Introduction: Patients undergoing oncologic surgical procedures may have a higher incidence of deep venous thrombosis (DVT) in the peri-operative period. We sought to assess healthcare utilization and expenditures among gastrointestinal (GI) cancer patients who developed DVT following a surgical procedure.
Methods: Patients who underwent surgery for esophageal, gastric, hepatic, biliary duct, pancreatic, and colorectal cancer between 2013 and 2020 were identified from the IBM Marketscan database. Generalized linear models were used to compare pharmacy and one-year post-discharge costs among patients who did and did not develop a post-operative DVT.
Results: Among the 17,048 individuals included in the analytic cohort (esophagus: n=561, 3.3%; stomach: n=827, 4.9%; liver: n=432, 2.5%; bile duct: n=332, 1.9%; pancreas: n=1,211, 7.1%; colon n=10,130, 59.4%; rectum: n=3,555, 20.9%), median age was 55 years (IQR: 49 - 60) and approximately half were male (n=9,207, 54.0%). Most individuals were employed at the time of surgery (n=10,547, 61.9%) and resided in the South region of the U.S. (n=8,056, 47.3%). In the post-operative period, 3.4% (n=571) of patients developed a DVT (esophagus: n=9, 1.6%; stomach: n=17, 3.0%; liver: n=17, 3.0%; bile duct: n=18, 3.1; pancreas: n=69, 12.1%; colon n=346, 60.5%; rectum: n=96, 26.8%). Patients with a higher Charlson Comorbidity Index score (CCI ?2; DVT: 16.8% vs. no DVT: 9.5%), as well as patients with a diagnosis of hepatic (DVT: 3.0% vs. no DVT: 2.5%) or pancreatic (DVT: 12.1% vs. no DVT: 6.9%) cancer were more likely to develop DVT (all p<0.001). On multivariable regression, patients who developed a DVT had higher odds of extended length-of-stay (OR 1.59, 95%CI 1.32-1.92), 30-day readmission (OR 2.70, 95%CI 2.20-3.30), and an emergency department visit (OR 2.00, 95%CI 1.69-2.38) (all p<0.001). Moreover, patients who developed a DVT had higher median outpatient pharmacy expenditures and total 1-year expenditures. Specifically, median outpatient pharmacy expenditures (DVT: ,555 [IQR: ,956-,479] vs. no DVT: ,780 [IQR: -,688]) and total 1-year expenditures (DVT: ,782 [IQR: ,323-,013] vs. no DVT: ,807 [IQR: ,060-,414]) were higher among patients who developed a DVT (p<0.001) (Figure).
Conclusion: DVT among patients with GI cancer was associated with worse postoperative outcomes and increased healthcare expenditures, which extended to the outpatient setting over the first-year post-discharge. These findings underscore the importance of prophylaxis, screening, and treatment of DVT to improve outcomes and reduce healthcare expenditures among GI surgical patients.
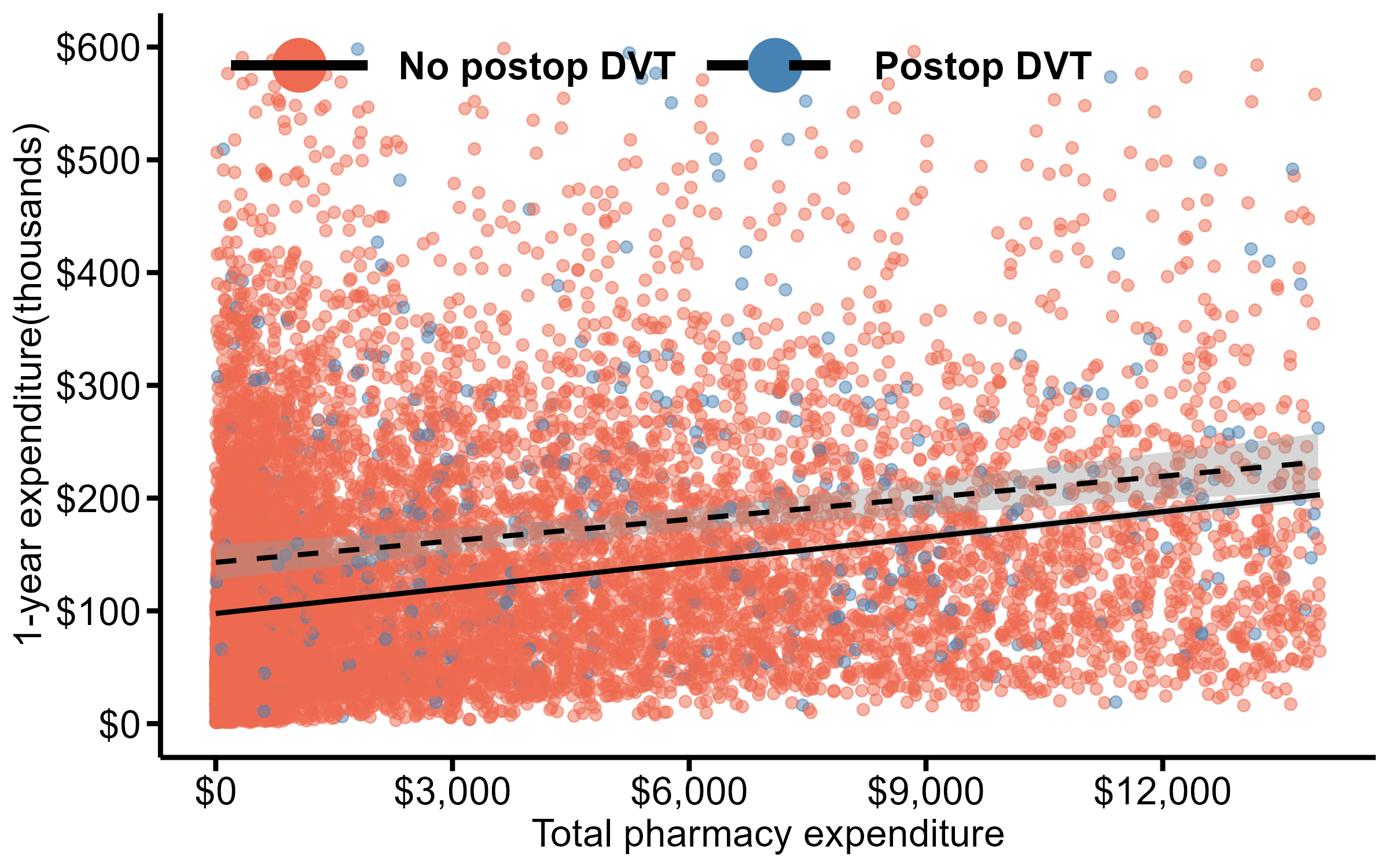
Scatter plot illustrating the association between the estimate of outpatient pharmacy costs and total 1-year expenditures in patients with and without deep vein thrombosis in the perioperative period.