Back to 2024 Abstracts
RESTORE OR RENOVATE? REVISIONAL ENDOSCOPIC SLEEVE GASTROPLASTY (R-ESG) VERSUS (RYGB) ROUX-EN-Y GASTRIC BYPASS FOR WEIGHT REGAIN FOLLOWING SLEEVE GASTRECTOMY (SG)
Abdellah Hedjoudje
*1, Anna C. Hoff
2, Gabriel C. Nunes
2, Sergio Barrichello
2, Induja R. Nimma
1, Vivek Kumbhari
1, Dilhana S. Badurdeen
11Mayo Clinic in Florida, Jacksonville, FL; 2Angioskope, Sao Paulo, Brazil
Background and aims: Weight regain following sleeve gastrectomy (SG) poses a significant challenge for patients and providers. Revisional endoscopic sleeve gastroplasty (R-ESG) and Roux-en-Y gastric bypass (RYGB) are treatment options. This study aims to compare the outcomes of R-ESG versus RYGB after a primary SG.
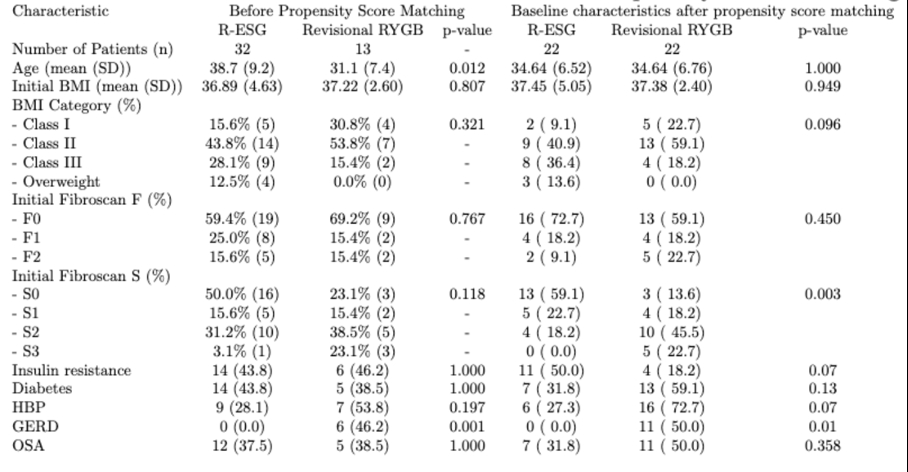
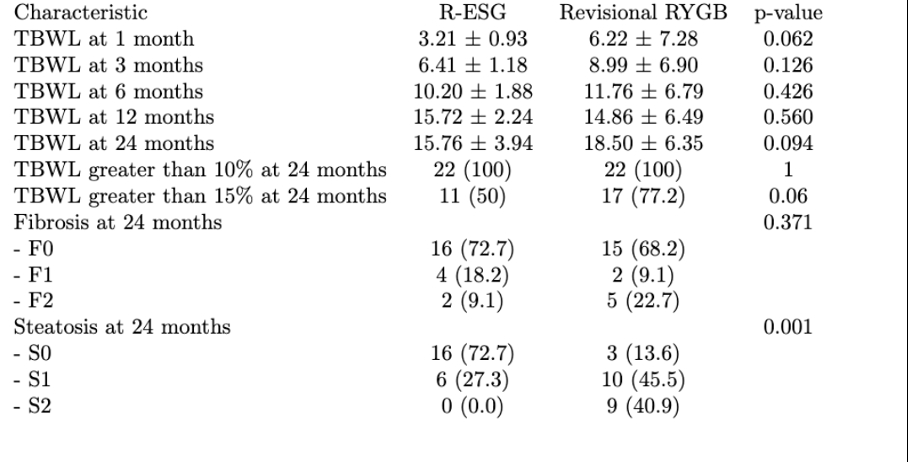
Methods: This retrospective study utilized prospectively collected data from 45 patients with suboptimal weight loss or weight regain following SG, who underwent either R-ESG or RYGB between between July 2019 and December 2021 in Sao Paulo, Brazil. Baseline patient demographics were assessed (Table 1). Percent total body weight loss (%TBWL) and excess weight loss (%EWL) were calculated. Liver steatosis and fibrosis were measured using fibroscan at 12 and 24 months. Propensity score matching was performed to reduce the imbalance between the two groups. The primary outcome was %TBWL at 12 and 24 months. Secondary outcomes were improvement in steatosis and fibrosis measured by fibroscan.
Results: A total of 45 patients were included in the analysis (32 R-ESG and 13 RYGB). Indications for conversion were suboptimal weight loss, weight regain, or gastroesophageal reflux disease (GERD). Propensity score yielded 22 matched pairs. After matching patients who opted for R-ESG were statistically younger, mean age 38.75 years vs. 31.15 years, (p=0.012) for RYGB. 46.2% of patients that underwent RYGB had GERD at baseline. Weight and BMI at baseline did not significantly differ between the two groups. Liver steatosis and fibrosis were similar at baseline for both groups. The %TBWL at all time points was higher for RYGB except at 12 months. The proportion of patients with steatosis at baseline decreased significantly in both groups at 24 months. However, the percentage of patients that reached F0 at 24 months was not significant. Patients with TBWL greater than 10% or 15% did not differ statistically between the two groups. No serious adverse events occurred with RYGB. Minor adverse events such as abdominal pain and nausea were reported for R-ESG
Conclusions: R-ESG is a viable first option for suboptimal weight loss or weight regain after SG. A higher proportion of patients that underwent R-ESG had improvement in steatosis at 24 months. Further randomized control trials are needed to confirm this finding. In patients with concurrent GERD symptoms RYGB is likely preferable.
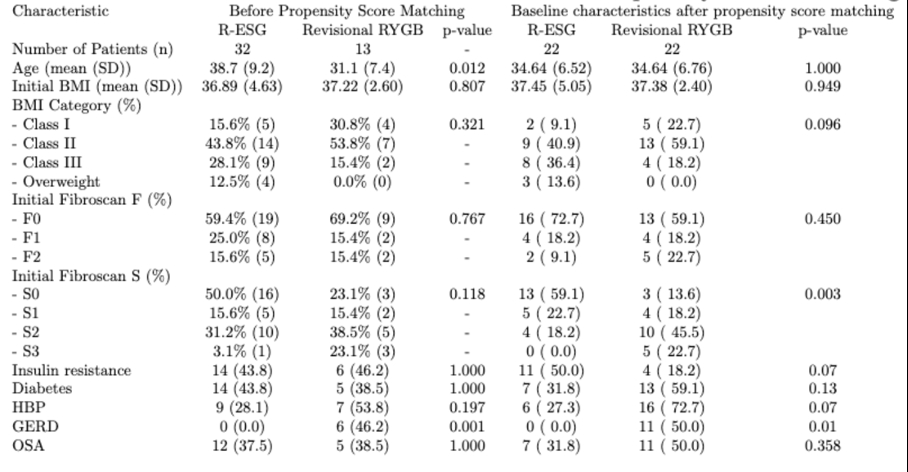 Baseline characteristics before and after propensity score matching
Baseline characteristics before and after propensity score matching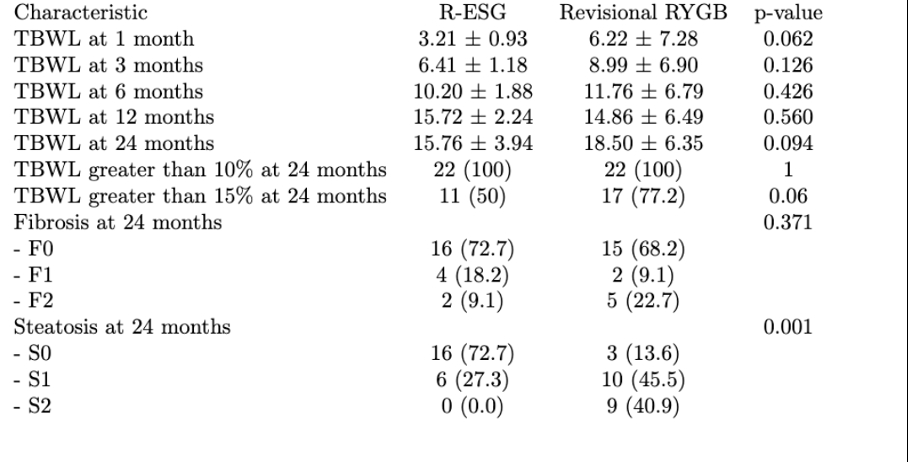
Outcomes after propensity score matching
Back to 2024 Abstracts