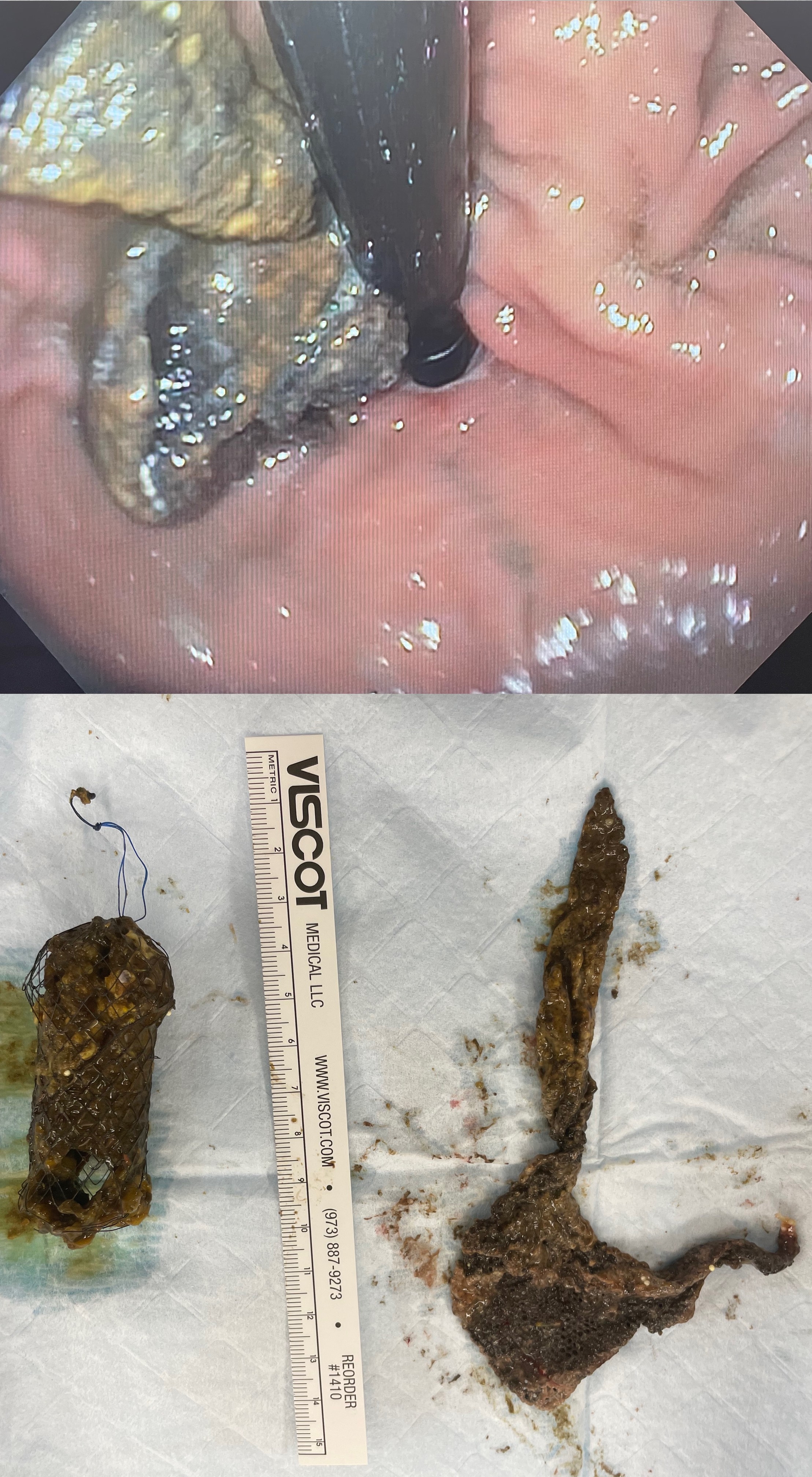
We present a case of a 67-year-old female patient who required urgent laparoscopic repair of an incarcerated hiatal hernia. The hernia promptly recurred, and she returned to the operating room the following day for re-operative repair. A non-absorbable mesh was used to reinforce the hiatal closure. Approximately six months after surgery, she developed progressive dysphagia and weight loss. An upper endoscopy was performed, and the mesh was seen eroding through the gastric cardia, creating a high-grade stricture at the gastroesophageal junction (GEJ). The mesh could not be extracted endoscopically due to adherence to the gastric wall, and therefore, a covered stent was positioned across the GE junction. Over the next three months, she was able to eat normally, gaining approximately 30 pounds. She was returned to the operating room with the plan to remove the stent and surgically remove the mesh, expecting the need to perform an esophagogastrectomy. After removing the stent, the mesh was seen lying free within the gastric lumen and was effortlessly extracted (Figure 1). She continues to do well but requires a proton pump inhibitor medication for gastroesophageal reflux disease. This case underscores the challenges encountered in managing mesh complications following hiatal hernia surgery. Mesh erosion at the GEJ is a well-described complication of permanent meshes; therefore, permanent mesh should never be used near the GEJ. There are case reports of successful endoscopic extraction of mesh through the esophagus without injury to the esophagus or free perforation, indicating that these non-absorbable meshes often wall themselves off from the peritoneal cavity as they erode through the GEJ. In this case, the placement of a stent provided time for the patientís nutritional status to improve and serendipitously allowed the mesh to fully migrate through the GEJ