Back to 2024 Abstracts
DIABETES MICROVASCULAR AND MACROVASCULAR COMPLICATIONS PREDICT DIABETES REMISSION AFTER BARIATRIC SURGERY
Wissam Ghusn
*2,1, Marita Salame
2, Karl Hage
2, Khushboo Gala
2, Andrew C. Storm
2, Barham K. Abu Dayyeh
2, Andres Acosta
2, Omar M. Ghanem
21Internal Medicine, Boston University, Boston, MA; 2Mayo Foundation for Medical Education and Research, Rochester, MN
Background:Obesity and type-2 diabetes mellitus (T2DM) are two inter-related chronic diseases with significant medical and financial burden. T2DM results in detrimental vascular complications including microvascular and macrovascular diseases. Bariatric surgeries, particularly Roux-En-Y gastric bypass (RYGB) and sleeve gastrectomy (SG), have demonstrated significant weight loss and T2DM remission (DR) outcomes. However, a remarkable proportion of patients do not achieve DR despite the weight loss associated with a bariatric surgery. Limited data are available on the association between the presence of preoperative microvascular and macrovascular diseases and T2DM remission rate after RYGB or SG. In this study, we assessed the link between these diseases and DR in patients with T2DM after long-term follow-up post-bariatric surgery.
Methods:This is a retrospective cohort study in patients with T2DM who underwent RYGB or SG. We collected data on preoperative microvascular (i.e., retinopathy, nephropathy, and neuropathy) and macrovascular (i.e., coronary artery disease [CAD], cerebrovascular accidents [CVA], and peripheral artery disease [PAD]) diabetes-associated diseases. Our primary endpoint was assessing the association between microvascular and macrovascular diseases at the time of the bariatric procedure and DR after long term follow-up. In addition, secondary endpoints included evaluating the cumulative effect of diabetes-associated diseases on DR. We also performed a multivariate logistic regression to evaluate the parameters associated with DR.
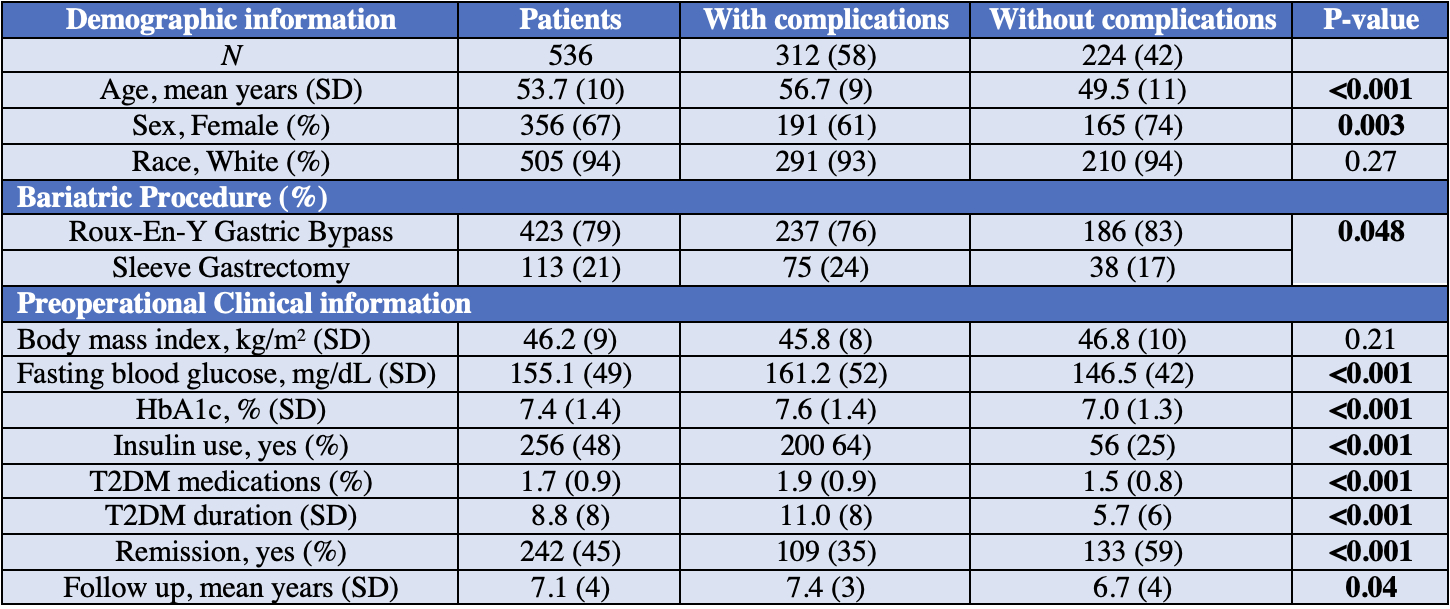
Results:We included 536 patients (356 female [67%], 94% white, mean age 53.7 [10] years, BMI 46.2 [9] kg/m
2) with a mean follow-up period of 7.1 (4) years (
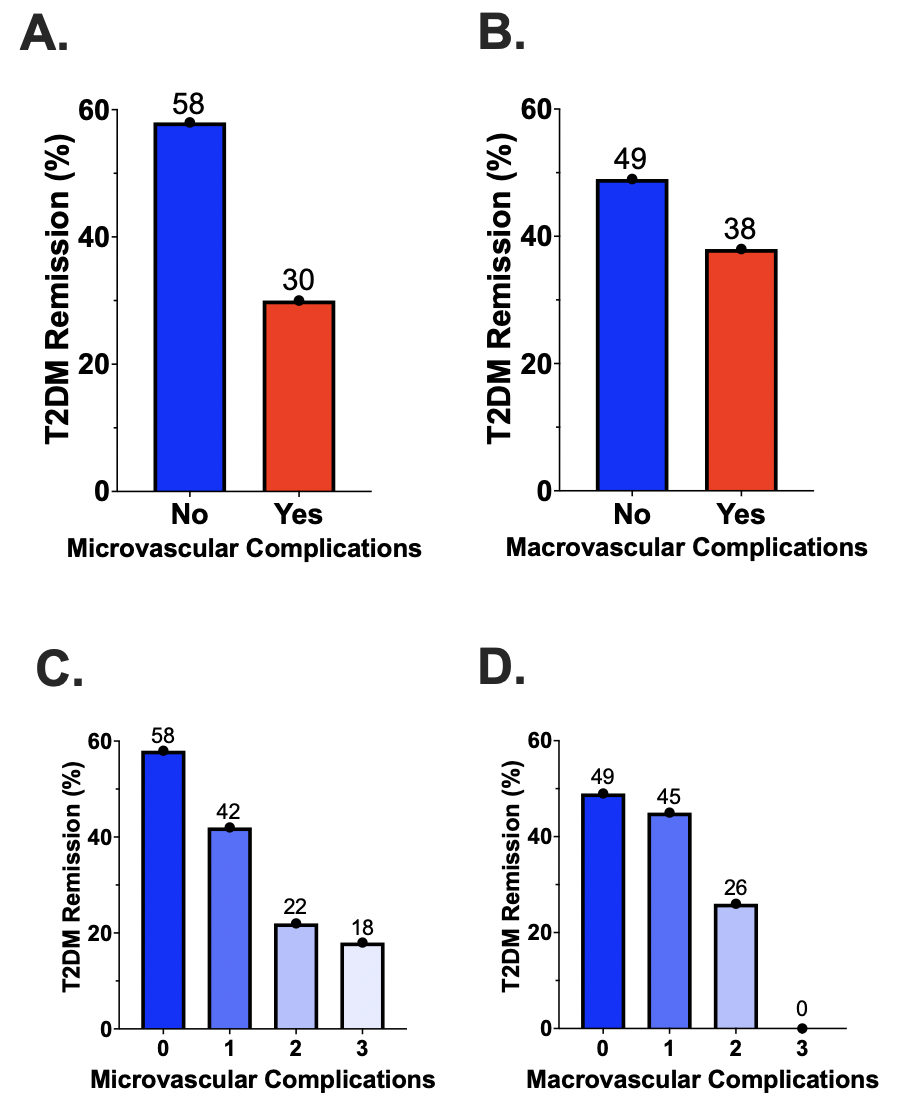
Table 1). Patients without diabetes complications were 2 times more likely to achieve T2DM remission compared to patients with diabetes-associated diseases (27.9% vs 59.4%; p<0.001). Patients with microvascular and macrovascular diseases had a significantly lower T2DM remission rate of (29.7% vs 57.6%; p<0.001,
Figure 1A) and (37.5% vs 49.2%; p=0.01,
Figure 1B) compared to patients without microvascular and macrovascular diseases, respectively. Importantly, there was an additive effect of the number of diabetes complications on the T2DM remission (p<0.001,
Figure 1 C&D). We demonstrate a significant association between HbA1c (p<0.001), number of diabetes medications (p<0.001), T2DM duration (p<0.001), surgery type (p=0.009), and insulin use (p=0.04) with DR.
Conclusion: In this study, patients with pre-surgical microvascular and macrovascular diseases had a lower DR rate after RYGB and SG. These findings reflect inferior remission outcomes in patients with longer duration and more poorly controlled T2DM. Hence, a more aggressive multidisciplinary management might be needed in this cohort of patients to achieve DR after bariatric surgeries.
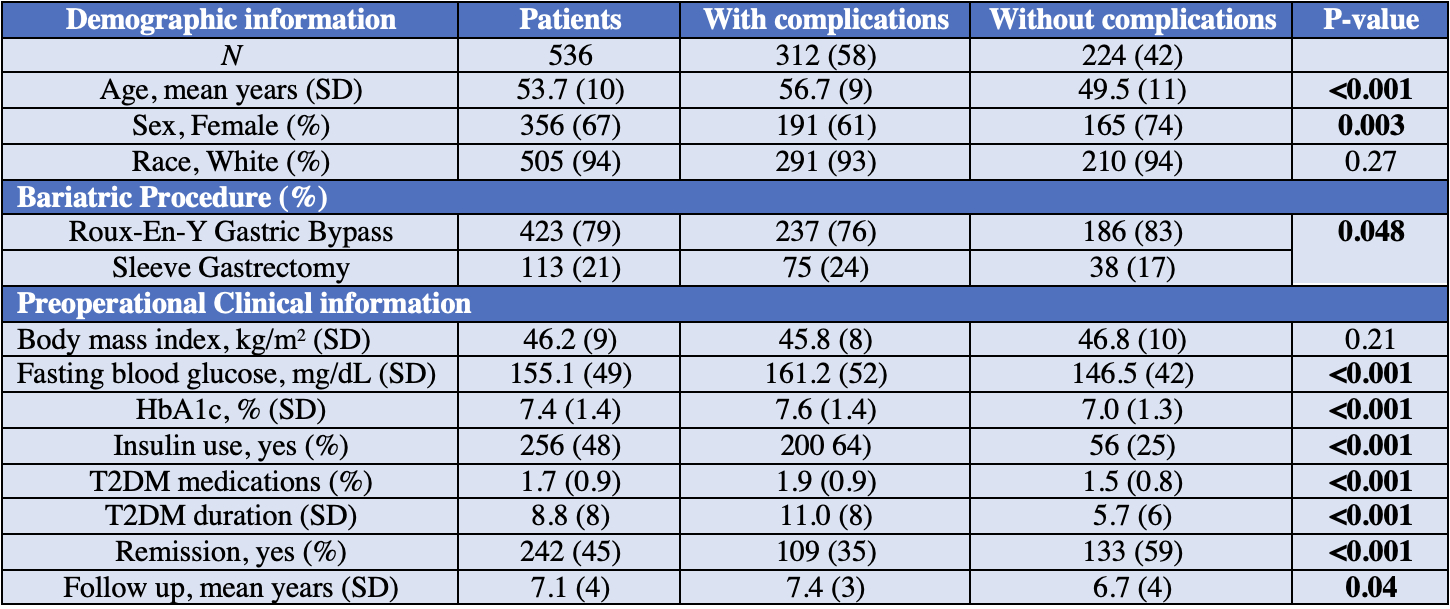 Table 1:
Table 1: Demographic, bariatric and pre-operative clinical information for patients with and without T2DM complications.
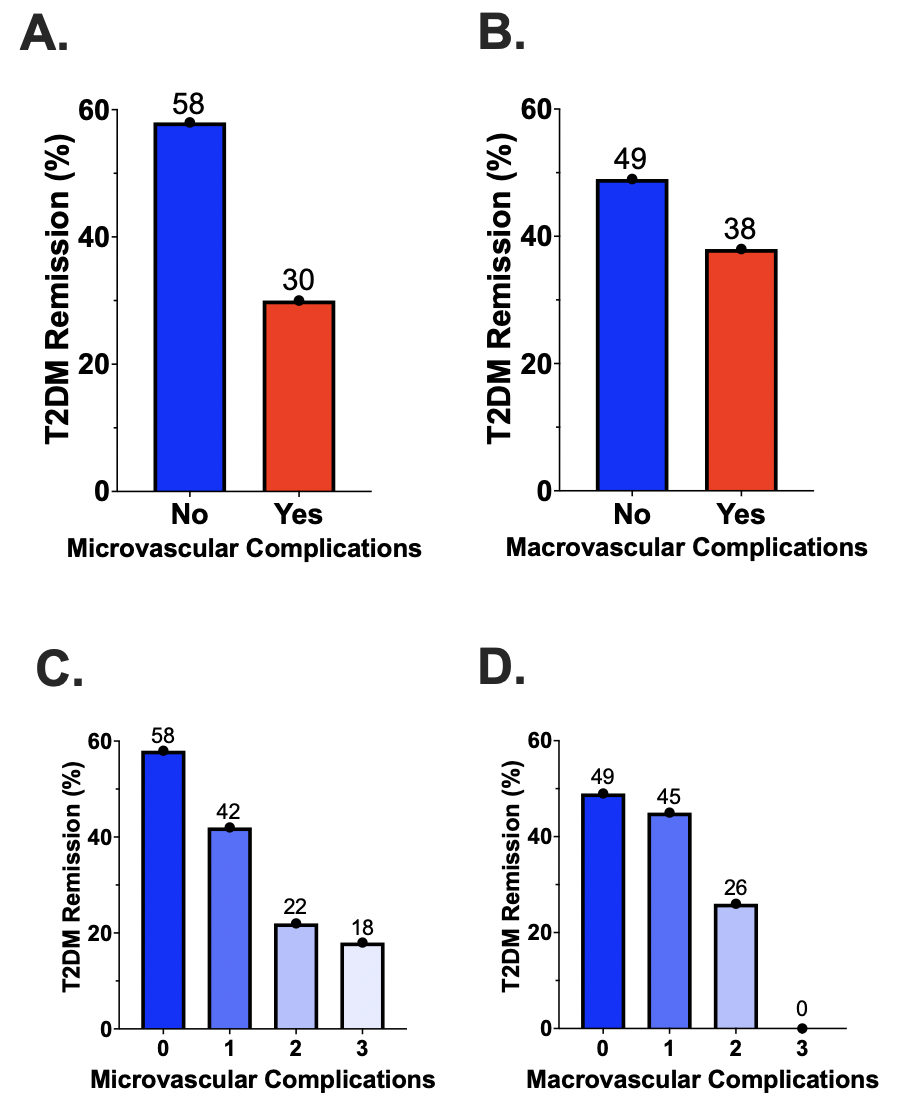 Figure 1:
Figure 1: Diabetes remission in patient with and without microvascular (A) and macrovascular (B) complications, and cumulative effect of microvascular (C) and macrovascular (D) complications on diabetes remission after bariatric surgery.
Back to 2024 Abstracts