Back to 2024 Abstracts
IMPACT OF INSTITUTIONAL RADIOTHERAPY VOLUME ON POSTOPERATIVE AND ONCOLOGIC OUTCOMES AFTER NEOADJUVANT RADIATION FOR PANCREATIC CANCER
Raja R. Narayan
*1,2, Anne Pannekoek
1, Mengyuan Ruan
1, Ritchell van Dams
1,2, George Molina
1,21Surgery, Brigham and Women's Hospital, Boston, MA; 2Dana-Farber/Harvard Cancer Center, Boston, MA
INTRODUCTIONNearly a third of patients with pancreatic cancer (PC) recur locally after resection prompting some centers to offer neoadjuvant radiation (NRT). In contrast to its use in patients with esophageal and rectal cancer (ERC), the role of NRT to improve overall survival (OS) for PC is controversial. The aim of this study is to investigate the impact of institutional NRT volume for ERC versus PC on postoperative and oncologic outcomes after NRT and resection for PC.
METHODSAll patients undergoing NRT for histologically confirmed ERC and PC between 2011-2019 were identified from the National Cancer Database excluding those with metastases or upfront resected. Sites in the top annual decile (10%) for NRT volume treating patients with ERC and PC separately, were used as definitions for high volume NRT institutions for PC. Chi-square test examined the association of NRT volume (high versus low) with resection margins as a marker of NRT efficacy and 30-day readmission as a proxy for postoperative morbidity. Kaplan-Meier methods compared postoperative OS by institutional NRT volume using the log-rank test.
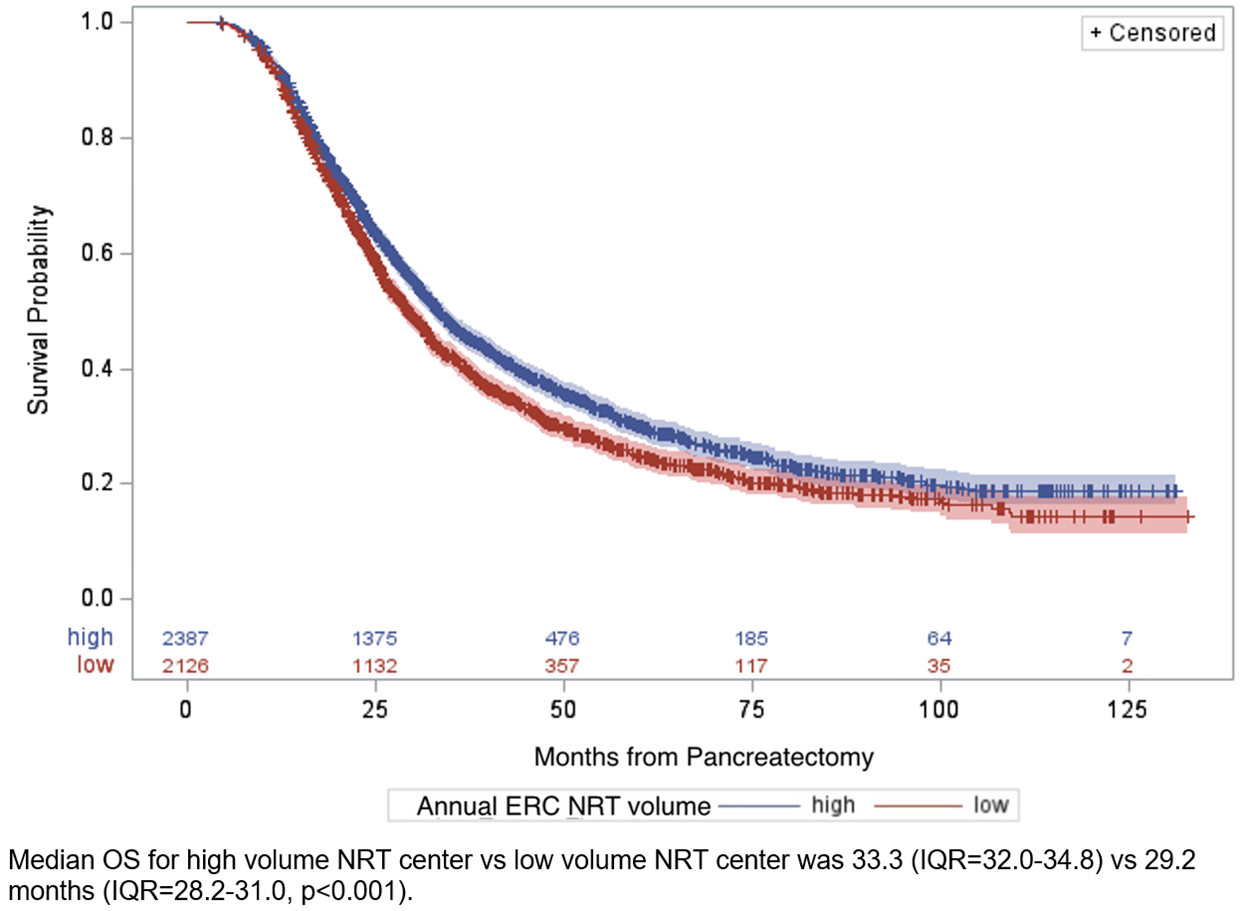
RESULTSOf 116,241 patients identified, 31,162 esophageal, 59,689 rectal, and 25,390 patients with PC were noted of which, 33.3%, 64.2%, and 17.7% underwent NRT for esophageal, rectal, and PC, respectively. The median age of patients with PC was 65 years (range=40-90) and 48.2% were female. The median annual center volume of patients with ERC versus PC undergoing NRT was 5.8 (range=1.0-138.9) versus 1.0 (range=1.0-34.0), respectively. High volume sites for ERC versus PC treated an average of 16.3 versus 3.2 patients annually comprising 52.3% versus 60.2% of nationally reported patients with PC undergoing NRT, respectively. With median follow up of 32.2 months, median OS was longer for patients with PC at high volume NRT centers for ERC (33.3 vs 29.2 months, p<0.001,
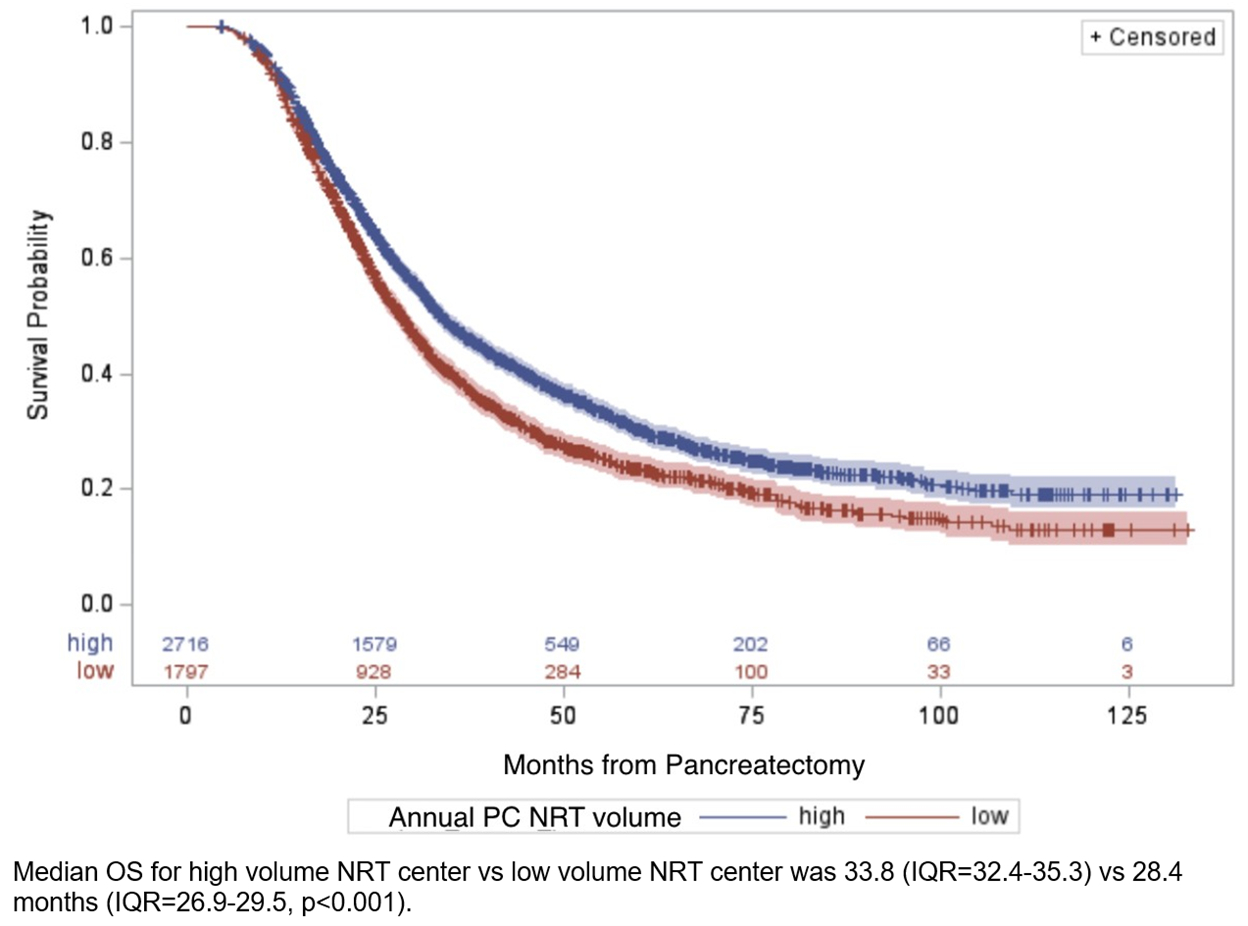
Figure 1) and PC (33.8 vs 28.4 months, p<0.001,
Figure 2). Patients with PC treated at high volume sites for PC NRT had significantly fewer margins positive (9.4% vs 14.1%, p<0.001), however ERC NRT volume did not significantly impact the positive margin rate for patients with PC (11.0% vs 11.7%, p=0.395). Compared to low volume centers, high volume NRT centers for both ERC (7.3% vs 5.5%, p=0.008) and PC (7.4% vs 5.0%, p<0.001) had higher rates of 30-day readmission in patients with PC.
CONCLUSIONSInstitutional NRT volume for PC was associated with better margin clearance and OS but increased rates of readmission at 30 days. Institutional NRT experience with ERC may not yield similar local control as experience with PC may, although this may reflect tumor biology rather than treatment efficacy. Most centers employing NRT treat few patients for PC annually. Institutional radiotherapy experience should be considered in the design of clinical trials investigating the efficacy of NRT in PC.
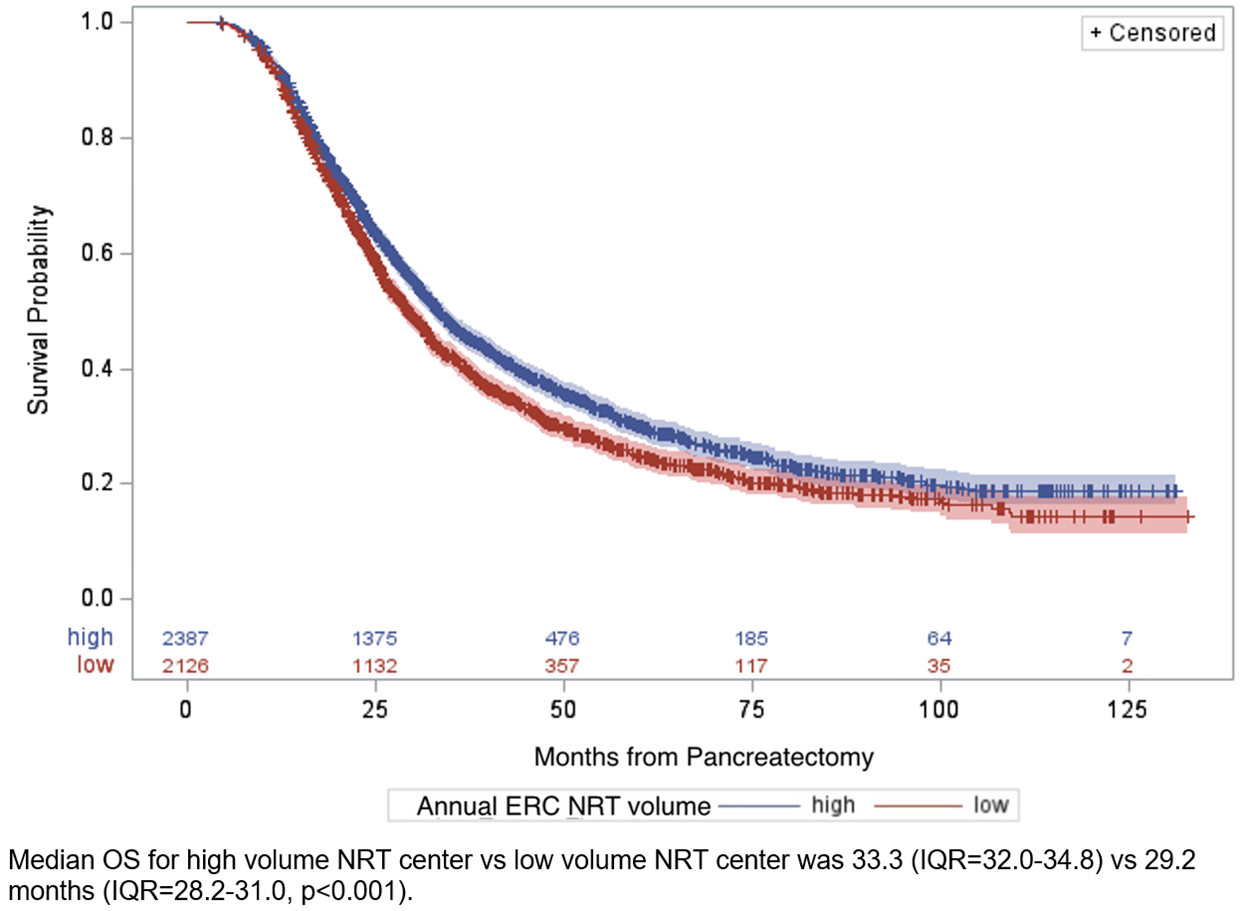 Figure 1:
Figure 1: Kaplan-Meier curves for overall survival by average annual institutional radiotherapy volume at for patients treated with neoadjuvant radiation and resection for pancreatic cancer, where high volume was defined as centers in the top 10% of patient volume for neoadjuvant radiation for esophageal and rectal cancer (high volume ≥ 16.3 patients/year).
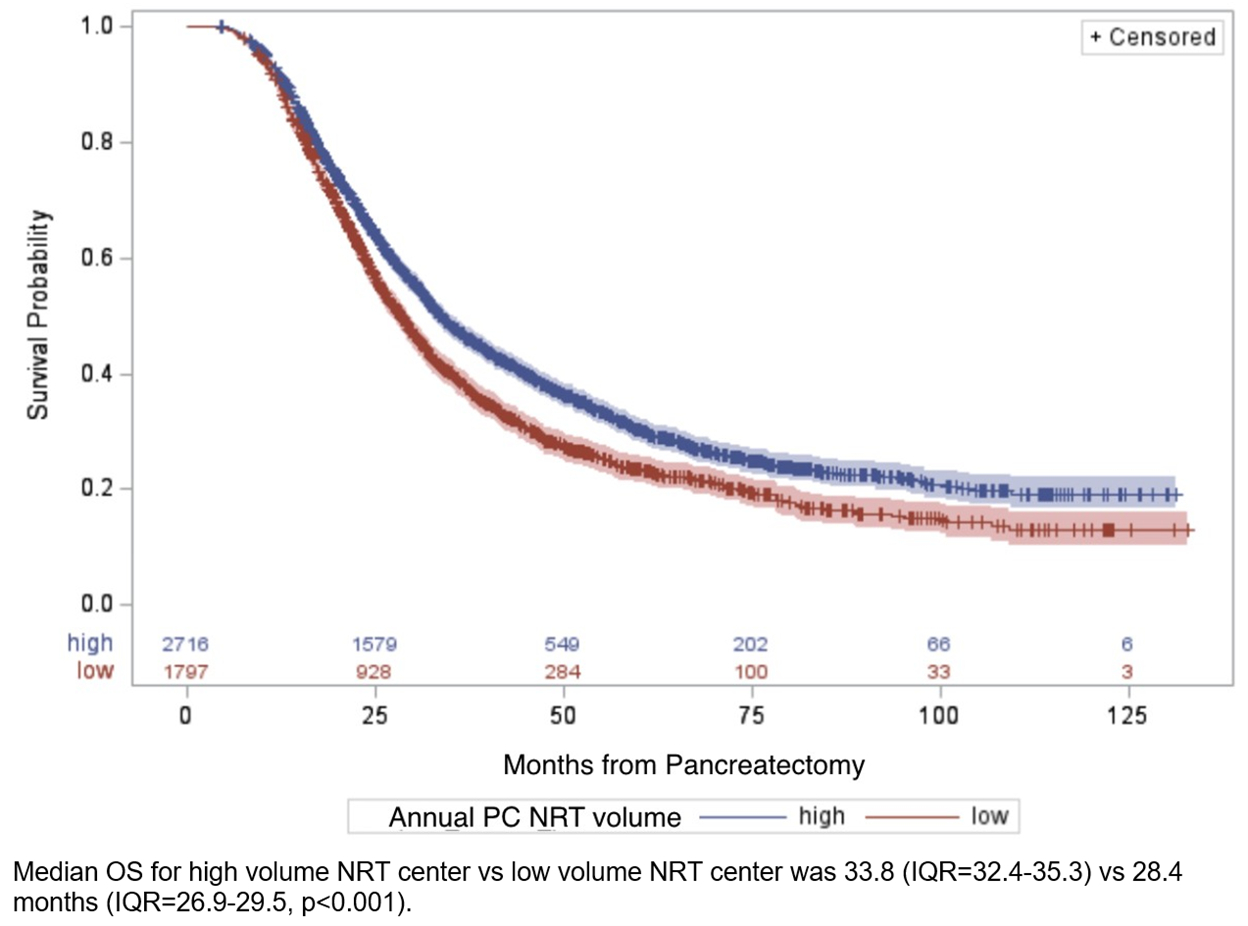 Figure 2:
Figure 2: Kaplan-Meier curves for overall survival by average annual institutional radiotherapy volume at for patients treated with neoadjuvant radiation and resection for pancreatic cancer, where high volume was defined as centers in the top 10% of patient volume for neoadjuvant radiation for pancreatic cancer (high volume ≥ 3.2 patients/year).
Back to 2024 Abstracts