Back to 2024 Abstracts
DIFFERENCES IN PATIENT OUTCOMES CANNOT EXPLAIN HIGHER MORTALITY FROM GASTRIC ADENOCARCINOMA IN RACIAL/ETHNIC POPULATIONS: AN ANALYSIS OF THE NCDB
Alexandra Adams
*1, Brijesh Rana
1, Brett L. Ecker
1, Mariam F. Eskander
1, Timothy Kennedy
1, Miral S. Grandhi
1, Russell Langan
1, Henry A. Pitt
1, Haejin In
1,21Surgical Oncology, Rutgers Cancer Institute of New Jersey, New Brunswick, NJ; 2Rutgers School of Public Health, Piscataway, NJ
Introduction:
Racial/ethnic minority populations in the US die from gastric cancer (GC) at roughly double the rate compared to non-Hispanic white (NHW) populations. We investigated if differences in sociodemographic variables, tumor characteristics, or receipt of treatment among patients diagnosed with GC contribute to the higher rates of mortality from GC in racial/ethnic populations.
Methods:
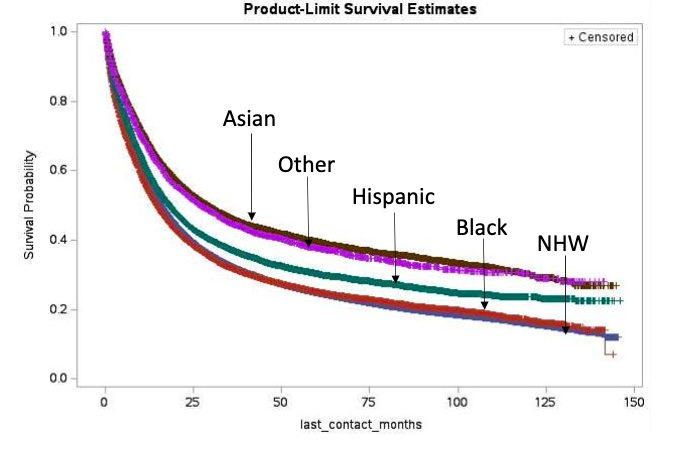
The National Cancer Data Base (NCDB) was used to identify patients with diagnosed with gastric adenocarcinoma between 2010-2020 (n=134,783). Race/ethnicity was examined as NHW, non-Hispanic Black, Hispanic, and Asian. Descriptive and inferential statistics were performed. Cox proportional hazard models and Kaplan Meier survival curves were used to analyze the effect of race/ethnicity on survival adjusting for demographic and tumor characteristics and receipt of therapy.
Results:
Among patients diagnosed with GC, 64.93% of patients were NHW, 13.98% of patients were Black, 10.43% were Hispanic, and 7.92% were Asian. NHW patients were more likely to be male, older, have insurance, live in areas with high rates of education, have cardia cancer and favorable tumor characteristics compared to patients of other race/ethnicities. Black patients had the highest rate of comorbidities amongst all race/ethnic groups. Hispanic patients were more likely to be young, uninsured, and live in areas with low rates of education. They were also more likely to have unfavorable tumor characteristics (high grade tumors 44.9% vs 38.5%; signet ring cell histology 32.4% vs 18.7%) and present with stage 4 disease (41.4% vs 33.6%) compared to NHW. Asians had the least comorbidities amongst the racial groups. They were more likely to present with unfavorable tumor characteristics yet the most likely to present with stage I (22.3% vs 17.8% for NHW). Rates of receipt of any treatment (surgery, chemotherapy, or radiation) were similar among all race/ethnic groups.
After controlling for socio-demographics, stage, tumor characteristics, and treatment, all other race/ethnic groups had improved survival compared to NHW (Black HR: 0.94, 95% CI 0.90-0.97; Hispanic HR: 0.75, 95% CI 0.71-0.79; Asian HR: 0.73, 95% CI 0.69-0.77).
Conclusions:
Despite having more aggressive tumors and similar rates of treatment, Black, Hispanic, and Asian patients with GC have better survival compared to NHW. This suggests the higher rates of death from GC observed in racial/ethnic minority populations cannot be explained by differences in patient demographics, disease stage, or treatment among patients diagnosed with GC, but instead are largely attributable to the higher incidence of GC observed for these populations. Efforts to reduce mortality in racial/ethnic minority populations should focus on prevention and early detection of GC.
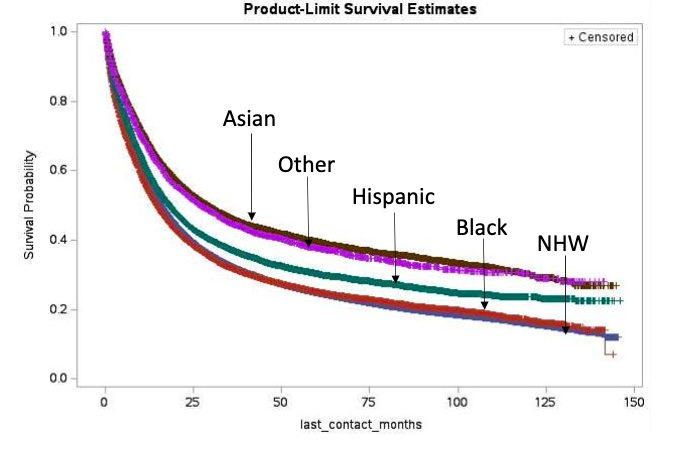
Figure 1. Overall survival for GC patients stratified by race/ethnicity
Back to 2024 Abstracts