Back to 2024 Abstracts
EFFECTS OF BARIATRIC SURGERY ON MORTALITY AND INPATIENT COMPLICATIONS IN PATIENTS HOSPITALIZED WITH DECOMPENSATED CIRRHOSIS: A NATIONWIDE ANALYSIS
Stephen A. Firkins
*, Yazan Abu Omar, Roma Patel, Heesoo Yoo, Alvin Kwon, Bailey Flora, Jeffrey Shu, Alison Zhao, Meghana Iyer, Roberto Simons-Linares
Gastroenterology, Cleveland Clinic, Cleveland, OH
Background: Both steatotic liver disease and bariatric surgery are becoming increasingly common in light of the rising obesity epidemic. Yet, there is a paucity of literature describing the impact of bariatric surgery on cirrhosis-related outcomes. The aim of this study is to investigate the effect of prior bariatric surgery on inpatient complications and mortality in patients with obesity hospitalized with decompensated cirrhosis.
Materials and Methods: We performed a retrospective case-control study utilizing the National Inpatient Sample (NIS) database from October 2015 to December 2020.
International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) and
Procedural Coding System (ICD-10-PCS) codes were used to identify all adults with obesity hospitalized with decompensated cirrhosis and stratified into those with or without a history of bariatric surgery (Roux-en-Y gastric bypass or sleeve gastrectomy). Primary outcomes were differences in rates of inpatient mortality and cirrhosis-related complications between patients with bariatric surgery and those without (controls). Secondary outcomes included rates of organ failures: acute kidney injury (AKI) respiratory failure requiring mechanical ventilation, shock, sepsis, and length of stay (LOS). Multivariate regression models were constructed to adjust for confounders (including Baveno criteria) and hospital characteristics.
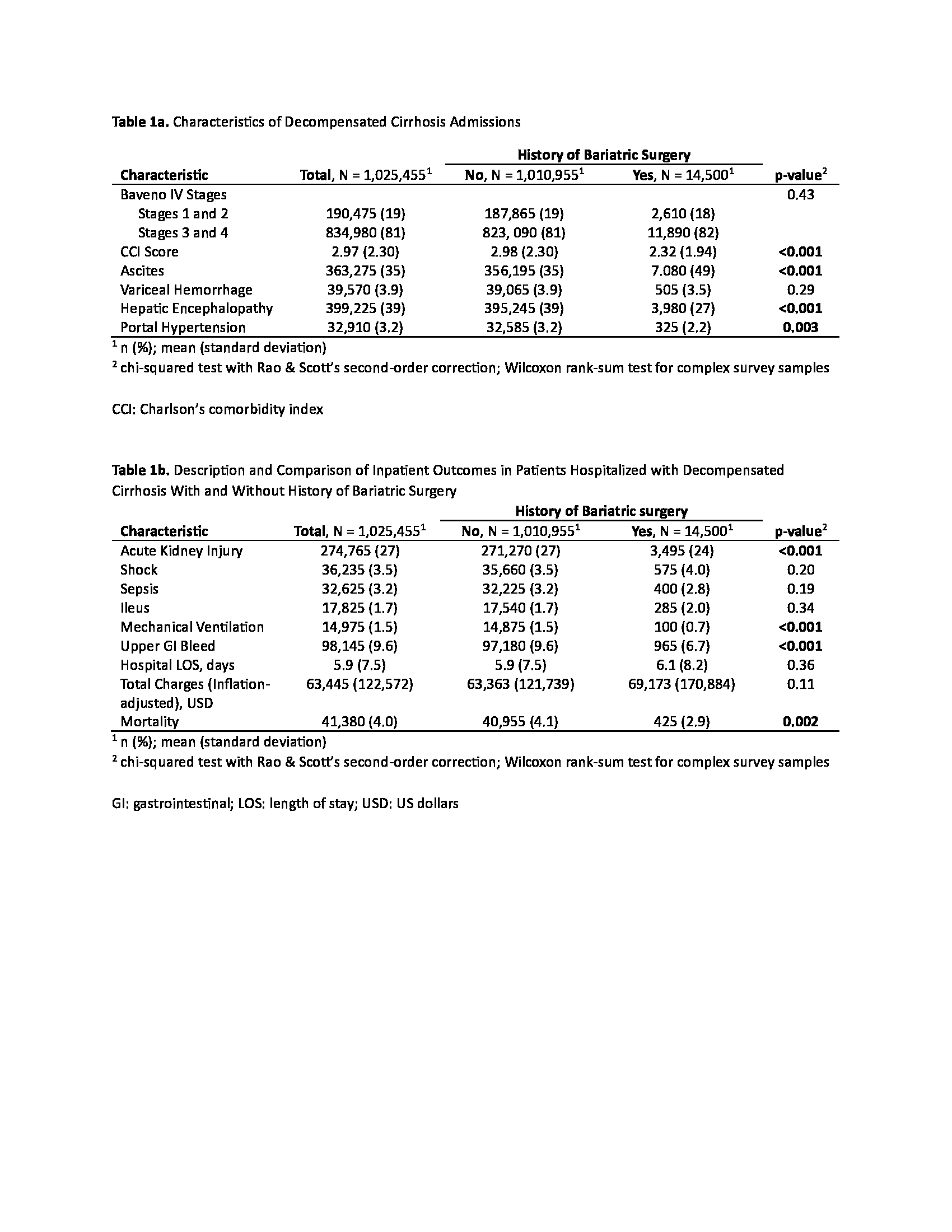
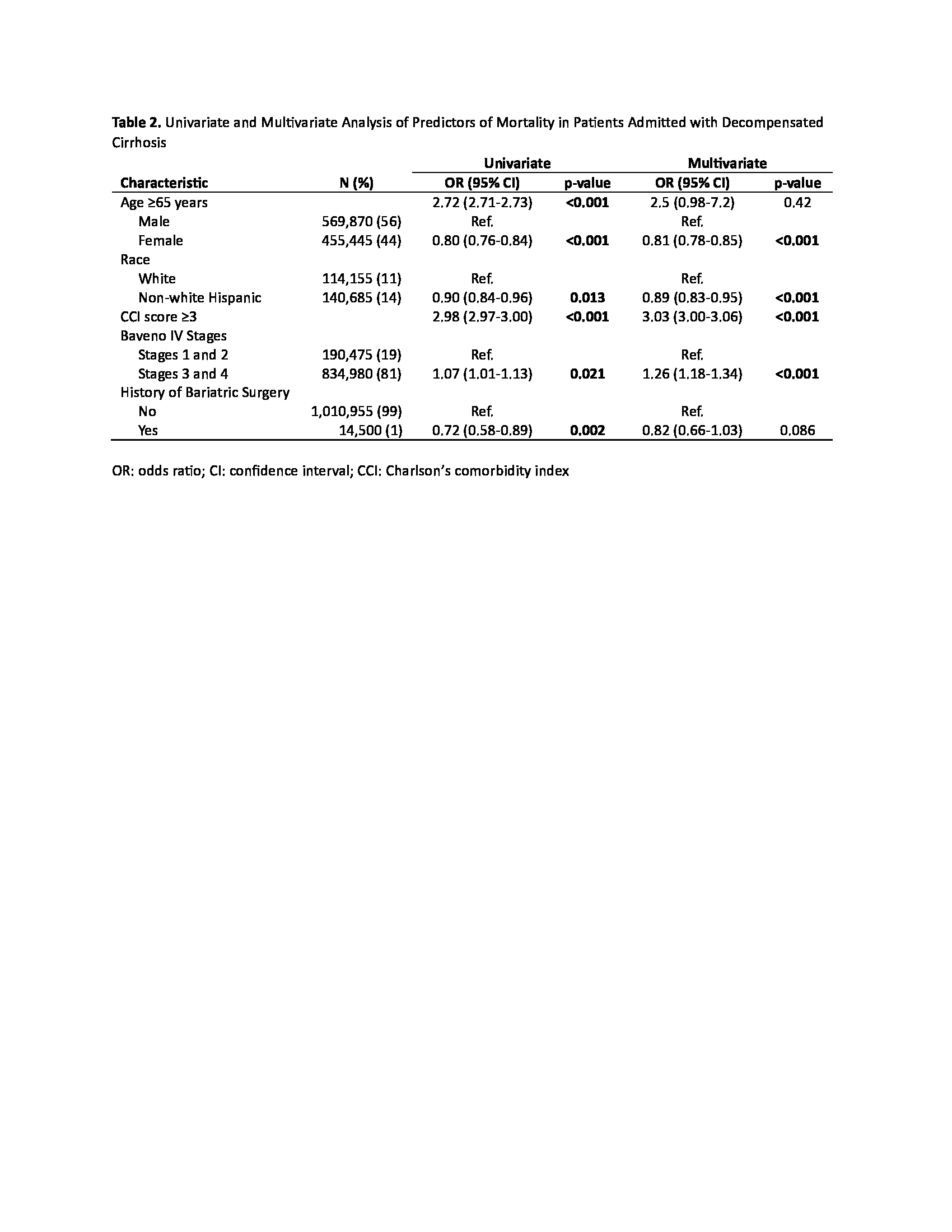
Results: A total of 1,025,455 (weighted) hospitalizations were included, 14,500 of which had history bariatric surgery. Inpatient mortality rates were lower in patients with history of bariatric surgery (2.9% vs 4.1%, p=0.002). Additionally, history of bariatric surgery resulted in lower rates of AKI (24% vs 27%, p<0.001), respiratory failure requiring mechanical ventilation (0.7% vs 1.5%; p<0.001), and upper GI bleed (6.7% vs 9.6%, p<0.001). Furthermore, bariatric surgery was a protective factor against inpatient mortality after hospitalization for decompensated cirrhosis (odds ratio [OR] 0.72, 95% confidence interval [CI] 0.58-0.89, p=0.002). Other protective factors for mortality were female sex (OR 0.81, 95% CI 0.78-0.85, p<0.001) and Hispanic race (OR 0.89, 95% CI 0.83-0.95, p<0.001).
Conclusion: Patients with obesity and history of bariatric surgery have lower inpatient mortality and lower rates of multi-organ failure when hospitalized with decompensated cirrhosis. This study highlights the metabolic benefits of bariatric surgery when treating obesity in patient with cirrhosis. Thus, it is imperative that we advocate for more widespread access to bariatric therapies for patients suffering from obesity and cirrhosis.
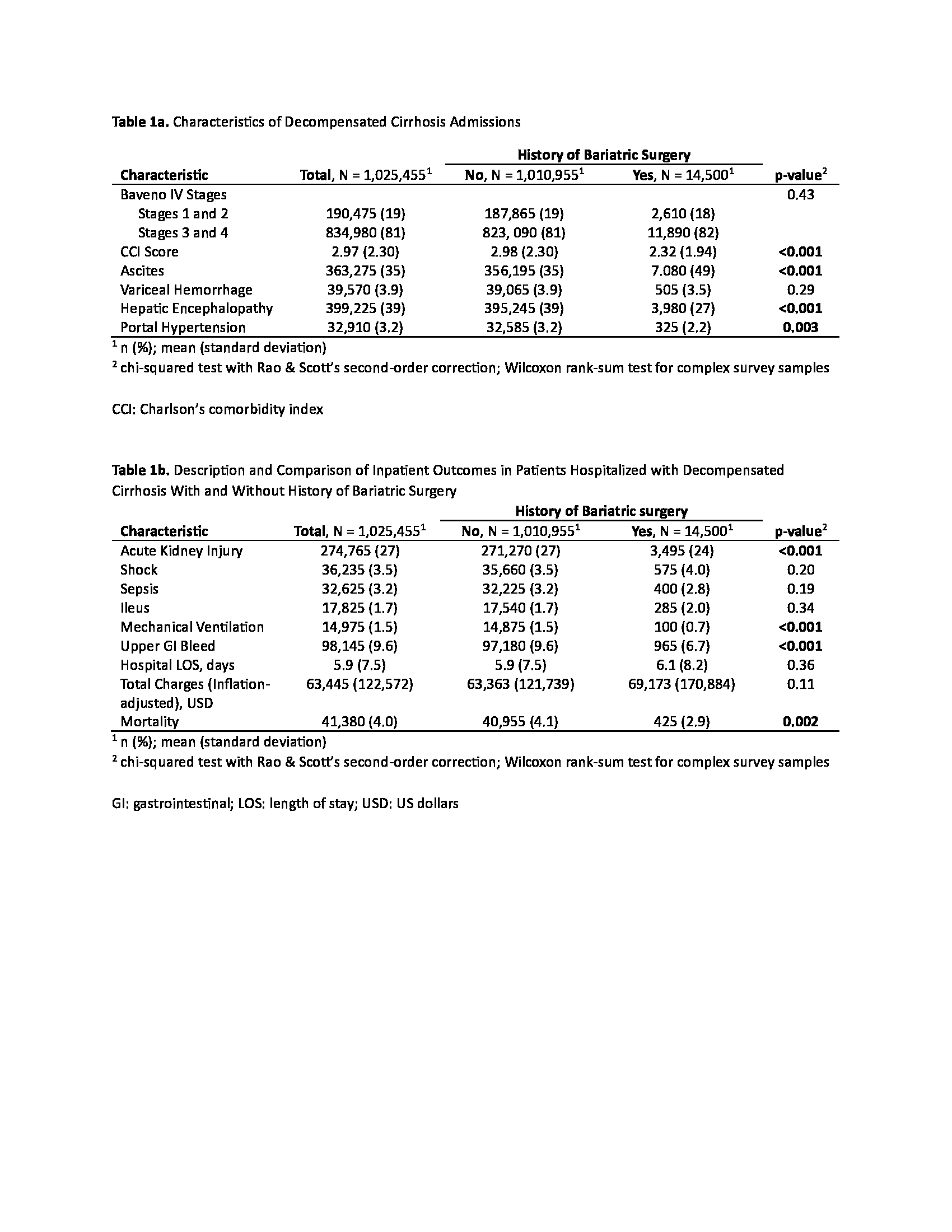
Table 1. Inpatient Outcomes
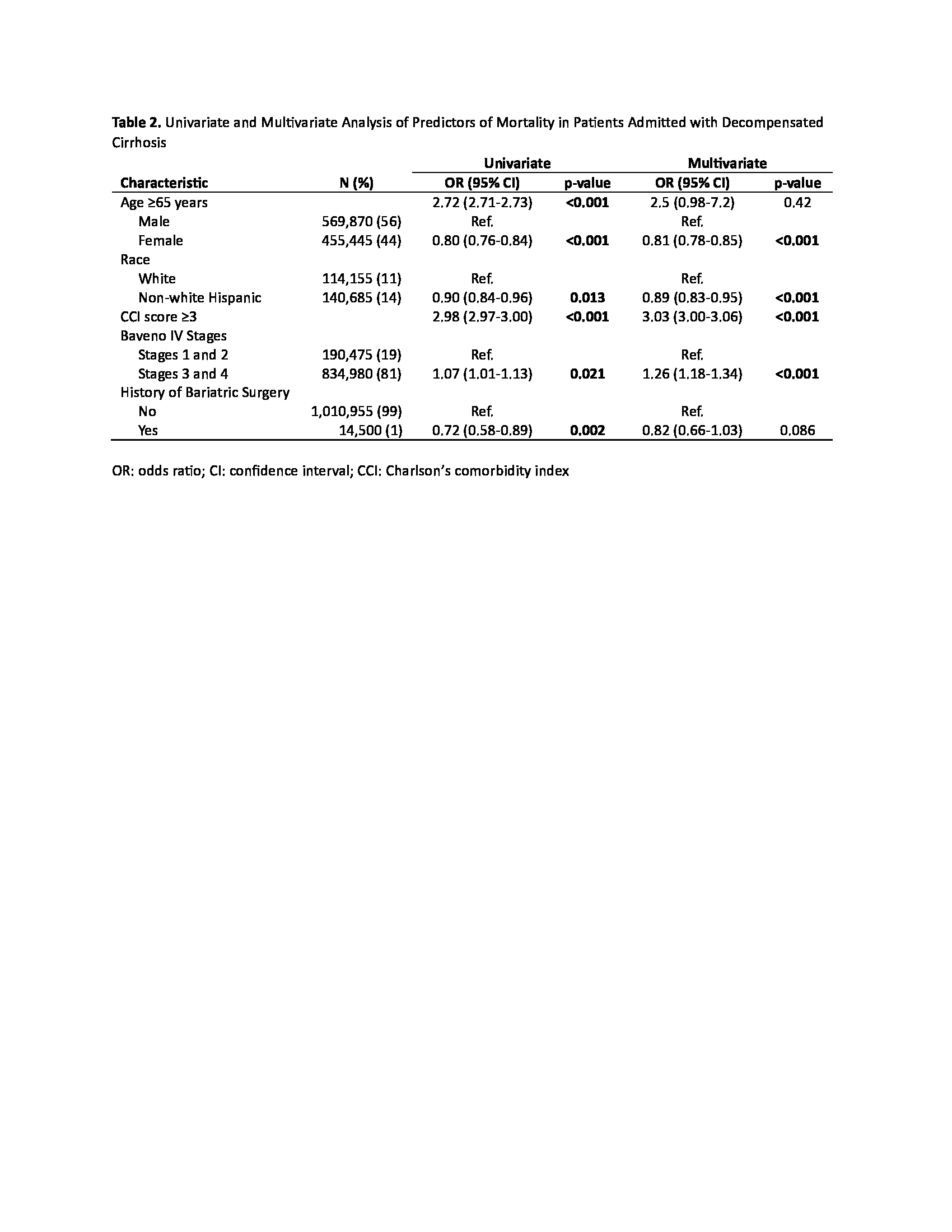
Table 2. Logistic Regression Mortality
Back to 2024 Abstracts