BACKGROUND: Surgery for pancreatic cancer is associated with high morbidity and mortality. Utilizing prediction models may help minimize post-operative complications. Pre-operative frailty scores are one such model useful in predicting surgical outcomes. We investigated the impact of surgery and the factors contributing to post-operative frailty (POF) in pancreatic adenocarcinoma patients.
STUDY DESIGN: Patients >65 years-old undergoing surgical resection for pancreatic adenocarcinoma in SEER-Medicare (2008-2015) were classified with a pre- and post-surgery (12 months prior to and after surgery, respectively) claims-based frailty index status (non-frail <0.10, prefrail 0.10-0.19, mildly frail 0.20-0.29, moderately frail 0.30-0.39, and severely frail ?0.40). Pre- and post-surgery frailty status was used to categorize patients as having increased POF or no increased in POF (no change or decrease). Baseline characteristics were analyzed utilizing chi-square analysis. Multivariate logistic regression was used to assess odds ratios for increased frailty.
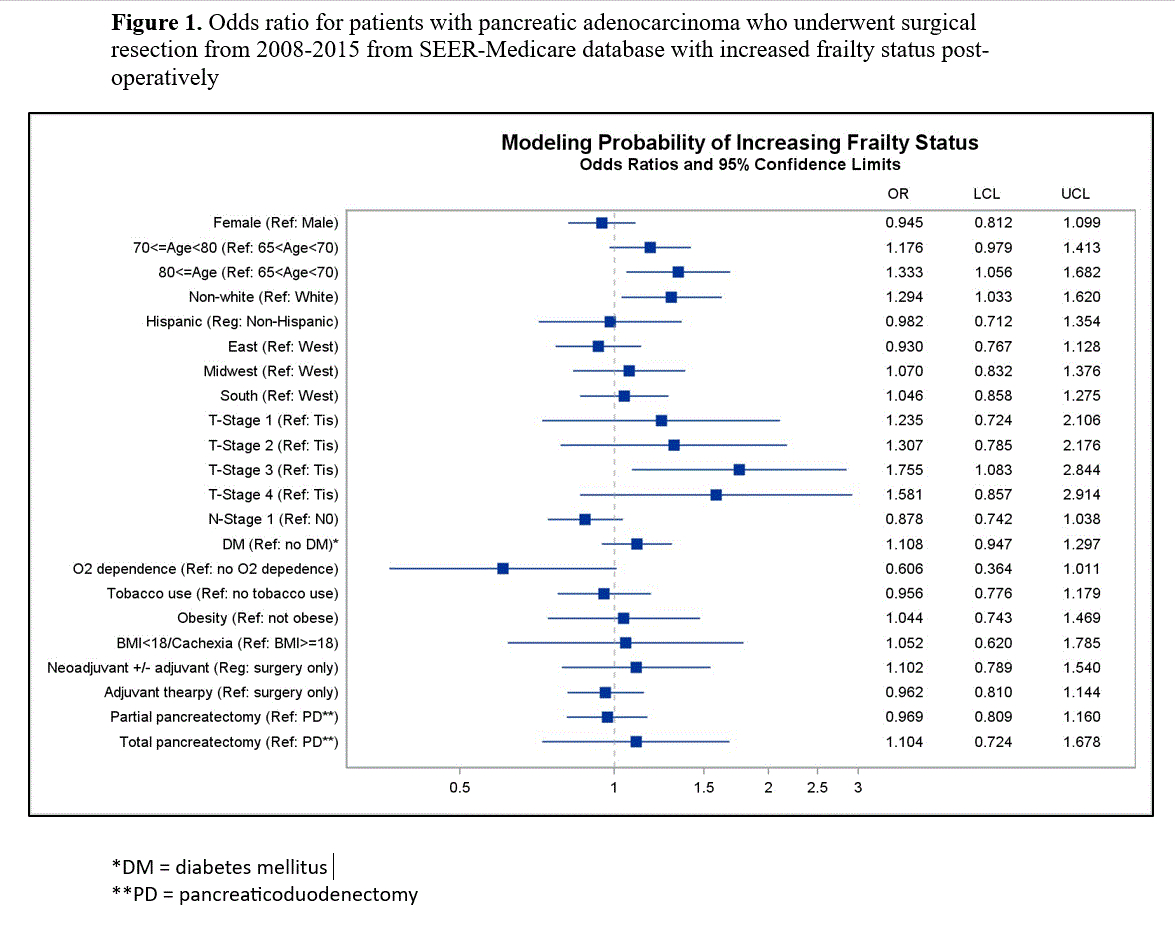
RESULTS: 2,855 patients were identified of which 1,273 (44.6%) patients had an increase in POF. Increased POF was more commonly seen in elderly patients (?80 years-old (21.2% vs 18.5%; p=0.0518)), patients who were non-white (14.4% vs 11.5%; p=0.0224) and those located in a metro-region (89.3% vs 85.5%; p=0.0022) compared to patients with no increase in POF. Patients with higher T stage also had increased POF (T3: 76.3%, Other Tstages: 23.7% vs. T3: 71.5% Other Tstages: 28.5%; p=0.0345) compared to no increase in POF. These findings persisted on multivariate analysis: ?80 years-old (OR 1.333; 95% CI 1.056-1.682), non-White (OR 1.294; 95% CI 1.033-1.620), and T-stage 3 (OR 1.755; 95% CI 1.084-2.844). No significant difference was seen in POF for variables of sex, Hispanic ethnicity, region or poverty level. We also found no correlation in POF with N-stage, diabetes, oxygen dependence, tobacco use, obesity, cachexia, neo/adjuvant therapy, or extent of pancreatic resection.
CONCLUSION: Increase POF was associated with elderly patients, non-white patients and those with higher T-stage, but was not affected by neoadjuvant or adjuvant therapy, type of surgery performed, significant comorbidities, gender or ethnicity. Further quantifying and validating post-operative frailty could prove useful as an index of assessment for patients undergoing curative surgery for pancreatic adenocarcinoma, and may extend to other cancers.