Introduction: Obesity remains an epidemic in the United States, particularly in the Deep South where there is a high burden of disease. Bariatric surgery remains the most effective and durable treatment for morbid obesity yet is underutilized in the Deep South. Rural populations have reduced access to care and worse surgical outcomes. Approximately 70-80% of the Deep South live in rural areas. Therefore, this study sought to assess access to bariatric surgery and postoperative quality metrics at a large tertiary bariatric center in the Deep South among rural and non-rural patients.
Methods: All patients referred for primary bariatric surgery from 2012-2023 were identified from a single institutional database (n=3,083). Patients were geocoded and stratified by rural or non-rural status, according to the rural-urban commuting area codes from their home addresses. Clinic appointment attendance after referral, access to surgery (patients who underwent bariatric surgery), and postoperative outcomes were compared within the groups using Pearsonís chi-squared test or ANOVA. Multivariable linear and logistic regression were used to assess short (length of stay (LOS), readmissions) and long-term postoperative outcomes (% weight loss at 6 months, 1 year, 3 years).
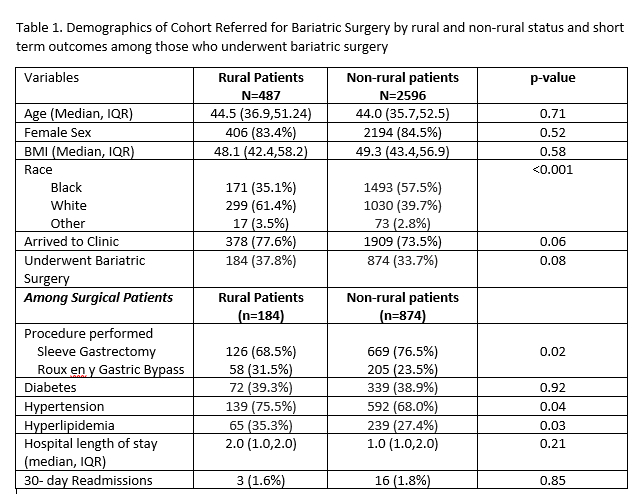
Results: Most bariatric referrals were urban patients (84.2%, n=2,956; rural 15.8%, n=487). However, after initial referral, there were no differences in clinic appointment attendance by rural or non-rural status. Among those who presented to clinic, 48.7% (n=184) of rural patients underwent bariatric surgery, compared with 45.8% (n=874) of urban patients (p=0.30). Rural patients referred were predominately White (61.4%, n= 299; Black 35.1%, n=171), while urban patients were more commonly Black (57.5%, n= 1,493; White 43.1%, n=1,329; p<0.001). There were no differences in short term outcomes by rurality or long-term weight loss (Table). However, in multivariate models accounting for rurality, White patients had shorter estimated LOS (-0.28 days (-0.50,-0.06; p=0.01) and greater weight loss following bariatric surgery at each time point (estimated change in % body mass index of -1.85 at 6 months (-3.05,0.66; p-0.002), -3.42 at one year (-5.47,-1.37; p=0.001), -5.56 at 2 years (-9.02,=2.10; p=0.002) and -6.68 at 3 years (-12.6,-0.79; p=.03).
Conclusions: This review from a large tertiary center demonstrated that despite serving a largely rural state in the Deep South, most of the bariatric surgery referrals were for urban patients. Those who were referred from rural areas were more commonly White compared with their urban counterparts. Rural patients once referred for bariatric surgery have acceptable outcomes, but racial disparities in some short and long term outcomes exist. Future studies are needed to determine barriers to referral for rural patients.