Introduction: 1.2 million cholecystectomies are performed every year in the USA, and over 90% are performed laparoscopically. While laparoscopy proffers faster recovery times, risk of post-operative bile leaks is up to 3 times higher than for open procedures. We aim to define factors affecting value (quality/cost) and predict outcomes for this service line in our Health System Network.
Methods: Clinical variables from patients (>18 y/o) were retrieved from a Health System Warehouse from Jan-2010 to Dec-2021, under IRB-approved protocols. Quality domains (Observed/Expected) assessed on post-operative complications (PC standardized by grading system), length of stay (LOS in days), 30-day readmission (RA), net promoter score as surrogate for patient satisfaction (PS), and textbook cases (TB). Total charges (TC) and reimbursement index (RI, O/E) were included as surrogates for cost. Diagnosis for common bile duct injury (CBDI) and bile leak (BL) were documented. Symptomatology at presentation was recorded for vomiting, fever, abdominal pain, and diarrhea at one health center (MC2). Modeling for univariate and multivariate analyses were conducted in SPSS.
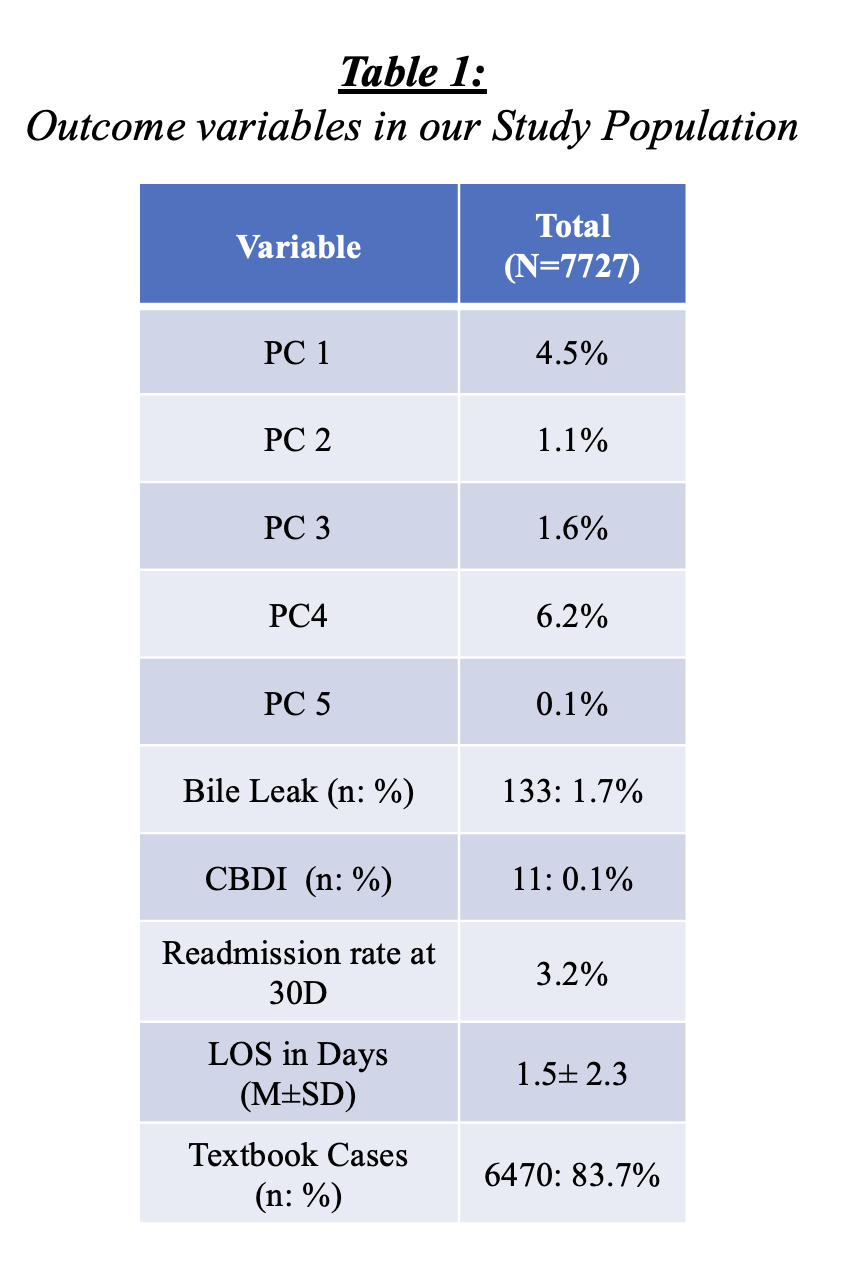
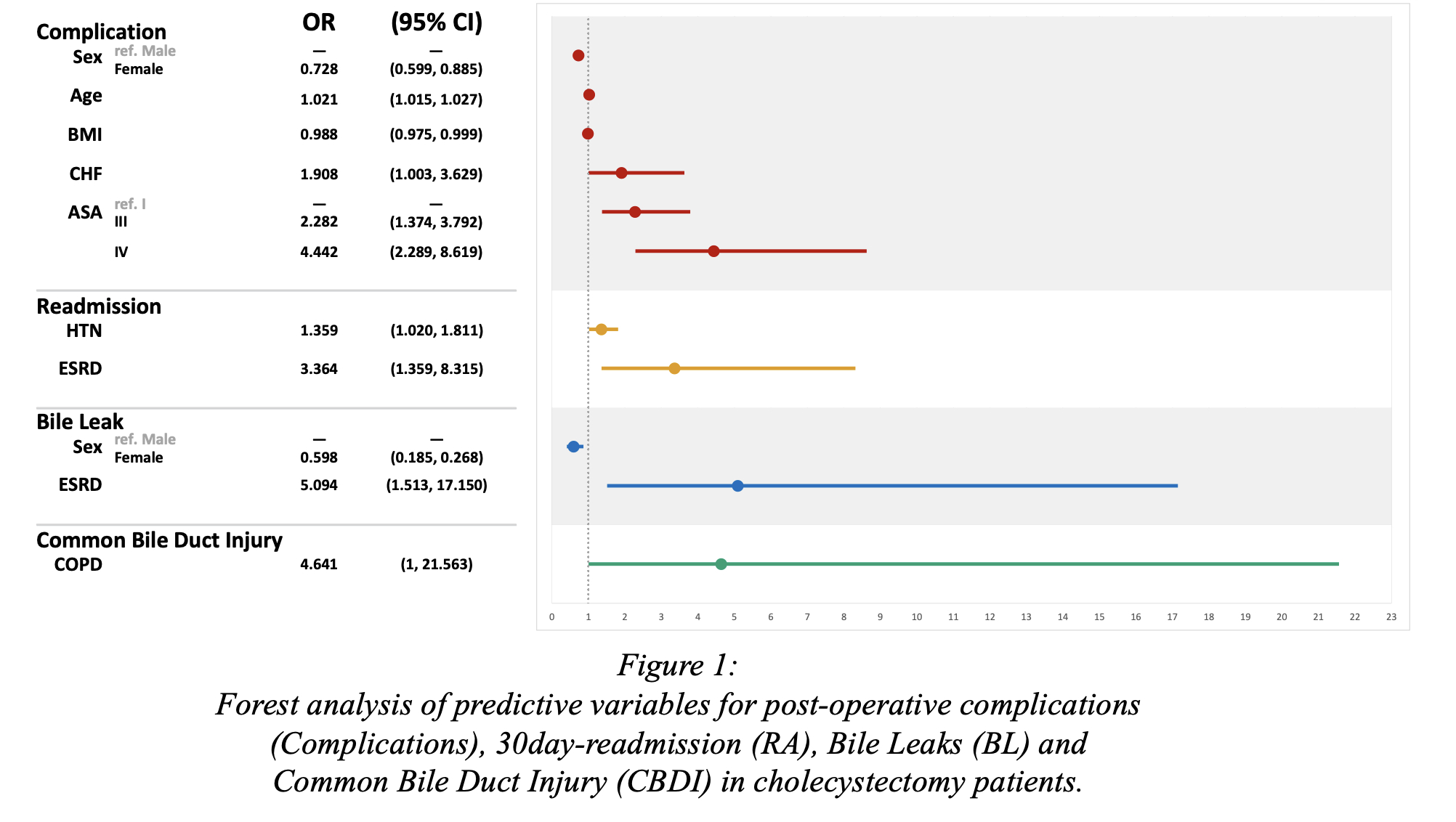
Results: 7727 patient underwent cholecystectomies, 97.4% were minimally invasive (MI), with a mean age and BMI of 44.5 ±16.3 years and 29.7±9.5 kg/m2, respectively. The male-to-female ration was 1:2. Outcome variables in our study population can be found in table 1. At MC1 (n=3585) 67.6% of cholecystectomies were outpatient procedures. MI procedures showed a lower incidence of bile leaks (1.2 vs 1.9%), CBD injuries (0.2 vs 0.6%), and lower PC (p=0.01) when compared to Open. At MC2 (n=4142) 86% of cholecystectomies were outpatient procedures. MI procedures showed a higher incidence of bile leaks (2.2 vs 0.0%), CBD injuries (0.1 vs 0.0%) and lower PC (p=0.01) than Open. Symptomatology at presentation was documented for MC2 with 98% of patients complaining from abdominal pain, 32.4% with vomiting, 9.8% with diarrhea, and 6.3% with a fever. In multivariate analysis age, BMI, CHF, and ASA >3 were predictive variables for PC, whereas HTN and ESRD were risk factors for RA (Forest analysis of predictive variables for PC, RA, BL and CBDI figure 1).
Conclusion: Cholecystectomies showed a high value as a service line in our Health Network with a low rate of bile leaks.