Introduction: Gastrointestinal stromal tumors (GIST) are rare mesenchymal neoplasms of the gastrointestinal tract. Complete surgical resection is the primary treatment. Although, open surgical resection has been traditionally performed, laparoscopy is increasingly used for GIST resection with similar oncological outcomes. This study examined current trends in open and laparoscopic resection for GIST management in the US.
Methods: We examined the National Inpatient Sample (NIS) database from 2016-2020 to retrospectively identify patients who underwent open and laparoscopic surgical resection for malignant GIST tumors using ICD-10- CM codes. Only patients with tumors in the stomach and small intestine were included. Tumors arising elsewhere in the GI tract were excluded from the study. Multivariable analyses were performed to assess differences in age, sex, ethnicity/race, income, insurance, Charlson Comorbidity Index (CCI), and hospital characteristics between surgical approach i.e laparoscopic versus open. Surgical outcomes including length of stay (LOS), complications, expenditures, and in-hospital mortality were analyzed by surgical approach.
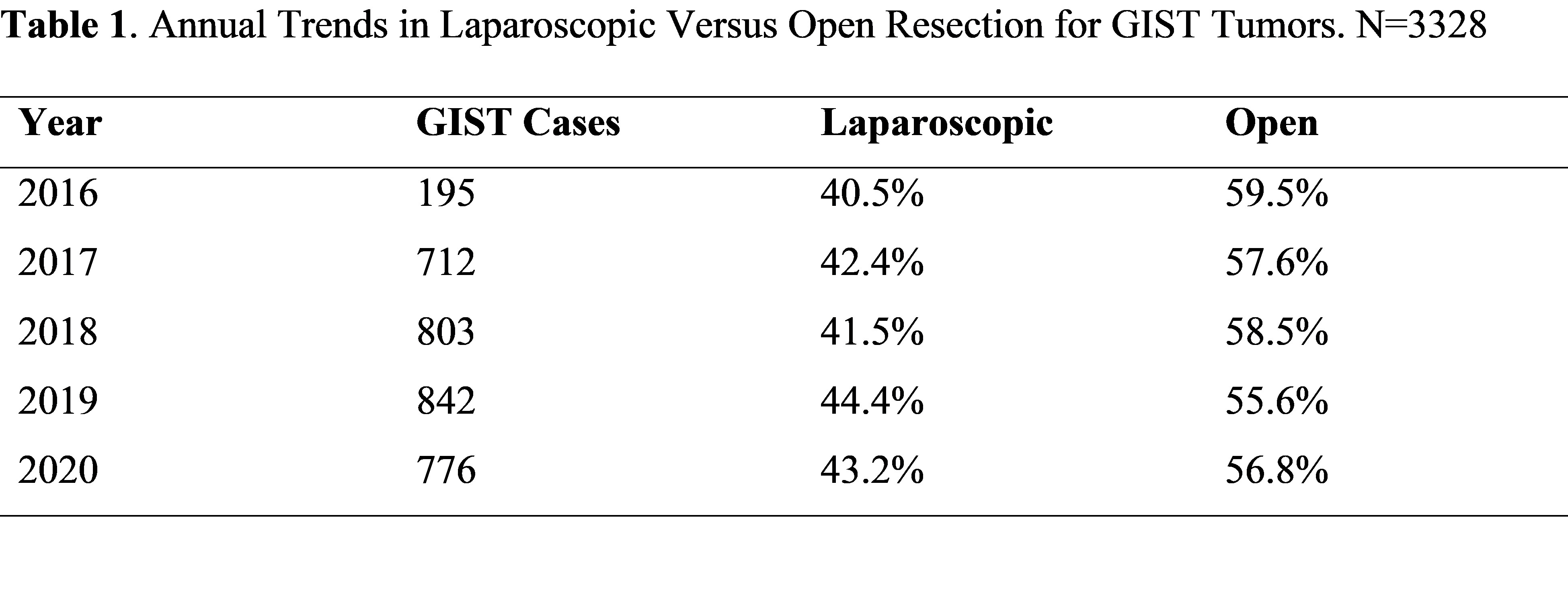
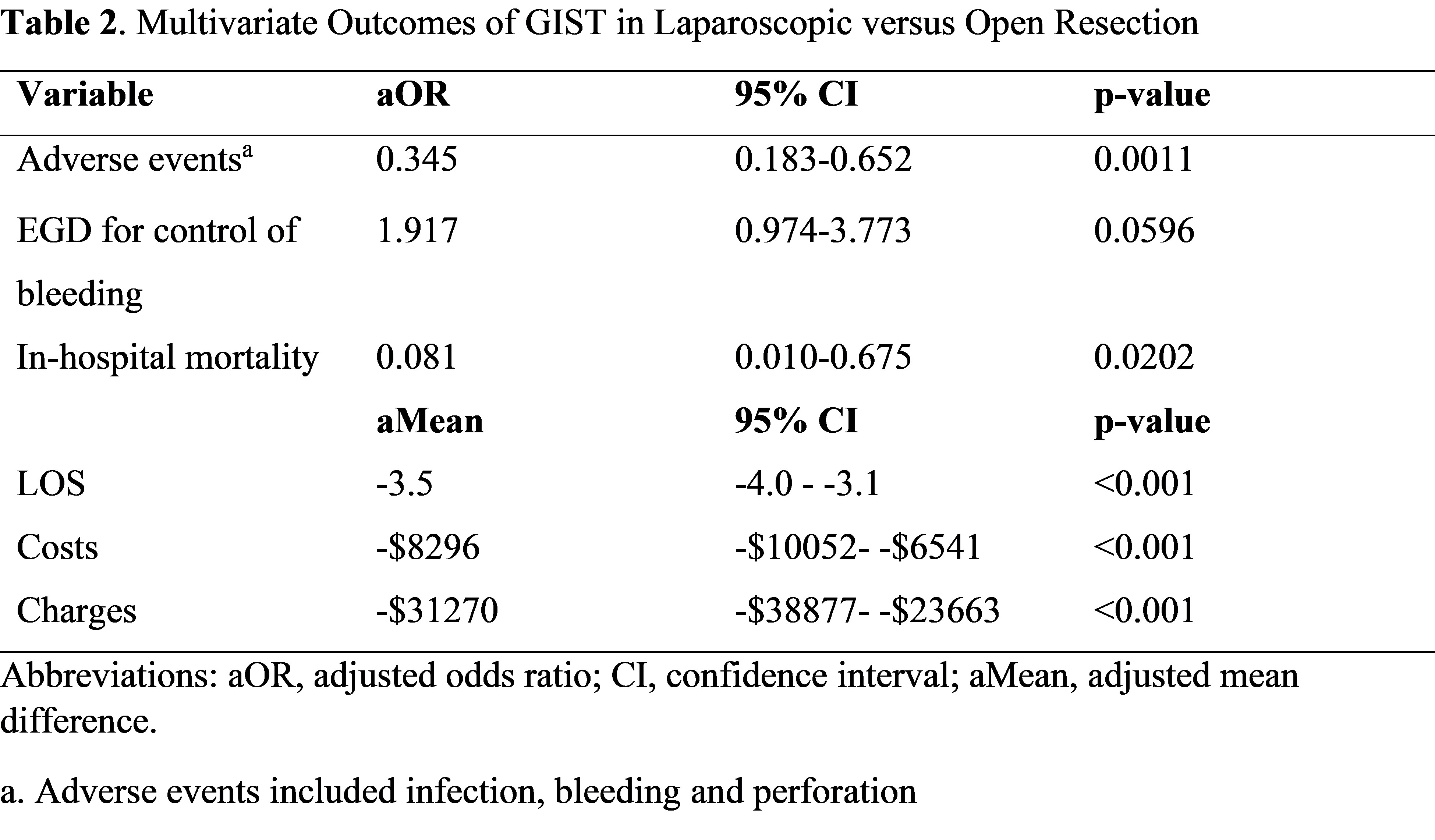
Results: A total of 3,328 patients were identified; 1,905 patients (57.2%) underwent open resection, while 1,423 patients (42.8%) underwent laparoscopic surgery. The mean patient age was 64 years, 50.1% were female. The use of laparoscopic resection increased from 40.5% to 43.2% while open resection decreased from 59.5% to 56.8% in the study period (2016-2020). Patients who underwent laparoscopic resection were more likely to be female (53.3% vs. 47.8%), morbidly obese (7.5% vs. 4.9%) or treated in the Northeast US region (23% vs 19%). Open surgery was associated with 3 or more comorbidities (56.0% vs. 51.2%), emergent surgery (33.5% vs. 18.7%) or South US region (39.1% vs 34.7%). Adverse events were noted in 97 cases (5.1%) in open versus 20 cases (1.4%) in laparoscopic resection. Laparoscopic surgery was associated with lower odds of adverse events (aOR 0.35; p=0.001), and in-hospital mortality (aOR 0.08; p= 0.02). The adjusted LOS, hospital costs and charges were lower by 3.5 days (p <0.001), ,296 (p <0.001) and ,270 (p <0.001) in the laparoscopic group, respectively.
Conclusion: This study demonstrates that the overall rates of laparoscopic resection for GIST tumors in the US increased from 2016 to 2020. Laparocopic resection was associated with fewer immediate adverse events, lower in-hospital mortality, shorter LOS and reduced hospital expenditures. Our study adds incremental evidence to the safety and cost effectiveness of laparoscopic GIST resection.