Back to 2024 Abstracts
COMPARING ONCOLOGIC AND SURGICAL OUTCOMES OF ROBOTIC AND LAPAROSCOPIC PANCREATICODUODENECTOMY: A PROPENSITY-MATCHED ANALYSIS
Chase J. Wehrle
*1, Jenny H. Chang
1, Abby Gross
1, Kimberly P. Woo
1, Robert Naples
1, Kathryn A. Stackhouse
1, Fadi Dahdaleh
2, Toms Augustin
1, Daniel Joyce
1, Robert Simon
1, R Matthew Walsh
1, Samer A. Naffouje
11Cleveland Clinic, Cleveland, OH; 2Edward Elmhurst Health Marquardt Memorial Library, Elmhurst, IL
Introduction:
Minimally invasive pancreaticoduodenectomy (MIPD), or the Whipple procedure, is increasingly utilized. No study has compared laparoscopic (LPD) and robotic (RPD) approaches, and the impact of the learning curve on oncologic, technical, and post-operative outcomes remains relatively understudied.
Methods:The National Cancer Database (NCDB) was queried for patients undergoing LPD or RPD from 2010-2020. Outcomes were compared between approaches using propensity-score matching (PSM); the impact of annual center-level volume of MIPD was also assessed.
Results: A total of 3,342 patients were included. Most (n=2,716, 81.3%) underwent LPD versus RPD (n=626, 18.7%). There was a high rate (20.2%, n=719) of positive margins. Mean length-of-stay (LOS) was 10.4 ± 8.9 days. Thirty-day mortality was 2.8% (n=92) and ninety-day mortality was 5.7% (n=189).
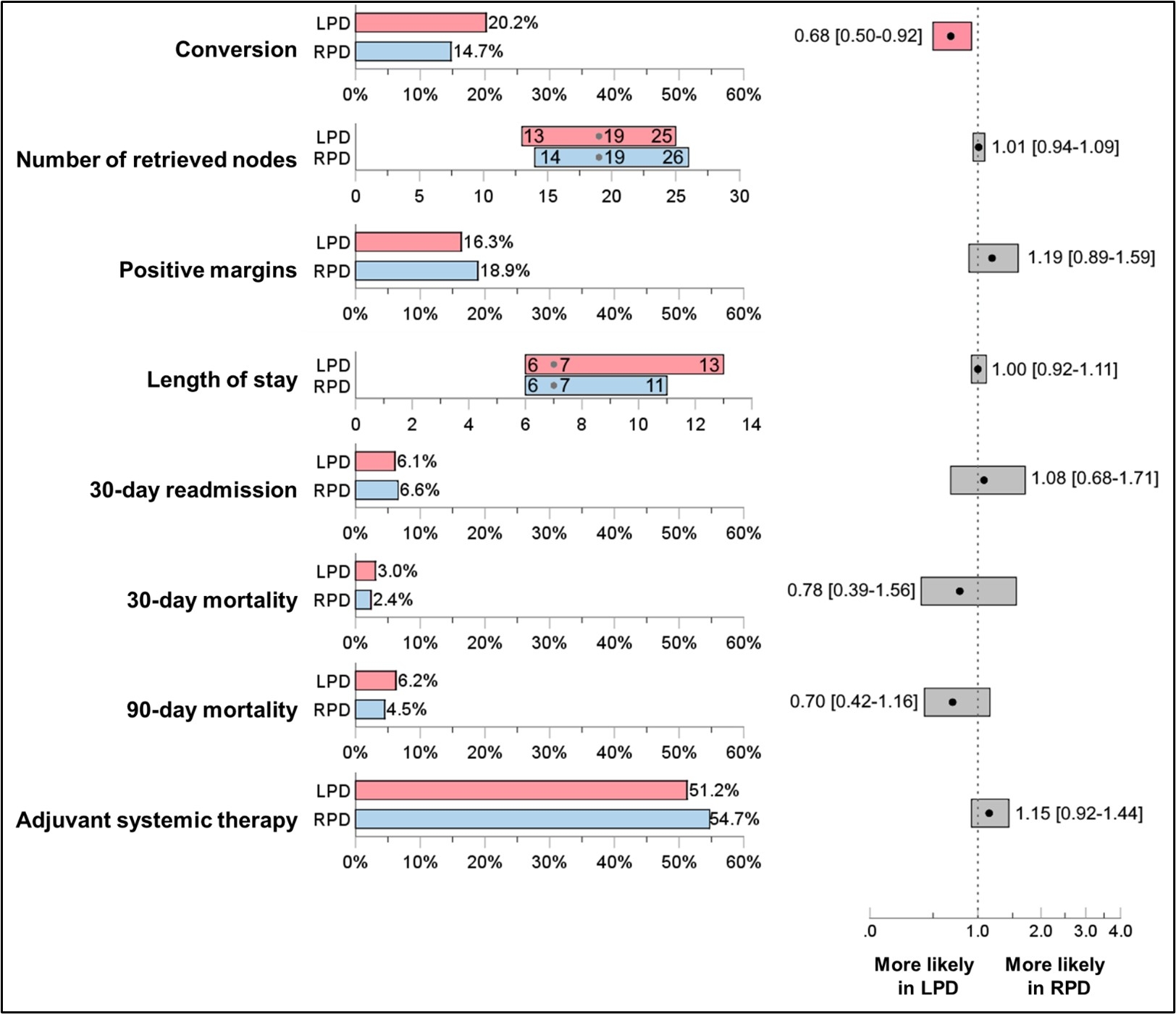
PSM matched 625 pairs of patients receiving LPD or RPD. After PSM, there was no differences between groups based on age, sex, race, CCI, T-stage, neoadjuvant chemo/radiotherapy, or type of PD. After PSM, there was a higher rate of conversion to open (HR=0.68, 95%CI=0.50-0.92)., but there was no difference in LOS (HR=1.00, 95%CI=0.92-1.11), 30-day readmission (HR=1.08, 95%CI=0.68-1.71), 30-day (HR=0.78, 95%CI=0.39-1.56) or 90-day mortality (HR=0.70, 95%CI=0.42-1.16), ability to receive adjuvant therapy (HR=1.15, 95%CI=0.92-1.44), nodal harvest (HR=1.01, 95%CI=0.94-1.09) or positive margins (HR=1.19, 95%CI=0.89-1.59).
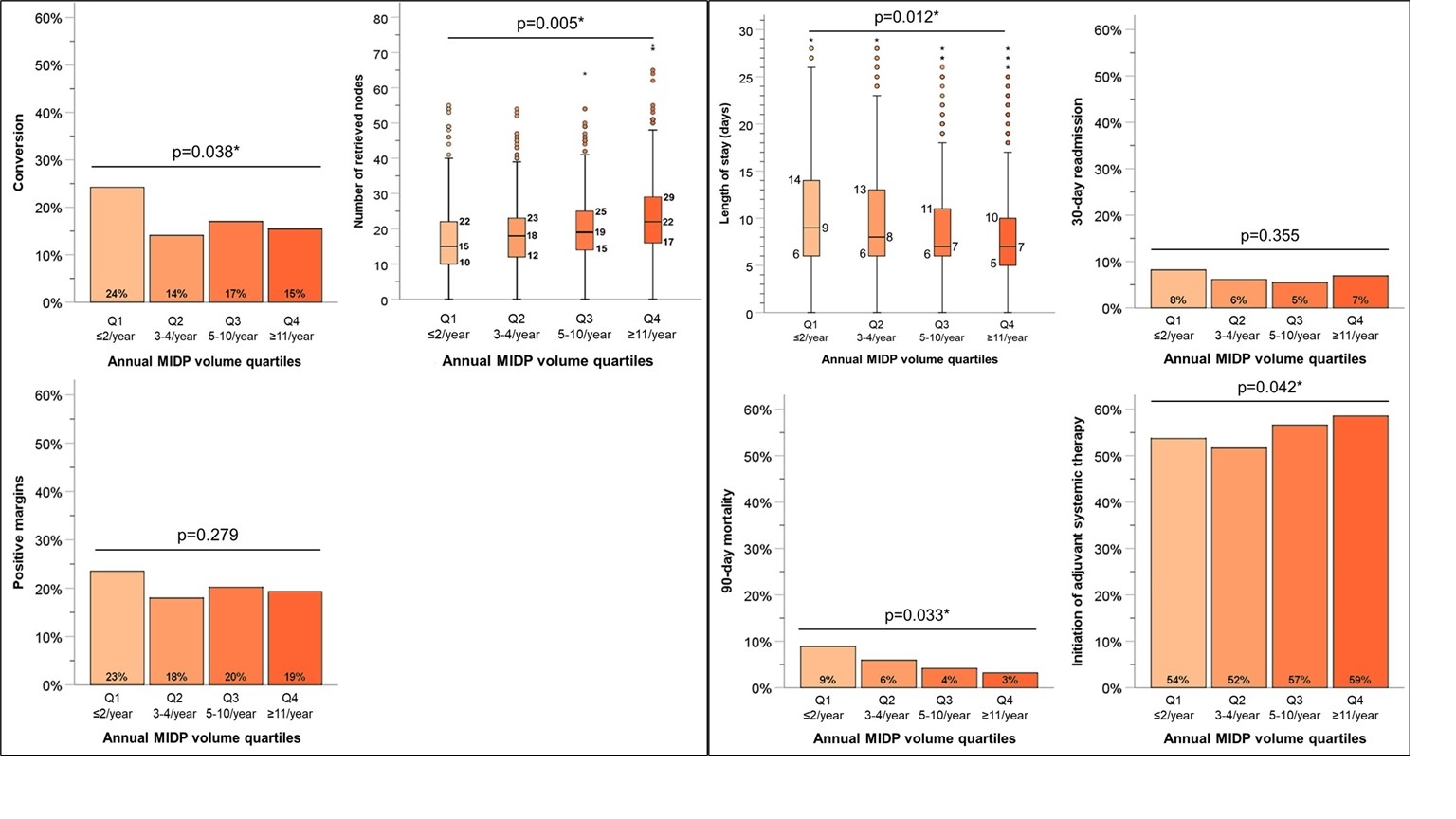
Lower annual volume of MIPD was associated with reduced nodal harvest (p=0.005) and a higher rate of conversion to open (p=0.038). Higher-volume centers had a shorter LOS (p=0.012), higher rate of initiation of adjuvant therapy (p=0.042), and, most strikingly, a reduction in 90-day mortality (p=0.033).
Conclusion:
LPD and RPD have similar surgical and oncologic outcomes, with a lower rate of conversion to open in the robotic cohort. The robotic technique does not appear to eliminate the “learning curve�, with higher volume centers demonstrating improved outcomes, especially seen at minimum annual volume of 5 cases
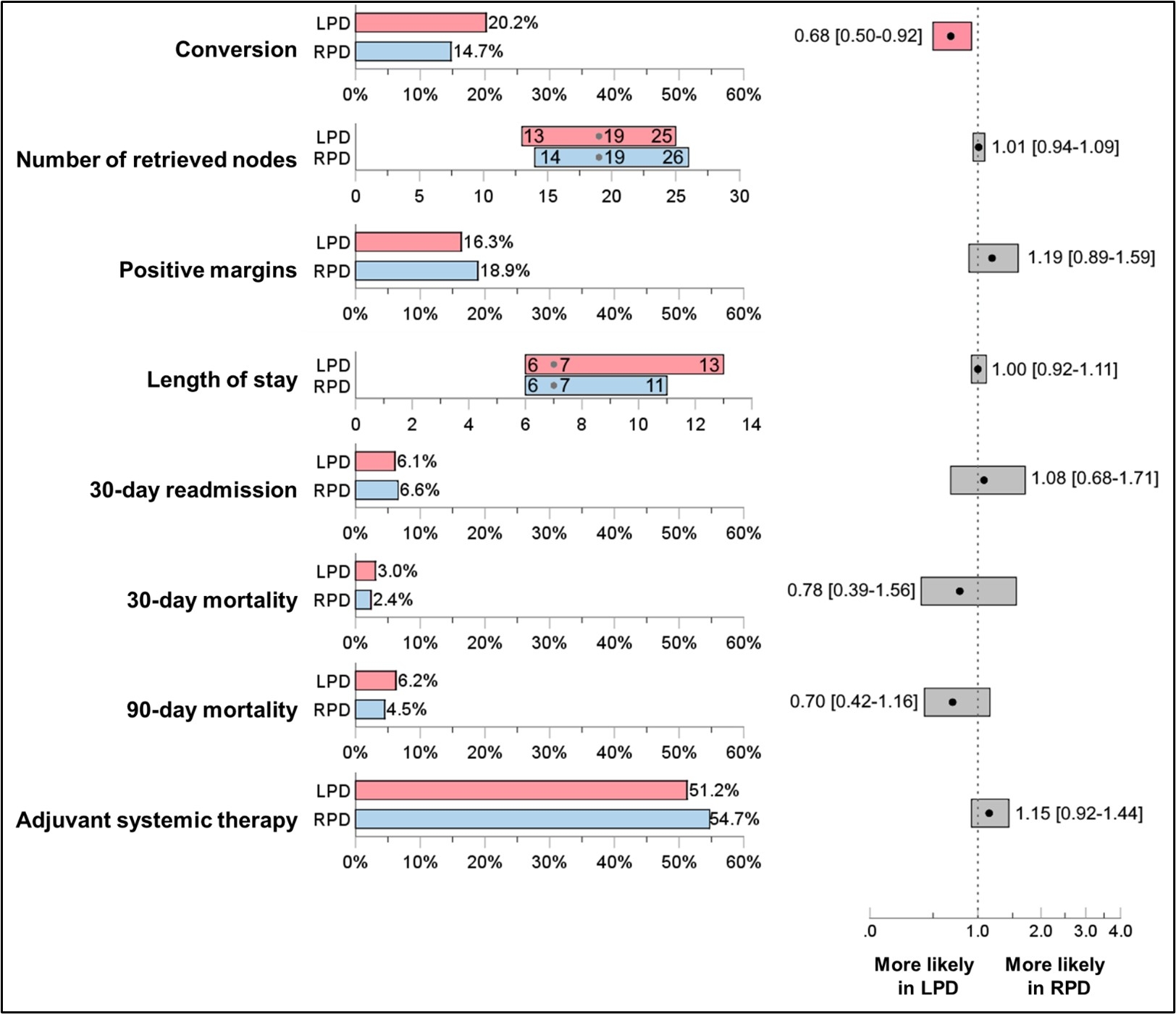 Figure 1
Figure 1: Comparison of short-term quality outcomes between the matched LPD and RPD groups.
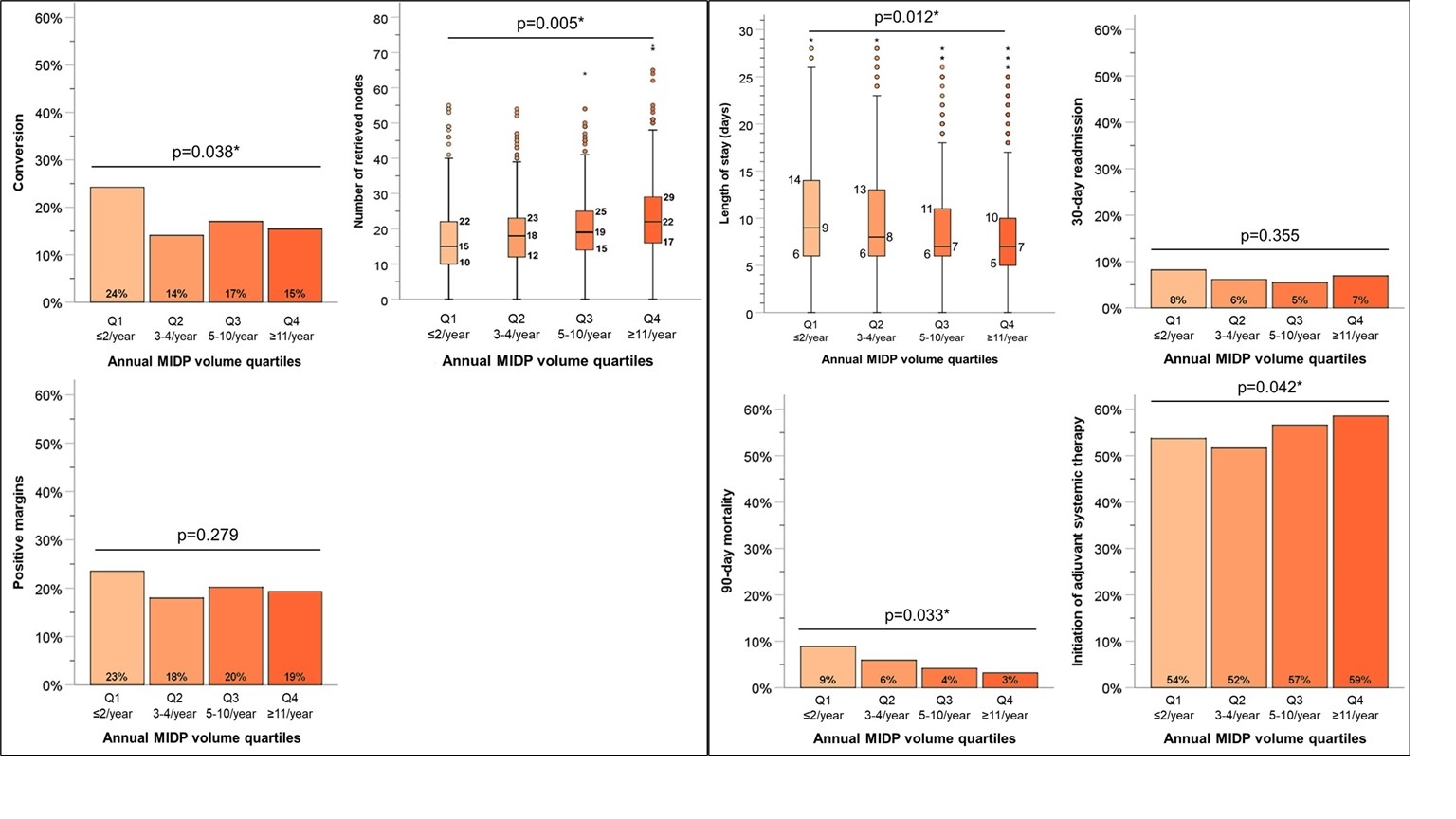 Figure 2
Figure 2:
A. Impact of annual institutional MIPD volume on technical metrics.
B. Impact of annual institutional MIPD volume on postoperative metrics.
MIPD: Minimally Invasive Pancreatoduodenectomy. * Statistically significant.
Back to 2024 Abstracts