Back to 2024 Abstracts
POSTOPERATIVE OUTCOMES OF ANTI-REFLUX SURGERY IN LUNG TRANSPLANT RECIPIENTS
William N. Doyle
1, Monica Stevens
1, Michael P. Rogers
1,2, Rahul Mhaskar
1, Kapil Patel
1,3, Samer Ganam
*2, Christopher DuCoin
1,2, Vic Velanovich
1,21University of South Florida Morsani College of Medicine, Tampa, FL; 2Division of Gastrointestinal Surgery, Department of Surgery, Tampa General Hospital, Tampa, FL; 3Division of Pulmonary and Critical Care Medicine, Tampa General Hospital, Tampa, FL
IntroductionGastroesophageal reflux disease (GERD) is a risk factor for aspiration and subsequent lung allograft rejection. Anti-reflux surgery (ARS) can be utilized for these vulnerable patients to improve symptoms of GERD and thus abate the decline of lung function. Equipoise regarding ideal ARS strategy in this population exists. Accordingly, we sought to compare the efficacy of different ARS in this unique population.
MethodsA single-center retrospective cohort study of lung transplant recipients who underwent ARS between 2011 – 2023 was performed. GERD symptoms were evaluated based on proton-pump inhibitor (PPI) usage at three and six months postoperatively. Pulmonary function testing, postoperative complications, dysphagia complaints, endoscopic dilation, and surgical fundoplication revisions were also evaluated. Variables were compared using Chi-square and Wilcoxon rank-sum tests. P≤0.05 denoted significance.
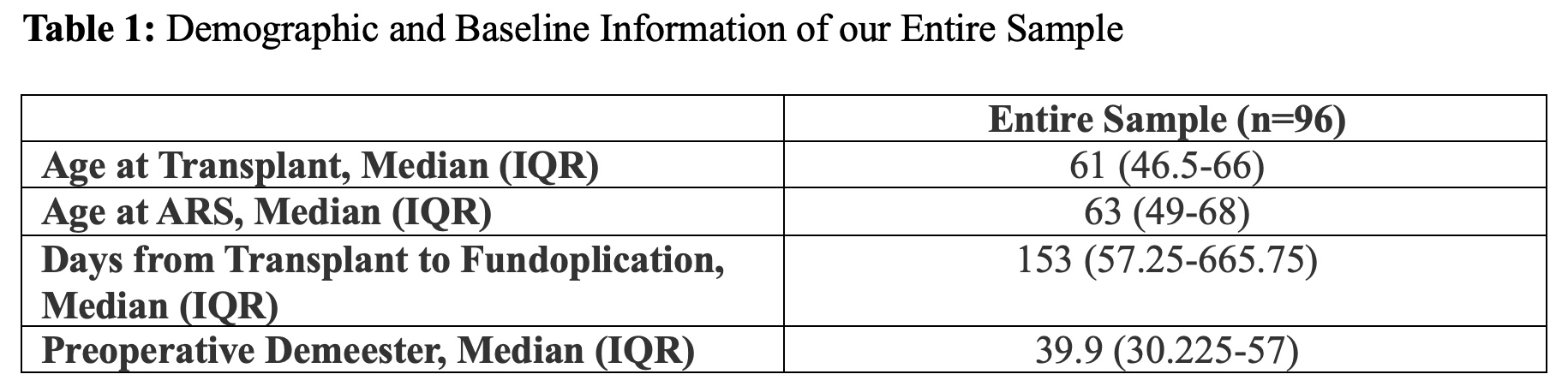
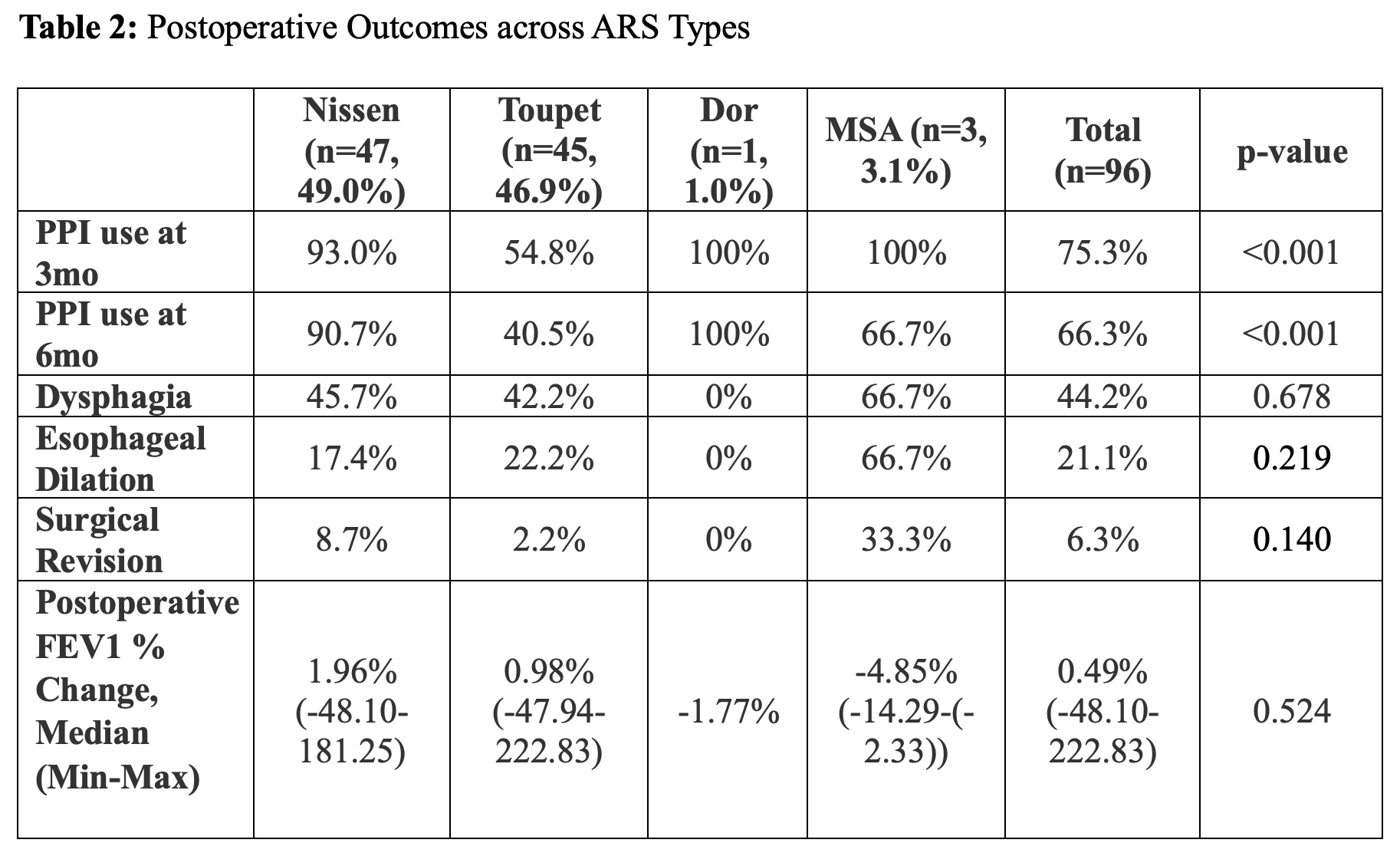
ResultsNinety-six patients undergoing Nissen (49.0%), Toupet (46.9%), or Dor (1.0%) fundoplication, or magnetic sphincter augmentation (MSA, 3.1%) were included for analysis.
Patients with a history of Nissen fundoplication had increased rates of PPI use at 3- (93% vs 54.8%, p<0.001) and 6-months (90.7% vs 40.5%, p<0.001) post-ARS when compared with Toupet patients. However, type of fundoplication was not predictive of the occurrence of post-operative dysphagia. Post-operative dysphagia frequency was similar between Nissen and Toupet patients (45.7% vs 42.2%, p=0.678).
Endoscopic dilation was required for 17.4% of Nissen patients, with 8.7% requiring revision surgery. Endoscopic dilation was performed for 22.2% of Toupet patients, with 2.2% requiring revision surgery. Endoscopic dilation (p=0.219) and surgical revision (p=0.140) rates were statistically insignificant.
Patients did not experience significant change in FEV1 from pre-ARS to postoperatively (1.98L vs. 2.04L, p=0.470). There appears to be no significant difference in median FEV1 percent change postoperatively when comparing Nissen vs. Toupet (1.96% vs. 0.98% respectively, p=0.524).
ConclusionThis study provides descriptive findings of outcomes following ARS in lung transplant recipients. Considering lower PPI usage at 3- and 6- months post-ARS, Toupet fundoplication is superior to Nissen in decreasing the amount of PPI use in lung transplant recipients. Postoperative dysphagia, reintervention, and pulmonary function outcomes are similar between Toupet and Nissen patients.
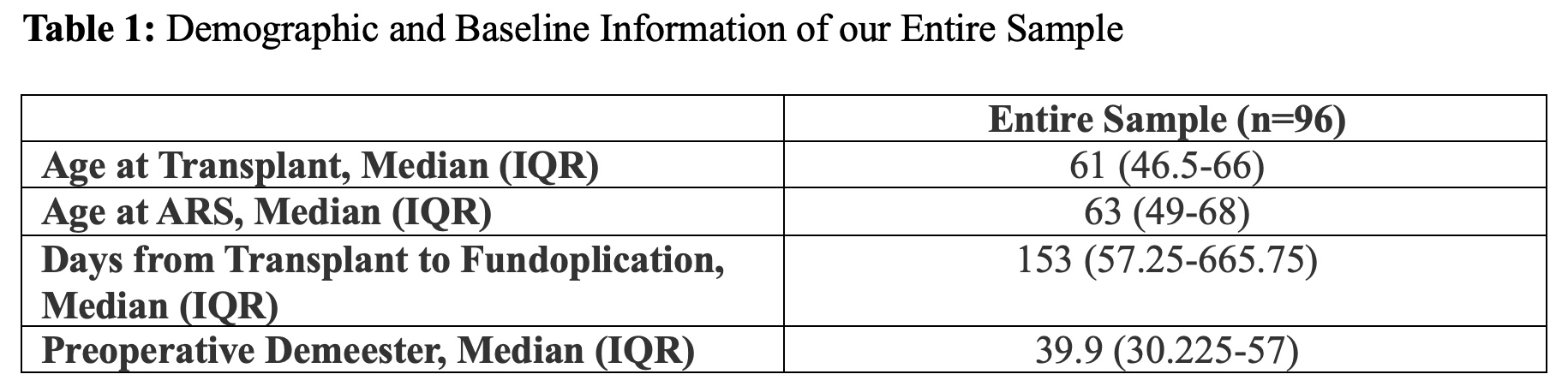
Table 1
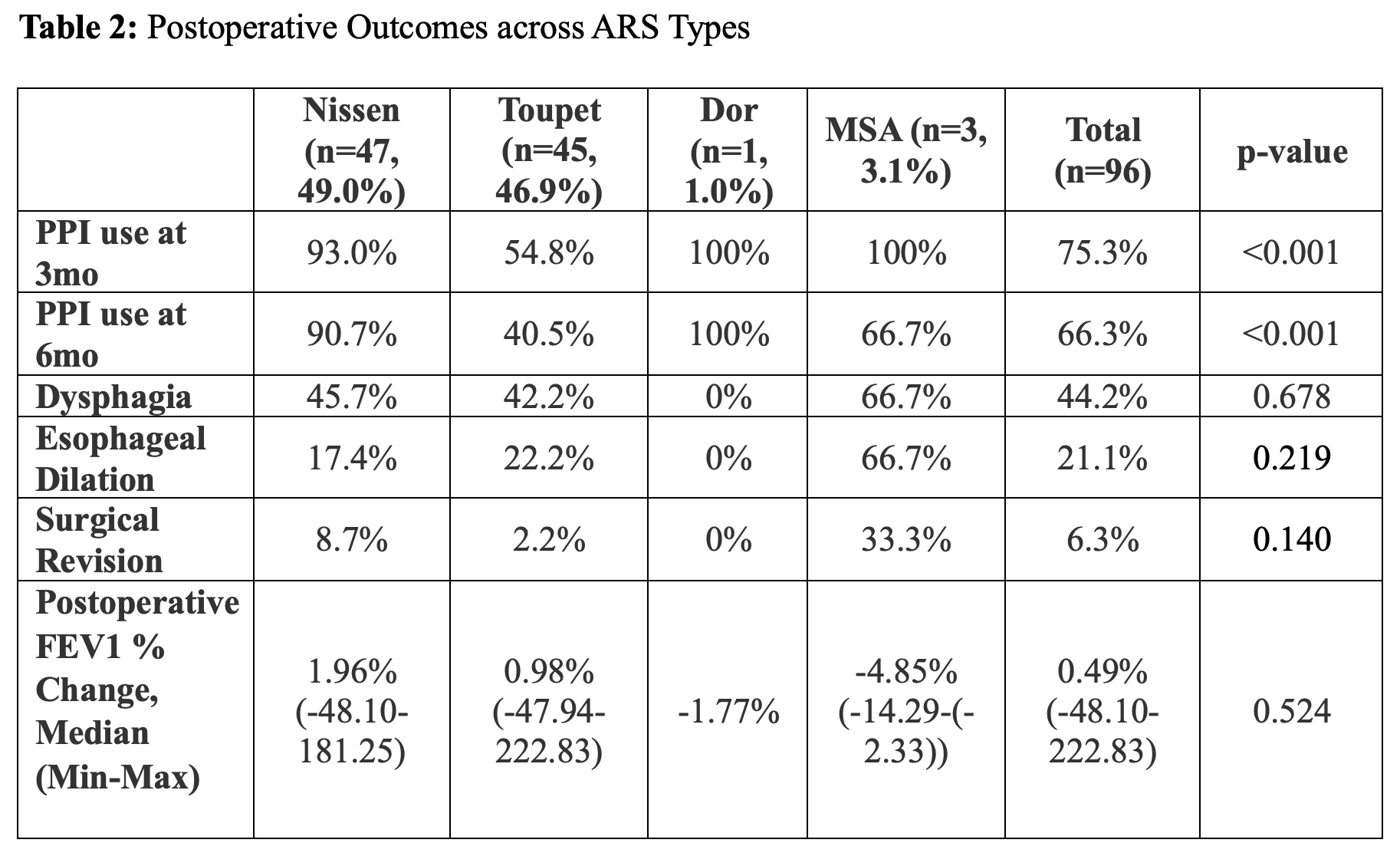
Table 2
Back to 2024 Abstracts