Back to 2024 Abstracts
EFFICACY OF GASTRIC-STIMULATOR AS AN ADJUNCT TO PYLOROPLASTY FOR GASTROPARESIS: CHARACTERIZING PATIENTS SUITABLE FOR SINGLE-PROCEDURE VS DUAL PROCEDURE APPROACH
Sven Eriksson
*1, Margaret Gardner
1, Inanc Sarici
1, Ali H. Zaidi
1, Ping Zheng
1, Blair Jobe
1,2, Shahin Ayazi
1,21Esophageal Institute, Department of Surgery, Allegheny Health Network, Pittsburgh, PA; 2Department of Surgery, Drexel University College of Medicine, Philadelphia, PA
Introduction: Pyloroplasty is an effective surgery for gastroparesis. However, some patients fail to improve after pyloric drainage and may require subsequent gastric electric stimulation. There is a paucity of data on the efficacy of gastric stimulator as an adjunct to failed pyloroplasty. This study aimed to describe our experience with pyloroplasty, determine the efficacy of gastric-stimulator for failed pyloroplasty, and compare the final outcomes of those who required pyloroplasty with and without gastric stimulator for gastroparesis.
Methods: Records of patients who underwent primary pyloroplasty for gastroparesis at our institution were reviewed. Patients with poor symptomatic improvement after pyloroplasty underwent subsequent gastric-stimulator. Symptoms were assessed using the gastroparesis cardinal symptom index (GCSI) preoperatively and after each surgery. Severe gastroparesis was defined as GSCI total score ≥3. Four-hour retention ≤10% on gastric emptying scintigraphy (GES) was considered normal. Outcomes were assessed after pyloroplasty in all patients and after stimulator in patients who failed pyloroplasty. Final outcomes were then compared between those who did and did not require adjunct gastric-stimulator.
Results: The study population consisted of 104 patients (89.4% female) with a mean (SD) age of 42.2(11) and BMI of 26.9(7). Gastroparesis etiologies were 71.2% idiopathic, 17.3% diabetic, and 11.5% postsurgical. At 18.7(12) months after pyloroplasty there was a decrease in the GCSI total score [3.5(1) to 2.7(1.2), p=0.0012] and the rate of severe gastroparesis (71.9% to 29.3%, p<0.0001). GES 4-hr retention decreased [36.5(24) to 15.3(18), p=0.0003].
Adjunct gastric-stimulator was required by 30 (28.8%) patients due to suboptimal outcomes with no improvement in GCSI (p=0.201) or GES (p=0.320). These patients were younger [40.5(10.6) vs 49.6(15.2), p=0.0016)], with higher baseline GSCI-Total scores [4.3(0.7)-vs-3.7(1.1), p<0.001] and more severe gastroparesis (100%-vs-55.6%, p<0.001). All other preoperative characteristics were similar. At 21.7(15) months after gastric-stimulator there was improvement in GCSI [4.1(0.7) to 2.6(1.1), p<0.0001], severe gastroparesis (100% to 43.3%, p<0.0001), and GES 4-hr retention [21.2(22) to 7.6(10), p=0.054].
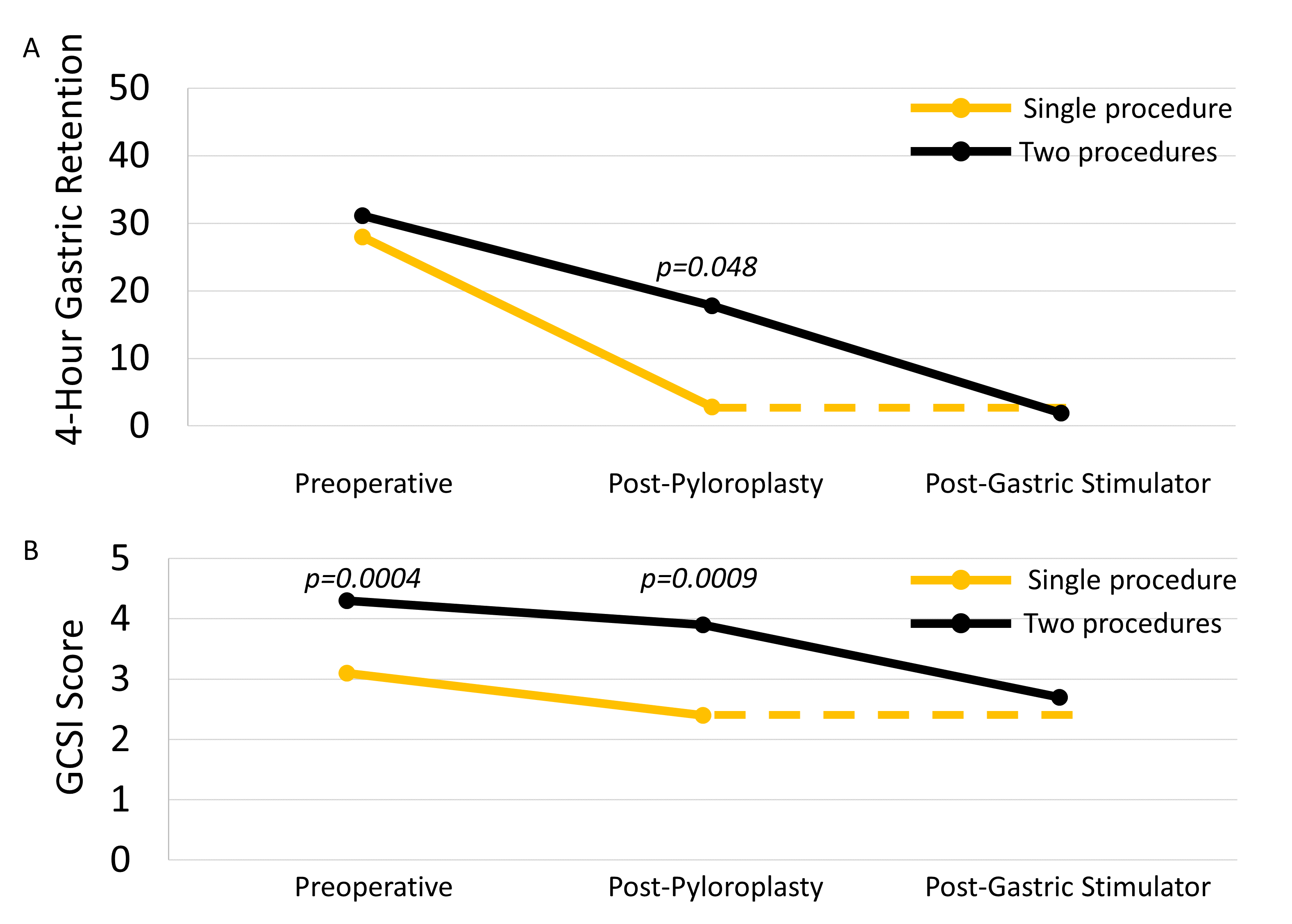
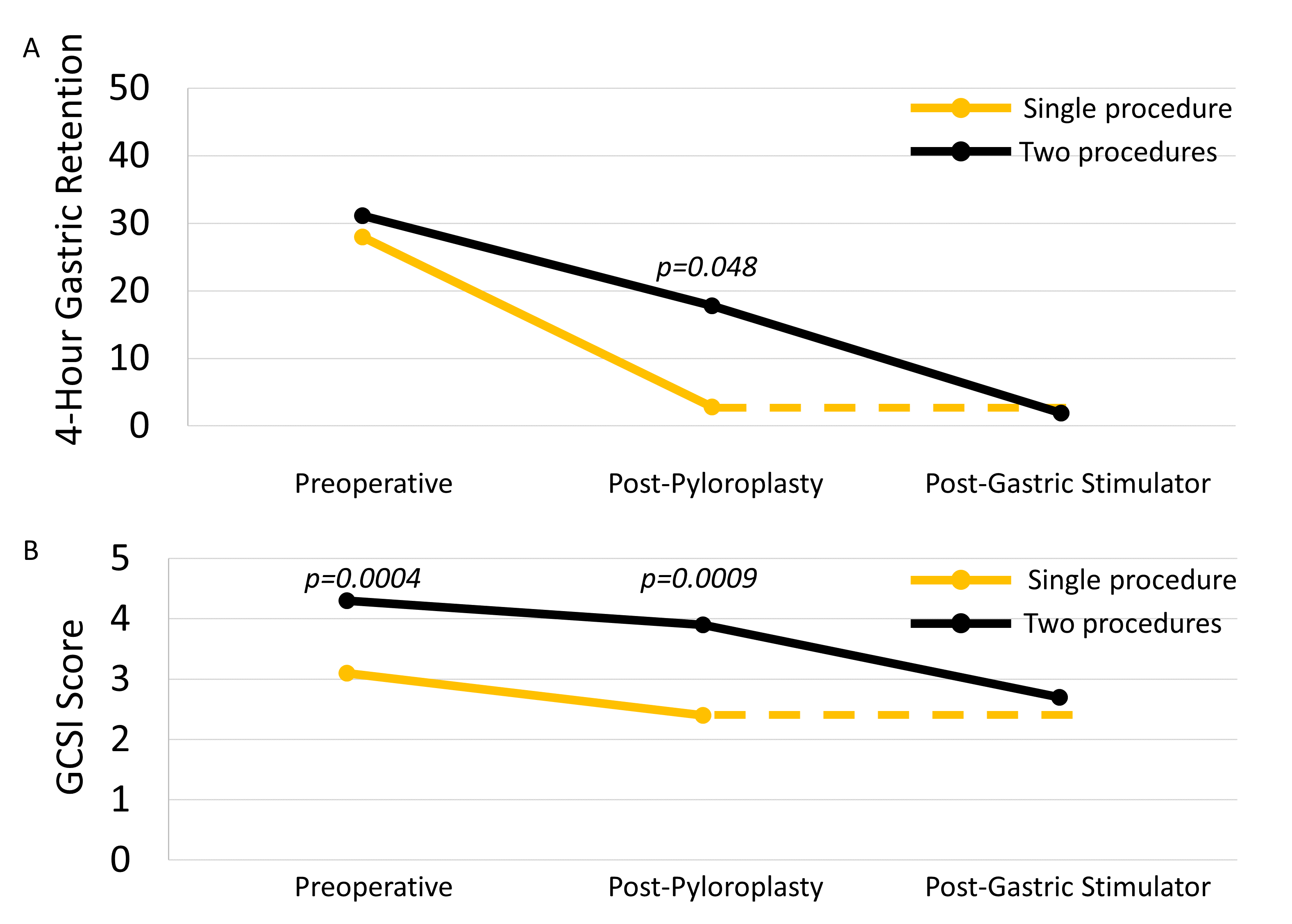
Prior to gastric stimulator, those who failed pyloroplasty had significantly worse GCSI (p=0.0009) and GES (p=0.048) (
Figure). However, after gastric stimulator, GCSI and GES improved, and were comparable to those who only required pyloroplasty (p>0.05).
Conclusion: Pyloroplasty improved gastroparesis symptoms and gastric emptying, yet 28% failed, requiring gastric stimulator. Younger patients and those with preoperative GCSI scores ≥3 were more likely to fail. Gastric stimulator improved outcomes after failed pyloroplasty, with comparable final GCSI and GES to those who did not fail.
Back to 2024 Abstracts