Back to 2024 Abstracts
LIMITED VALUE OF THE PITTSBURGH SEVERITY SCORE IN ASSESSING NEED FOR EMERGENCY ESOPHAGECTOMY FOLLOWING BENIGN ESOPHAGEAL PERFORATION
Vladimir Tverskov
2, Ory Wiesel
3, Ran Orgad
1, Hanoch Kashtan
1, Daniel Solomon
*11Surgery, Assuta Ashdod Hospital, Ashdod, South, Israel; 2Rabin Medical Center, Petah Tikva, Central, Israel; 3The Baruch Padeh Medical Center Poriya, Tiberias, Northern, Israel
Background: Benign esophageal perforations (BEP) are a rare but highly morbid occurrence, often requiring surgical management and, ultimately, emergency esophagectomy (EE) for severe cases. The Pittsburgh Severity Score (PSS) has been recently validated as a reliable predictor of outcomes among BEP patients. Limited data exists regarding its value in guiding treatment strategies and, specifically, predicting the need for EE.
Methods:Retrospective analysis of all BEP patients admitted 2011-2021. Patients who underwent esophageal resection were compared to patients who underwent organ-preserving management.
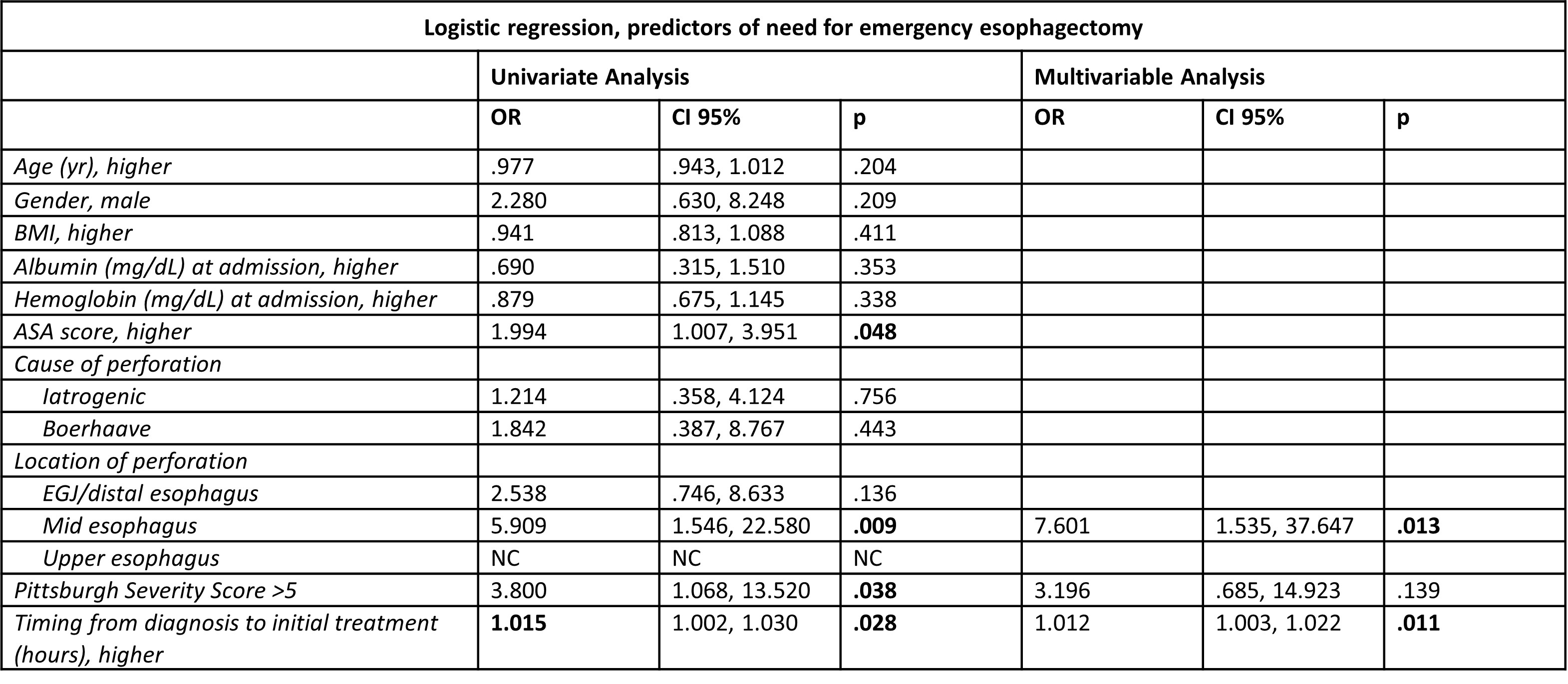
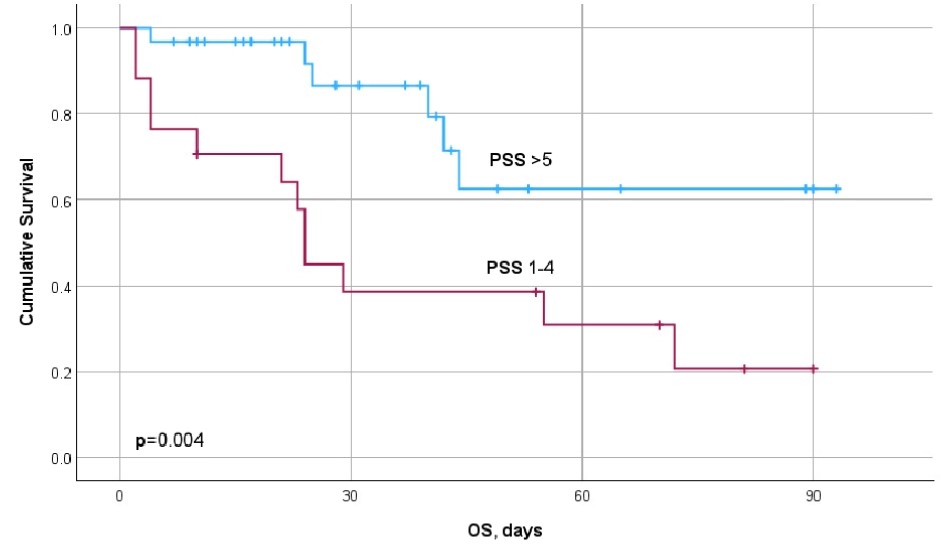
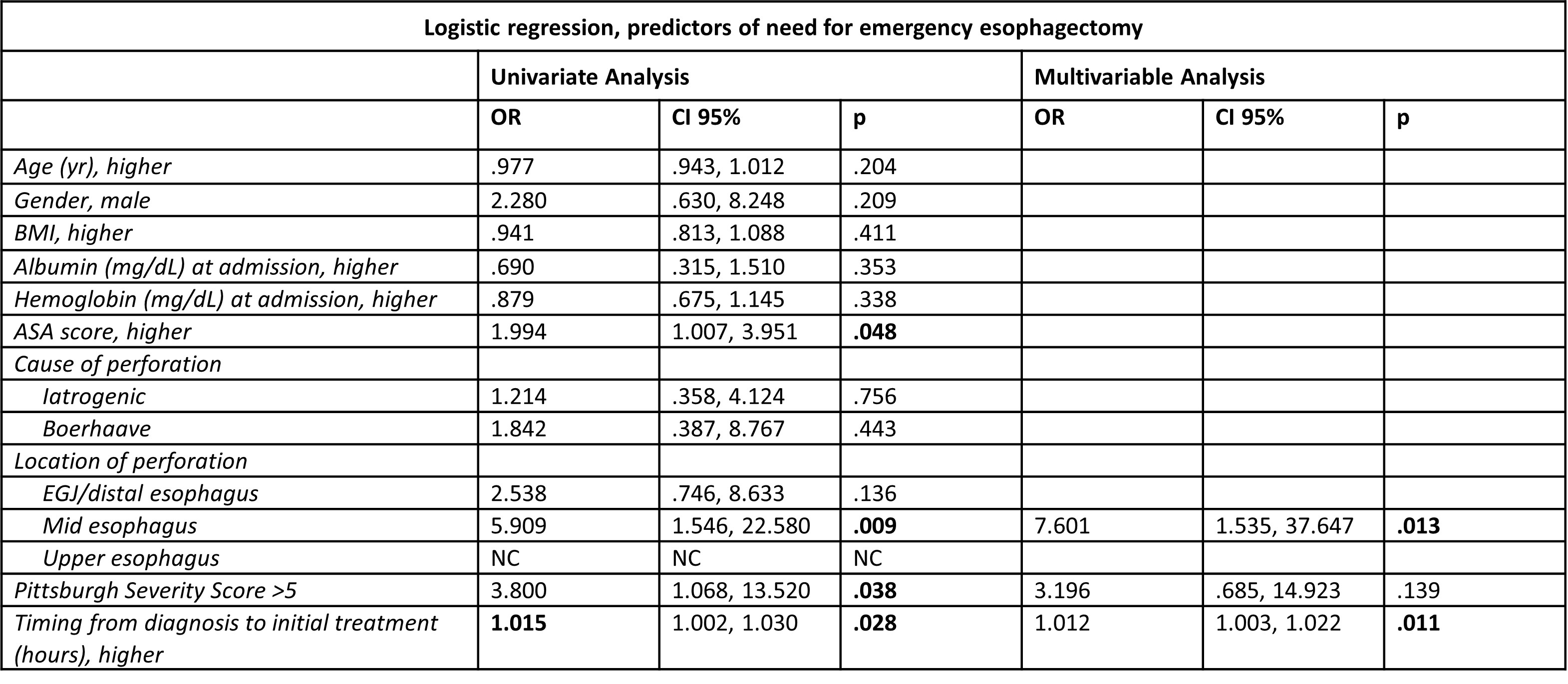
Results:Forty-eight BEP patients were included in the analysis. Cause of perforation was iatrogenic in 33 patients (68.8%), Boerhaave syndrome in 8 (16.7%), caustic ingestion in 4 (8.3%). The perforation was located in the distal esophagus in 17 cases (35.5%), mid esophagus in 17 (35.4%), and upper esophagus in 14 (29.2%). Overall, 14 patients underwent EE (29.2%) as an initial treatment choice, and 10 more patients underwent resection following failure of organ-preserving strategies. Demographic and baseline variables were comparable among the resected vs non-resected cohorts. At initial presentation, mid esophageal perforations were more common (n=13, 54.2% vs n=4, 16.7%, p<0.001), PSS scores were higher (median, IQR1-3 5.5, 4-7.5 vs 3, 2-5, p=0.016), and time to initial treatment was longer (median hrs, IQR 1-3 48, 7-114 vs 12.5, 2-20.8, p=0.007) among EE patients. A subgroup analysis on patients who received initial organ-preserving strategies confirmed that subsequent esophagectomy was more common among mid esophageal perforations (p=0.008), high PSS patients (p=0.038), and with longer time to initial treatment (p=0.004). On Kaplan Meier analysis, patients with PSS>5 had poorer OS at 90 days than their counterparts (median OS, CI 95% 24 months, 22.1-25.9 vs not reached, p=0.004). On multivariable logistic regression, only mid esophageal location (OR 7.601, p=0.013) and longer time to initial treatment (OR 1.012, p=0.011) were independently associated with need for EE.
Conclusions:While PSS was associated with poorer OS, we did not find an independent association with the need for EE. Mid esophageal perforations and patients with later presentation were more likely to be treated with EE.
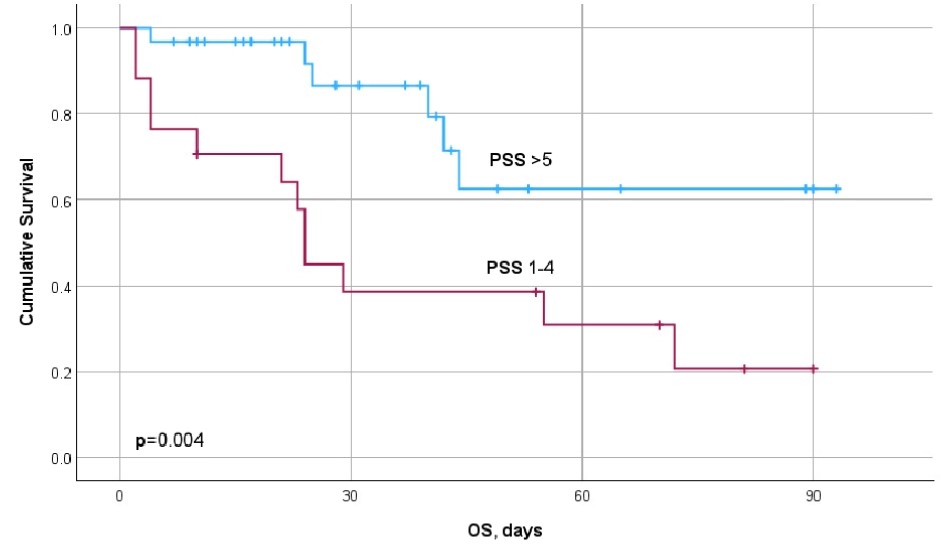
Kaplan Meier analysis for overall survival, low PSS vs high PSS
Back to 2024 Abstracts