Background: Gastrointestinal (GI) hemorrhage is a common indication for hospitalization, both in the general populace and in those with history of bariatric surgery. The aim of this study was to investigate the effect of prior bariatric surgery on inpatient mortality and complications in patients hospitalized with non-variceal upper GI bleed.
Materials and Methods: We performed a retrospective case-control study utilizing the National Inpatient Sample (NIS) database from October 2015 to December 2020. All adults hospitalized with non-variceal upper GI bleed were identified and stratified into those with (case) and without (control) a history of bariatric surgery (Roux-en-Y gastric bypass or sleeve gastrectomy). Primary outcomes were differences in mortality rate and inpatient outcomes between the two groups. Secondary outcomes were organ failures: blood transfusion requirement, endoscopic procedures rates, hemorrhagic shock, acute kidney injury (AKI) respiratory failure requiring mechanical ventilation, sepsis, and length of stay. Multivariate regression models were constructed to adjust for confounders and hospital characteristics.
Results: A total of 1,742,025 (weighted) hospitalizations were included, 67,010 of which had history of bariatric surgery. Inpatient mortality rates were lower in patients with prior bariatric surgery (1.2% vs 2.2%, p<0.001). After adjusting for confounding factors, bariatric surgery was independently protective against inpatient mortality after hospitalization for non-variceal upper GI bleed (odds ratio [OR] 0.70, 95% confidence interval [CI] 0.60-0.82, p<0.001). Female sex was also protective against mortality (OR 0.93, 95% CI 0.88-0.97, p<0.001), while white race (OR 1.18, 95% CI 1.12-1.25, p<0.001), age ?65 years (OR 1.39, 95% CI 1.32-1.46, p<0.001), and Charlson comorbidity index ?3 (OR 2.40, 95% CI 2.29-2.53, p<0.001) increased mortality. Bariatric surgery was further associated with lower rates of AKI (13% vs 23%, p<0.001) and sepsis (2% vs 2.7%, p<0.001), however bariatric surgery patients required significantly more endoscopic procedures (47% vs 39%, p<0.001), had higher rates of ileus (2.2% vs 1.7%, p<0.001), longer hospital stay (5.6 vs 4.6 days, p<0.001), and higher total charges (,837 vs ,629, p<0.001).
Conclusion: When hospitalized with non-variceal upper GI bleed, patients with a history of bariatric surgery had lower inpatient mortality and overall better outcomes compared to non-bariatric surgery patients. However, hospital care for bariatric patients had a higher cost, likely due to longer hospital stay and higher rates of endoscopic procedures. This study shows interesting data on the benefits of bariatric surgery when patients are hospitalized with upper GI bleed, however exploring ways to mitigate hospitalization cost could be very beneficial to our healthcare system and are worth studying.
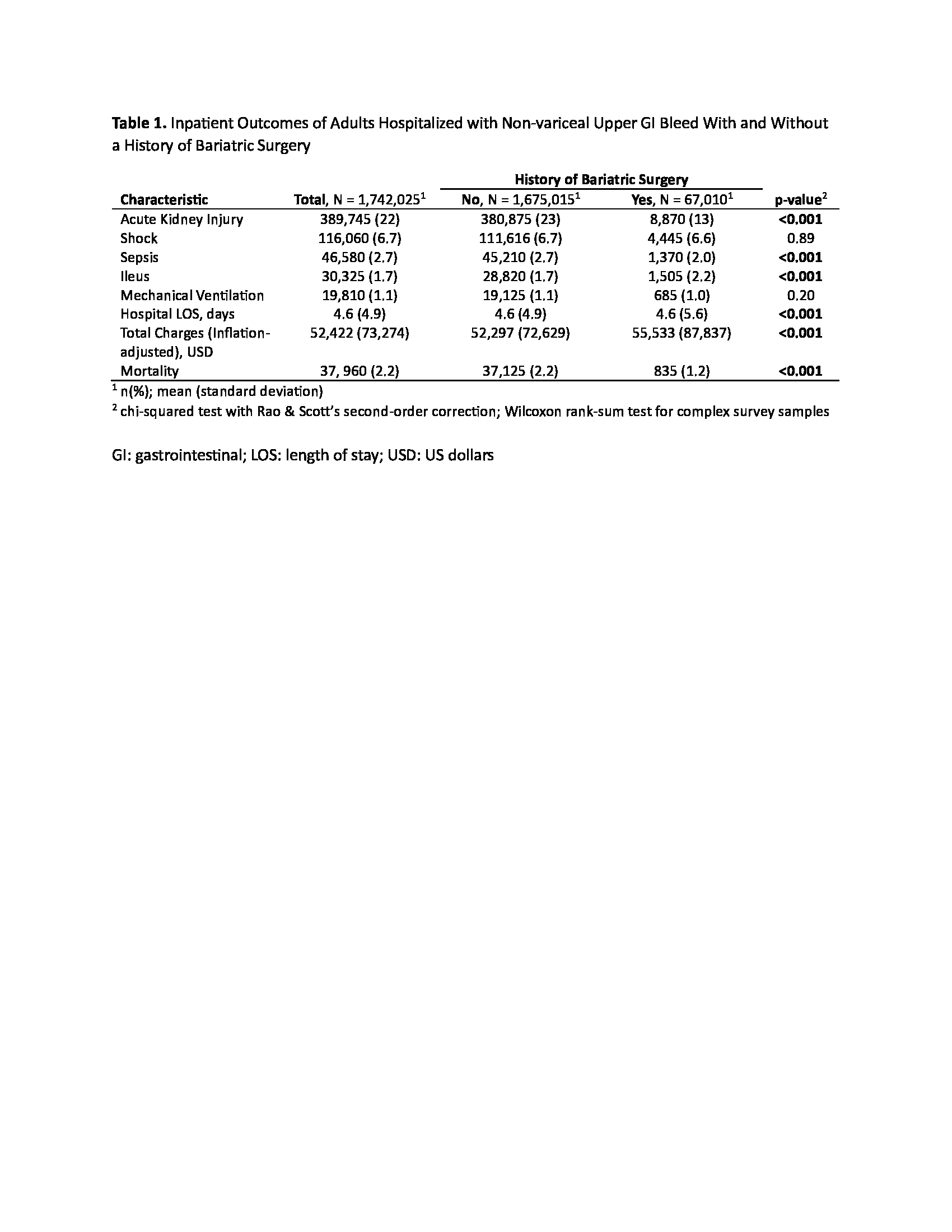
Table 1. Inpatient Outcomes of Adults Hospitalized with Non-variceal Upper GI Bleed With and Without a History of Bariatric Surgery
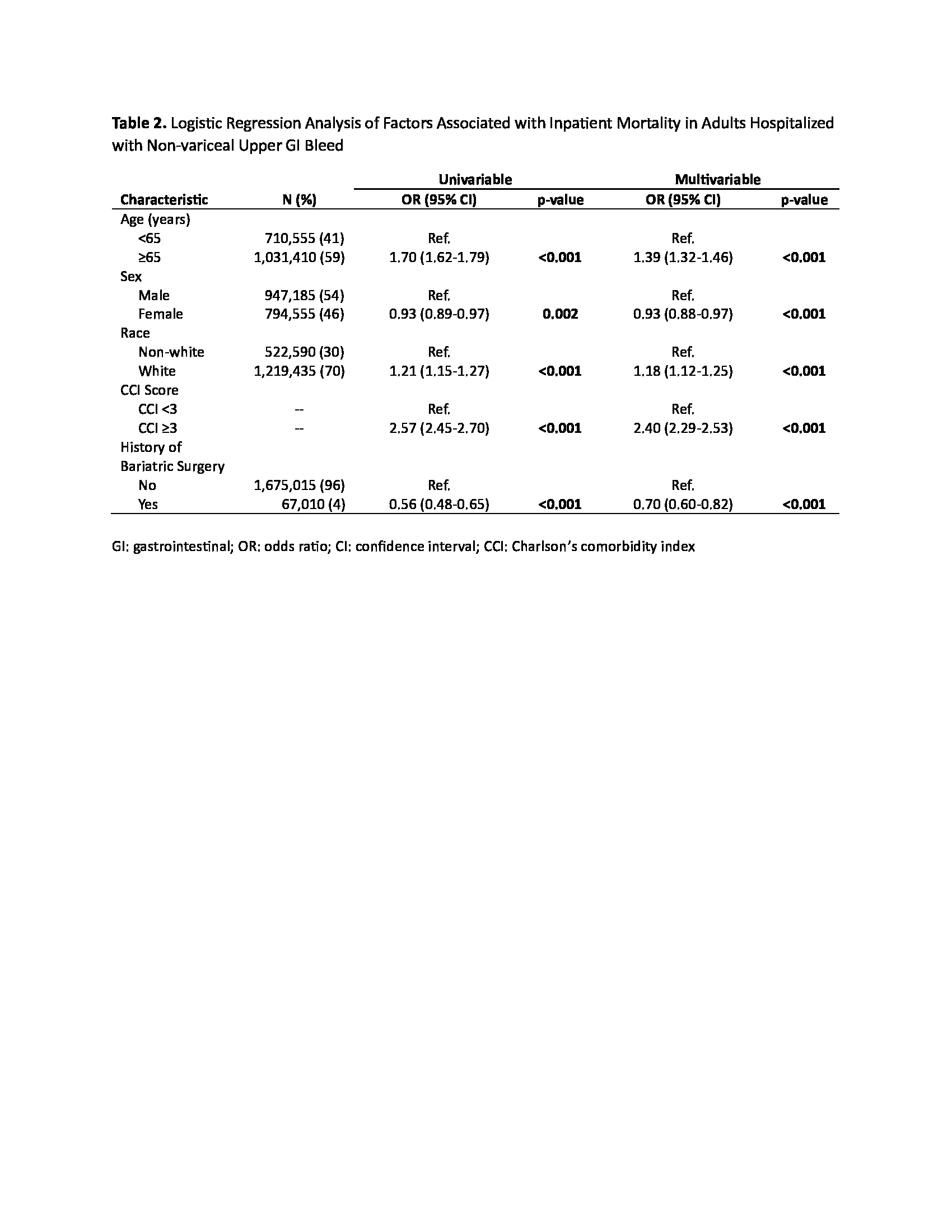
Table 2. Logistic Regression Analysis of Factors Associated with Inpatient Mortality in Adults Hospitalized with Non-variceal Upper GI Bleed