Back to 2024 Abstracts
UNDERSTANDING FRAGMENTED PANCREATIC CANCER CARE IN PATIENTS RECIEVING NEOADJUVANT THERAPY: ARE SOCIODEMOGRAPHIC DISPARITIES PREDICTIVE OF PATIENTS RECEIVING FRAGMENTED CARE?
Maryclare E. Taylor
*1,2, Andrew B. Crocker
2, Emily Papai
1,2, Max Perilstein
1, Malek Maddah
1, Karen Ruth
2, Anthony Villano
2, Sanjay S. Reddy
21Surgery, Temple University Hospital, Philadelphia, PA; 2Fox Chase Cancer Center, Philadelphia, PA
Introduction: Fragmented Care (FC), care at multiple centers, is an emerging area of study in oncologic care. We examined a cohort of pancreatic cancer patients who received neoadjuvant therapy (NAT) to evaluate if sociodemographic disparities play a predictive role in receiving FC.
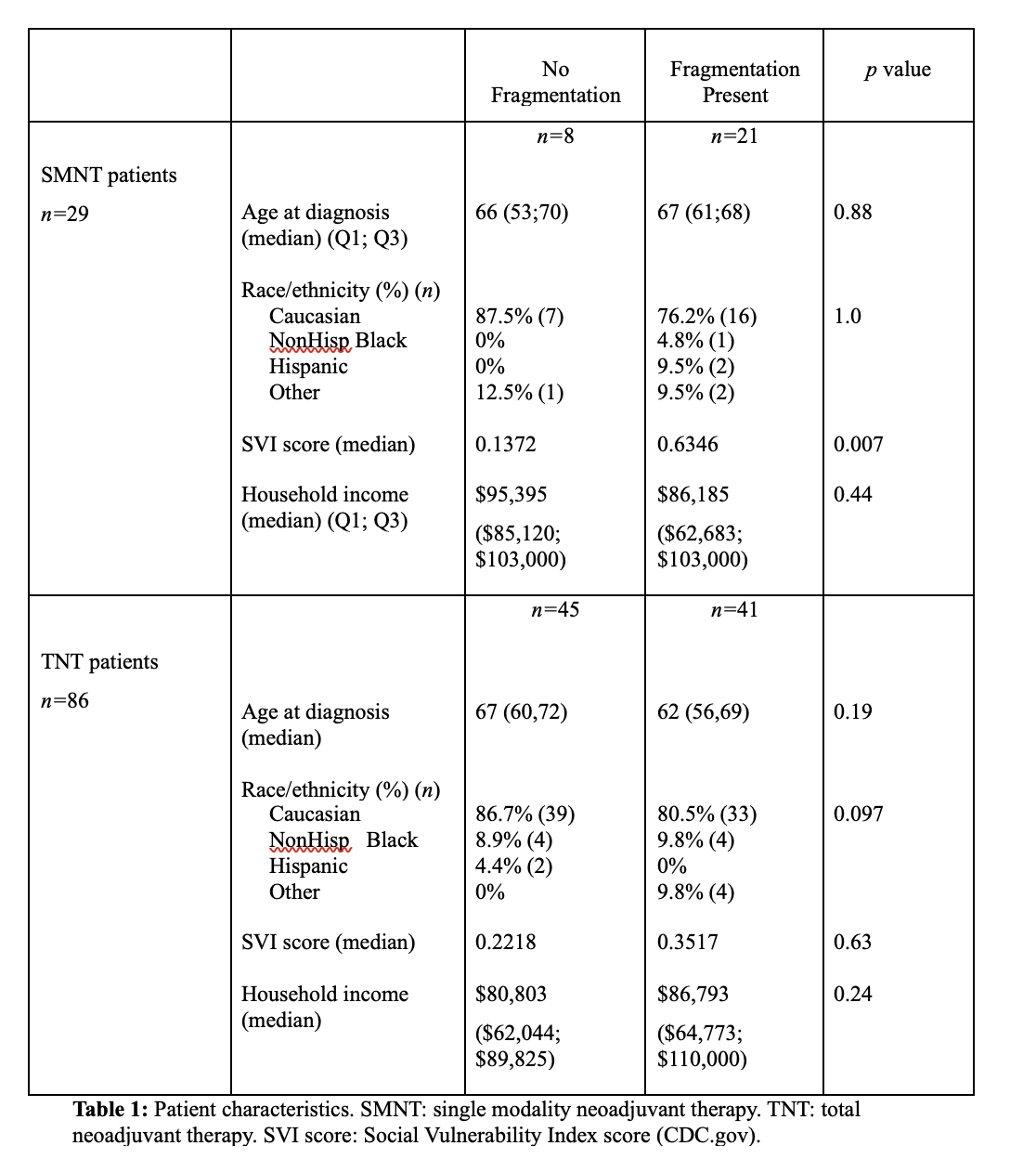
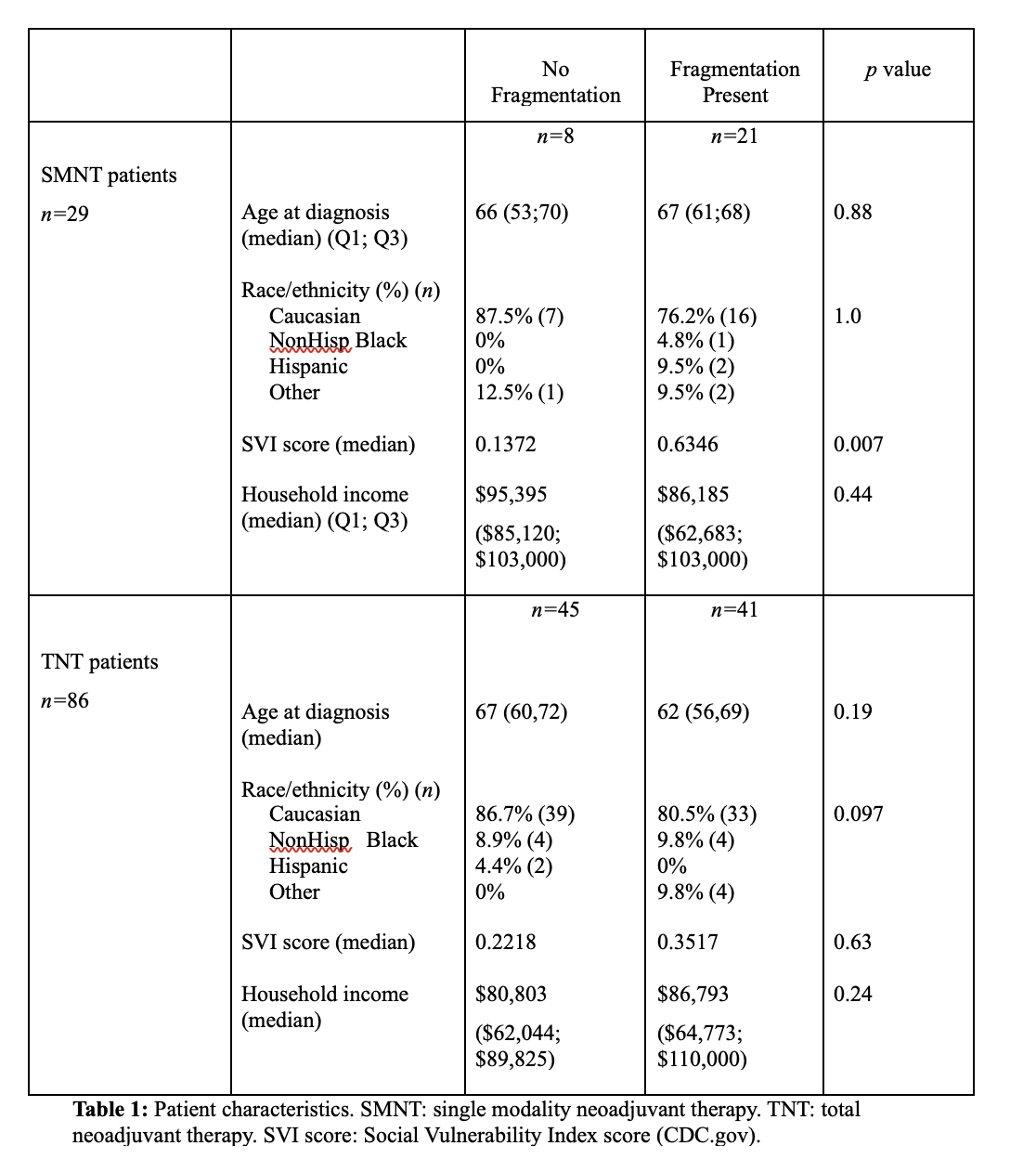
Methods: Patients with pancreatic adenocarcinoma from 2008 to 2022 who underwent NAT were queried from a single NCI designated cancer center. The cohort of NAT patients was divided into patients who received single modality neoadjuvant therapy (SMNT) or total neoadjuvant therapy (TNT). FC was defined as patients who received any aspect of care including diagnosis, chemotherapy, chemoradiation, or surgery at more than one institution. Characteristics assessed included age at diagnosis, race/ethnicity, median household income (MHI) (from census.gov), and social vulnerability index (SVI) score (CDC.gov scale of socioeconomic status, household characteristics, minority status, and housing/transportation per county). SVI score is graded on a scale of 0 to 1 with 0 the lowest and 1 the highest vulnerability.
Results: Out of 256 patients with pancreatic adenocarcinoma, 115 patients received NAT. 29 patients (25%) had SMNT and 86 patients (75%) had TNT. Patients who received SMNT were more likely to experience fragmentation of care than those who received TNT with 72% of SMNT patients experiencing FC as opposed to 48% of TNT patients (
p=0.03). When the SMNT and TNT groups were compared for differences in sociodemographic disparity predictors, no statistically significant difference was found between the median age, race/ethnicity, MHI, or SVI score. Among the SMNT cohort, SVI score was higher amongst patients who experienced fragmented care (median 0.6346 vs 0.1372,
p=0.007), indicating a higher level of vulnerability per county in the SMNT patients who received FC. There were no differences in sociodemographic variables (age, SVI, race/ethnicity, income) amongst the TNT cohort (all
p>0.05).
Conclusion: Recognizing how sociodemographic disparities impact fragmentation of care is pivotal in the understanding of how this newly emerging concept of FC affects cancer patients. When patients with pancreatic cancer who underwent NAT were evaluated, social vulnerability per country, measured by SVI scale, was associated with FC in patients who received SMNT. Patients who received SMNT more frequently received FC than patients who received TNT.
Back to 2024 Abstracts