Back to 2024 Abstracts
BOTULINUM TOXIN PYLOROPLASTY TO REDUCE POST-OPERATIVE NAUSEA AND VOMITING AFTER SLEEVE GASTRECTOMY: A PILOT RANDOMIZED TRIAL
Grishma Pradhan
*, Tyler Robinson, Ashar Ata, Tejinder P. Singh, Jessica Zaman
General Surgery, Albany Medical Center, Albany, NY
Background: Postoperative nausea and vomiting (PONV) is common after sleeve gastrectomy (SG). Chemical pyloroplasty (CP) using botulinum toxin benefits patients after esophagectomy or with gastroparesis by relaxation of the pylorus. Prior retrospective analysis studying chemical pyloroplasty (CP) using botulinum toxin after SG demonstrated some benefit in length of stay and staple line leak warranting further study in a randomized fashion.
Methods: We
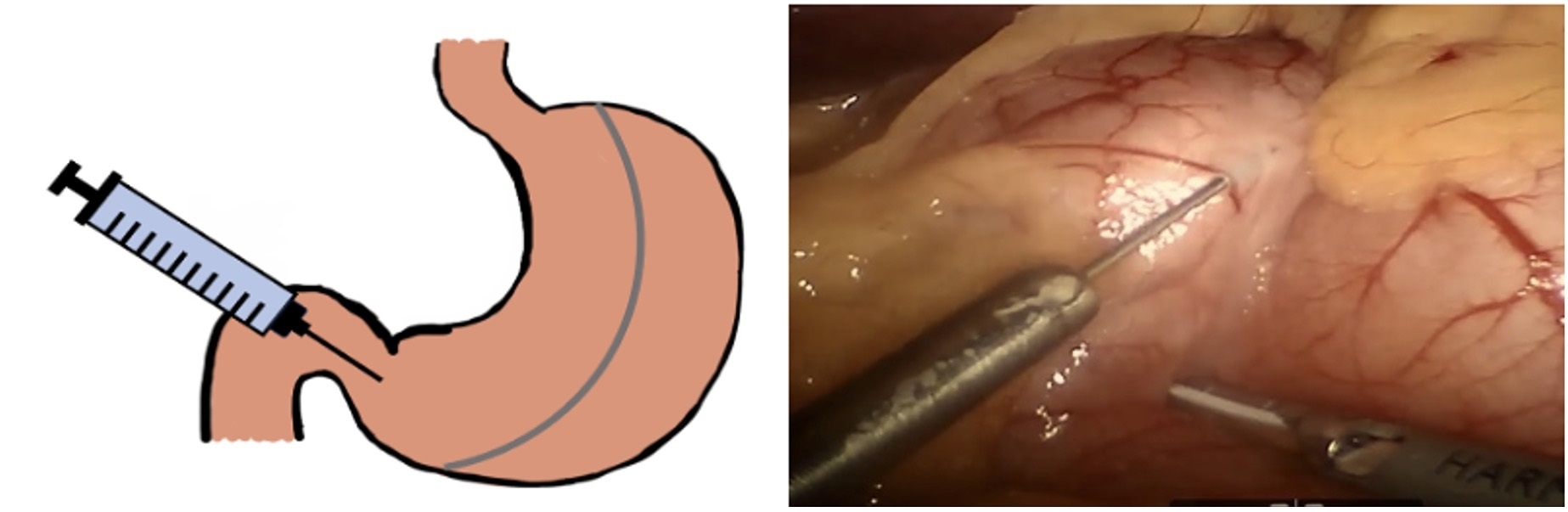
conducted a prospective, double-blinded, randomized control trial with patients undergoing SG from January 2019 to May 2022. At the completion of the sleeve, patients received either 100 U of botulinum toxin suspended in saline or saline alone. The injection is performed with a laparoscopic needle just proximal to the pylorus (Figure 1). Primary outcomes assessed were post-operative anti-emetic usage and hospital length of stay. Secondary outcomes included patient-reported nausea scores, postoperative use of antiemetic medications, 30-day hospital readmission rate and complication rate.
Results: Fifty-seven patients were randomized into the protocol, 28 had CP and 27 had no CP. There were no significant differences in patient characteristics between the two cohorts (age, gender, obesity-related comorbidities, or preoperative BMI). The addition of CP intra-operatively did not impact operative times (106.3 for CP vs. 106.8 mins for no CP, p=0.94) and no intra-operative complications occurred for either group. Anti-emetic usage was equivalent in the study and placebo arms (48.5% CP vs. 51.5% no CP, p=0.91). Hospital length of stay was not impacted by the intervention (2.65 vs. 3.46 days, p=0.40), There were no differences in inpatient or outpatient PONV scores. Need for postoperative outpatient hydration was similar in both groups (21.42% CP vs. 10.34% no CP, p=0.25).
Conclusion: Intraoperative CP during SG can be performed safely and efficiently but did not add substantial benefit when routine enhanced recovery measures were employed. It is possible that the delayed onset of botulinum toxin as demonstrated in other operations such as complex abdominal wall reconstruction may make CP more effective when administered 2-4 weeks before surgery during pre-operative endoscopy. Limitations include low power due to restrictions on bariatric surgery during the pandemic leading to a barrier in recruitment.
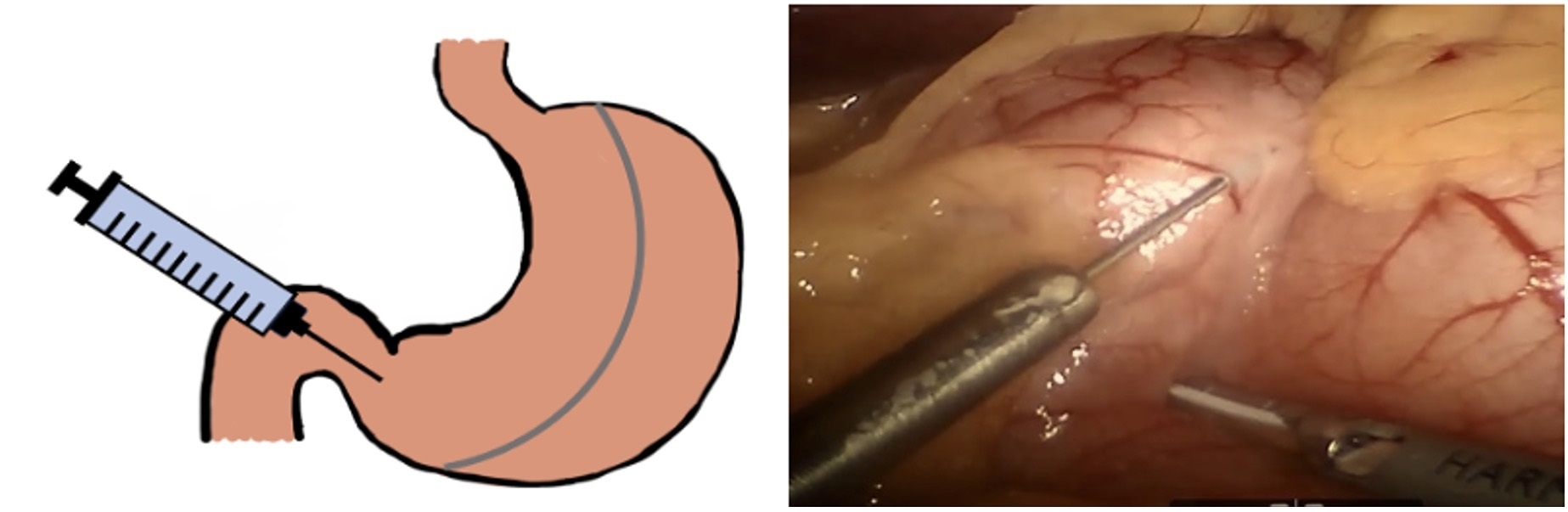
Figure 1. Mock-up and laparoscopic view of chemical pyloroplasty performed laparoscopically
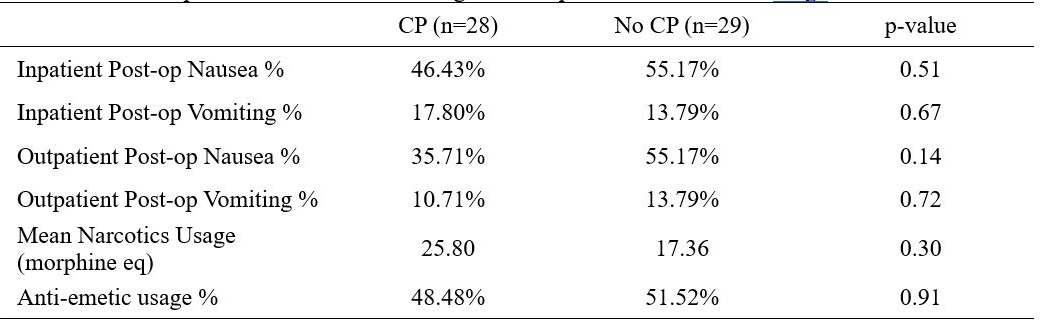 Table 1:
Table 1: Postoperative nausea and vomiting with morphine and anti-emetic usage
Back to 2024 Abstracts