Abstract
Introduction
Racial and ethnic disparities are present in outcomes after bariatric surgery. Effects of the COVID-19 pandemic on these pre-existing disparities are less well-characterized. We hypothesize that the pandemic has disproportionately affected outcomes of patients of different racial and ethnic groups undergoing bariatric surgery and strive to identify trends.
Methods and Procedures
This is a retrospective cohort study evaluating outcome disparities in patients receiving bariatric surgery from 2016-2019 (pre-COVID) and 2020-2021 (post-COVID) using the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database. Outcomes were categorized by Clavien-Dindo (CD) scores (0-5) and extended length of stay (eLOS) defined as >90th percentile. Thirty-day post-operative outcomes were assessed for non-Hispanic White (NHW), non-Hispanic Black (NHB), Hispanic, and non-Hispanic Asian/Native American/Pacific Islander (A/NA/PI) using chi-square and multinomial logistic regression.
Results
A total of 1,055,503 patients were included in the analysis. We found that compared to NHW, NHB patients were more likely to experience postoperative complications before covid as characterized by CD scores of 1-2, 3-4, and 5 compared to 0 (IRR 1.36, p<0.0001; IRR 1.19, p<0.0001; IRR 1.26, p=0.02, respectively). Post-COVID, we found that NHB were still more likely to have CD scores of 1-2, 3-4, but not 5 (IRR 1.36, p<0.0001; IRR 1.20, p<0.0001; IRR 1.15, p=0.392, respectively). NHB were more likely after COVID to have eLOS than NHW (IRR 1.65, P<0.0001 compared to IRR 1.47 p<0.0001 pre-COVID). Hispanic patients experienced fewer postoperative complications compared to NHW both pre- and post-COVID, except in the CD 1-2 category pre-COVID (IRR 1.04, P=0.001). However, they were more likely to have eLOS after COVID when compared with NHW (IRR 1.20, p<0.0001 post-COVID; IRR 1.13 p<0.0001 pre-COVID). There was no difference between A/NA/PI and NHW for any CD categories however, they also experienced greater likelihood of eLOS post-COVID when compared to NHW (IRR 1.20, p=0.002 post-COVID; IRR 1.10 p<0.0001 pre-COVID).
Conclusions
NHB patients continue to experience inferior post-operative outcomes when compared to patients of other races after bariatric surgery and this difference persisted after the pandemic. Hispanic ethnicity was protective. All non-White race/ethnicity patients experienced greater likelihood of eLOS when compared to NHW and this disparity increased in likelihood after the pandemic. Limited data on socioeconomic status, access to care, geographic data, and psychological co-morbidities in the MBSAQIP limit our ability to understand why NHB race continues to be an independent predictor of adverse outcomes. Future directions include institutional data of the same patient cohorts to further investigate this trend.
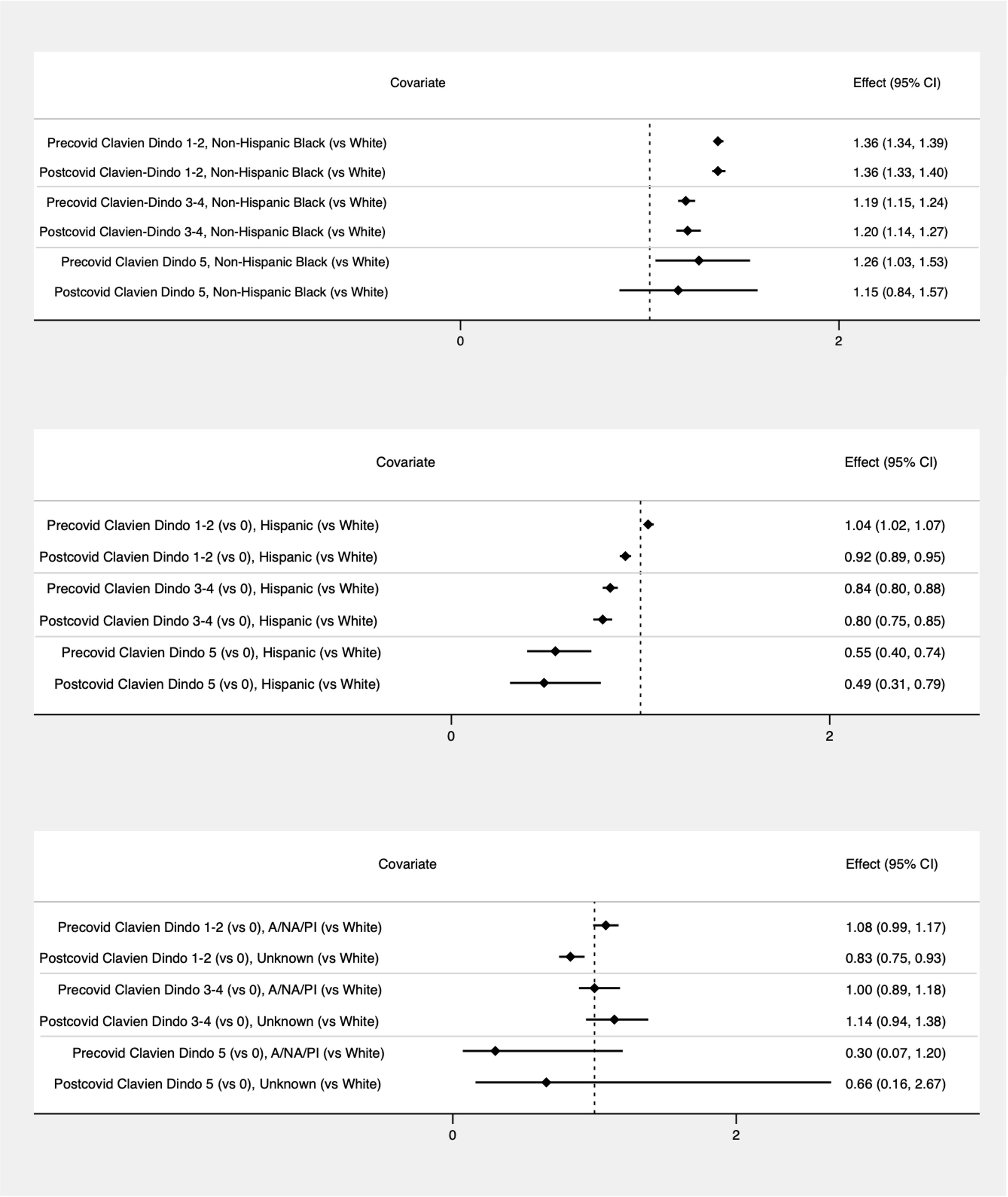
Multivariable risk ratios of Clavien-Dindo grades pre and post-COVID by race/ethnicity with non-Hispanic Black patients (top), Hispanic patients (middle), and non-Hispanic Asian, Native American, and Pacific Islanders (bottom).