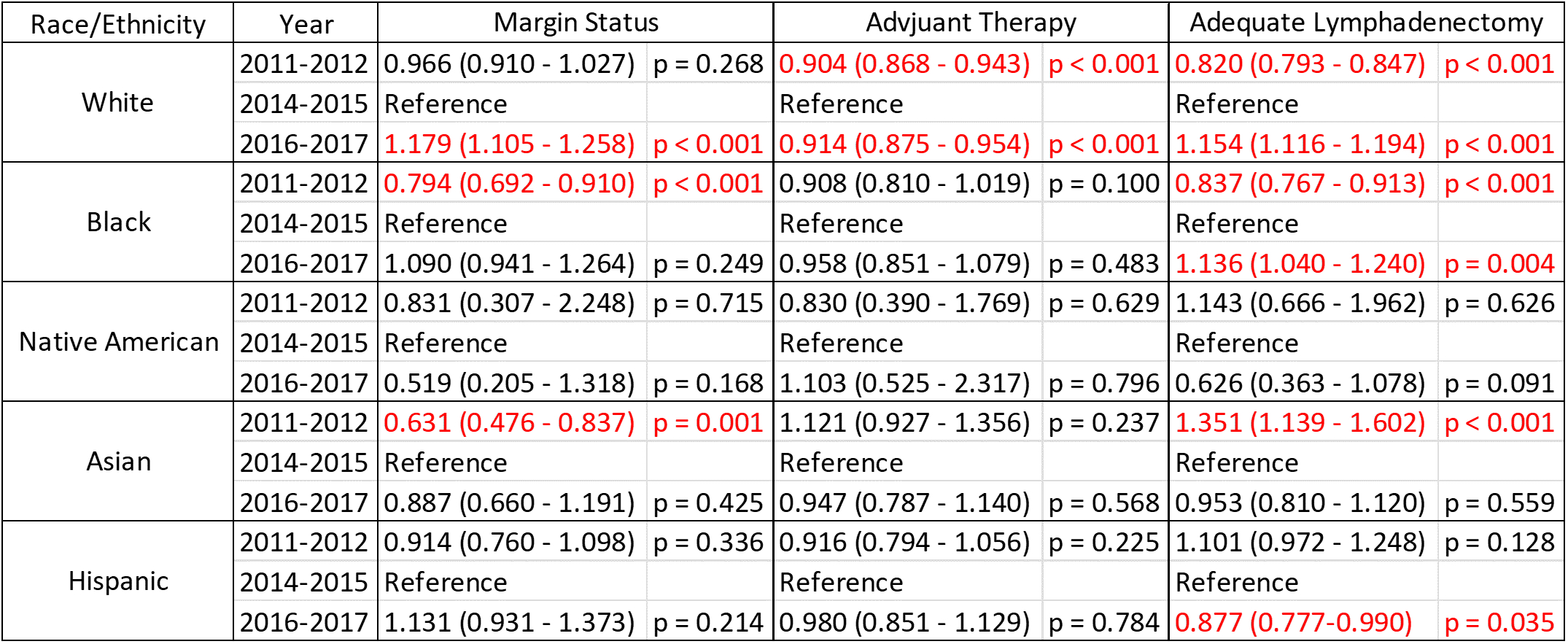
Table 1: Surgical oncology outcomes before and after the ACA Marketplace by race/ethnicity
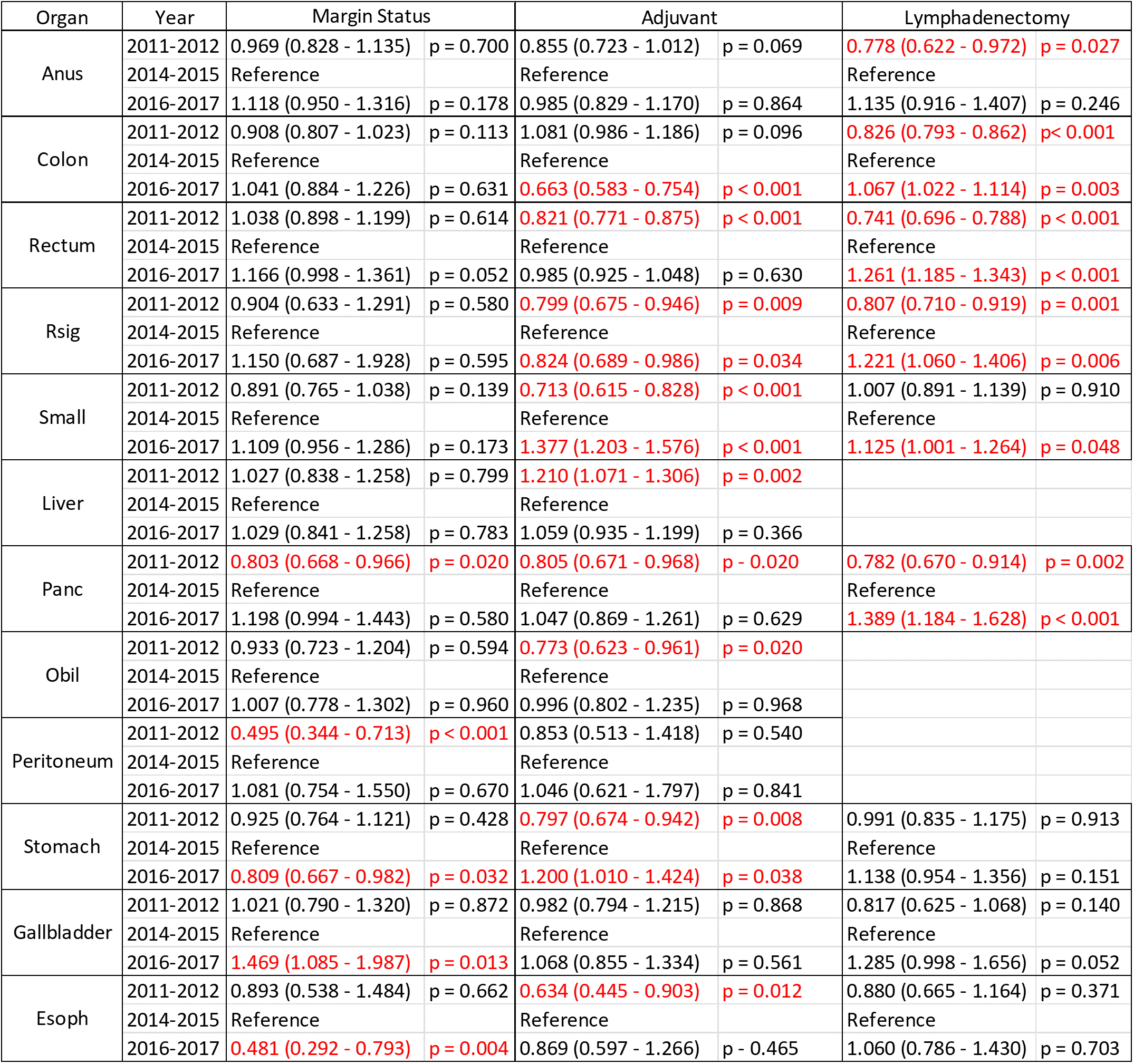
Table 2: Surgical oncology outcomes before and after the ACA Marketplace by primary organ site