Back to 2024 Abstracts
THE SAFETY AND TECHNICAL FEASIBILITY OF ENDOSCOPIC SUBMUCOSAL DISSECTION FOR EARLY GASTRIC CANCER AMONG PATIENTS ≥75 YEARS OF AGE – A SYSTEMATIC REVIEW AND META-ANALYSIS
Maryam Rafaqat Hussain
*2, Faisal S. Ali
1, Brian Downer
2, Vaibhav Wadhwa
1, Tomas DaVee
1, Nirav Thosani
21The University of Texas Health Science Center at Houston, Houston, TX; 2The University of Texas Medical Branch at Galveston, Galveston, TX
Introduction
There is a lack of consensus on the safety and efficacy of endoscopic submucosal dissection (ESD) for the treatment of early gastric cancer among elderly patients.
Methods
A systematic review to identify the impact of ESD on individuals aged ≥75 years was performed. A meta-analysis of safety and efficacy-related outcomes was performed to compute a risk ratio (RR) with their corresponding 95% confidence intervals. Influence analyses were done to assess the robustness of our findings. Certainty was assessed using the GRADE approach.
Results
We included 15 studies, with a mean age difference of 17.85 years between elderly and control arms. Elderly patients had larger lesions (mean 1.77 mm; 1.13, 2.40 mm) compared to control. On subgroup analysis, the difference in lesion size was significant only for patients ≥80 years of age and controls (mean 2.66 mm; 0.83, 4.50 mm). No significant disparities were observed in procedure time or length of stay (LOS) for elderly and control arms, regardless of age group.
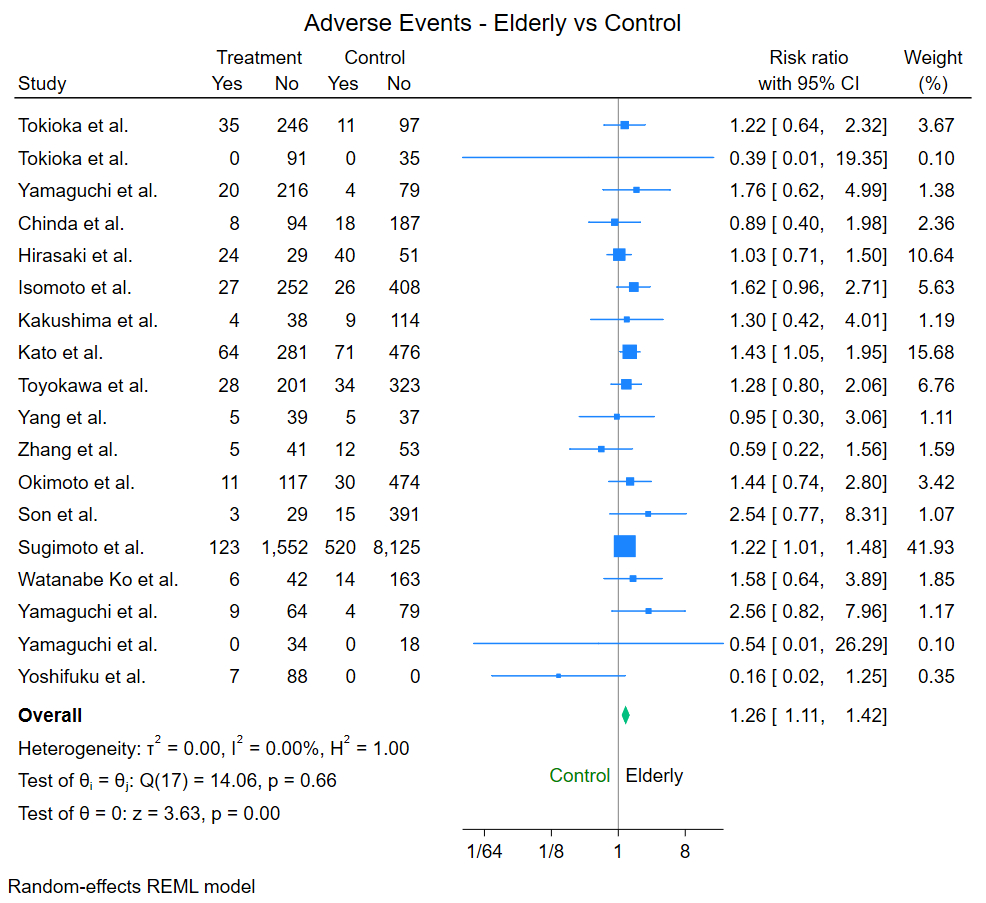
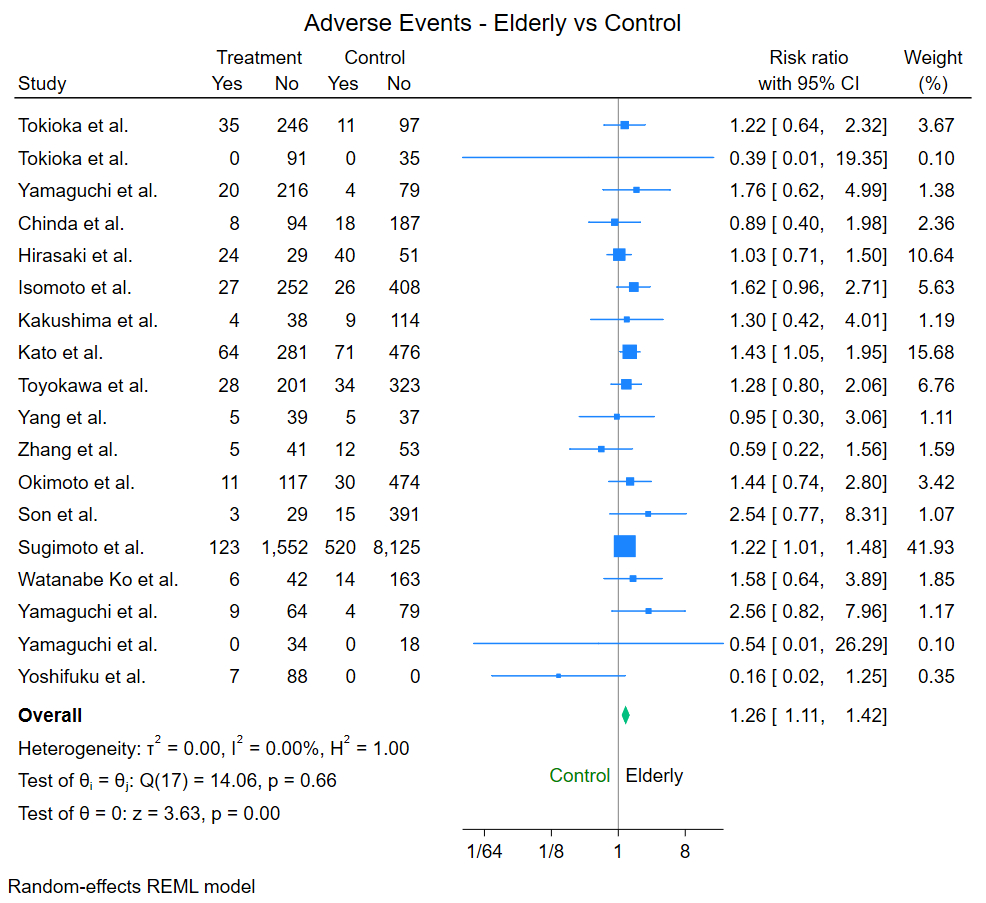
Procedural efficacy, assessed by en bloc and complete resection rates, did not differ significantly between elderly and control arms. However, Elderly patients had a higher risk of adverse events (RR: 1.26; 1.11, 1.42; I2 0%; CERTAINTY: LOW). Subgroup analysis revealed higher risk for patients ≥75 years (RR: 1.23; 1.03, 1.48; I2 0%; CERTAINTY: LOW) and ≥80 years (RR: 1.27; 1.07, 1.51; I2 0%; CERTAINTY: LOW), but not for patients 65-75 years compared to controls. The risk of post-procedural bleeding was higher in elderly patients (RR: 1.20; 1.03, 1.40; I2 0% CERTAINTY: LOW) and significantly higher for patients ≥80 years (RR: 1.28; 1.04, 1.57; I2 0%; CERTAINTY: LOW), but not for patients ≥75 years or 65-75 years compared to controls.
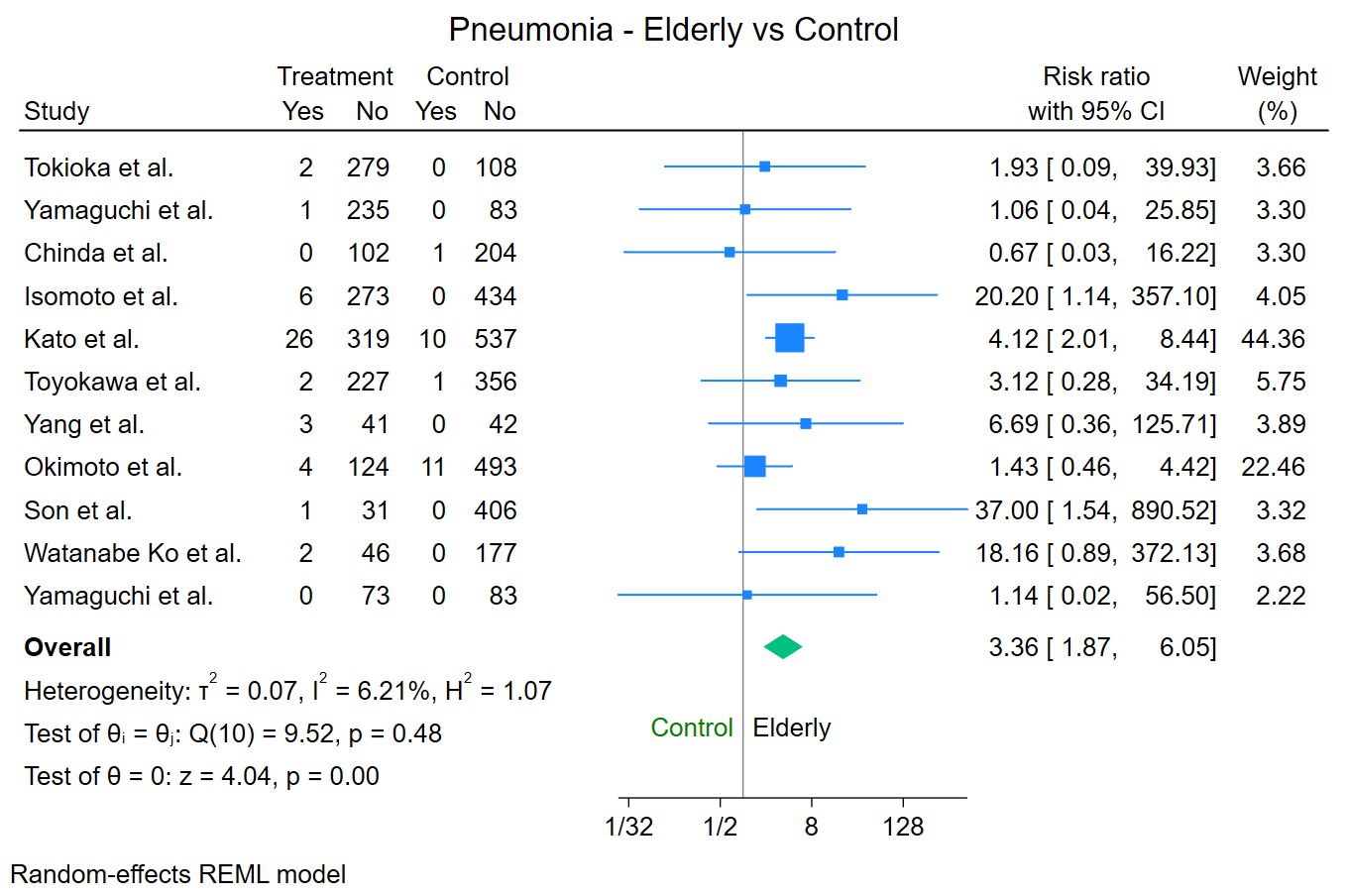
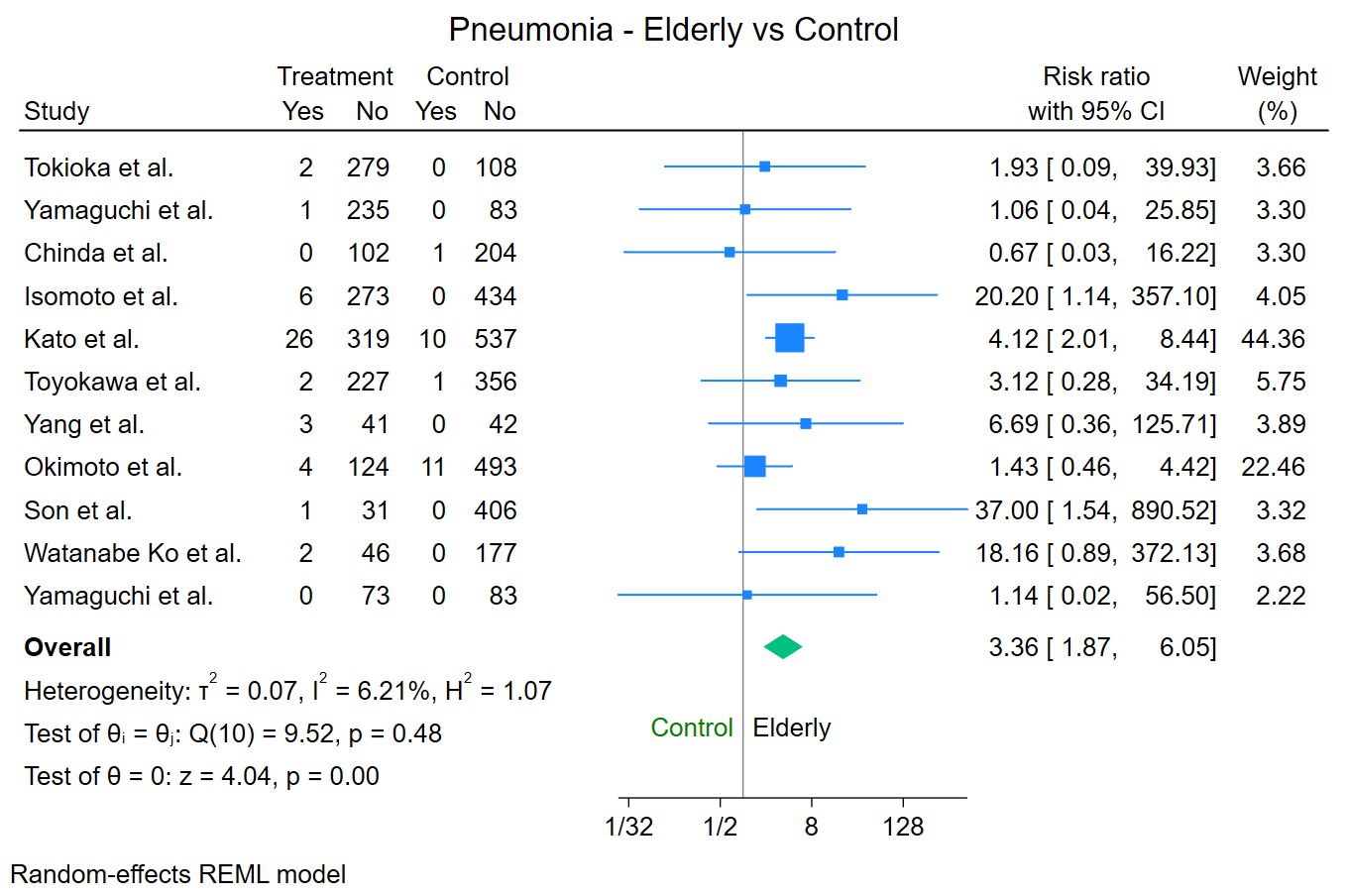
The risk of post-operative pneumonia was higher in elderly patients (RR: 3.36; 1.87, 6.05; I2 6.2%; CERTAINTY: MODERATE). Subgroup analysis showed significantly higher risk for patients ≥75 years (RR: 4.16; 2.20, 7.87; I2 0%; CERTAINTY: MODERATE), with continued significance on influence analysis. Patients ≥80 years did not exhibit a higher risk, but influence analysis revealed significance with the removal of one study (RR: 12.10; 1.79, 81.75). Patients 65-75 years did not have a higher risk of post-operative pneumonia compared to controls.
No significant difference in luminal perforation rate was observed between elderly and control arms in pooled or subgroup analyses Data on procedural mortality was insufficient to perform a meta-analysis.
Conclusion
In patients ≥75 years of age, ESD for early gastric cancer increased the risk of post-operative pneumonia compared to their younger counterparts based on moderate certainty evidence. These findings warrant further study of the risk factors for development of pulmonary events and pneumonia after gastric ESD to allow better patient selection and preventive efforts.
Back to 2024 Abstracts