Back to 2024 Abstracts
NEOADJUVANT CHEMOTHERAPY VERSUS UPFRONT SURGERY IN RESECTABLE PANCREATIC DUCTAL ADENOCARCINOMA: A NATIONAL CANCER DATABASE INTENTION-TO-TREAT ANALYSIS
Joanna T. Buchheit
*, Cynthia E. Burke, Charles C. Vining, Rushin D. Brahmbhatt, June S. Peng
Penn State College of Medicine, Hershey, PA
INTRODUCTIONThe benefit of chemotherapy in addition to surgery for pancreatic ductal adenocarcinoma (PDAC) is well established. Neoadjuvant chemotherapy (NAC) is beneficial for patients with borderline resectable and locally advanced PDAC in comparison with upfront surgery and adjuvant chemotherapy (AC). However, the role of NAC for resectable PDAC is debated due to conflicting results in randomized trials. The recent NORPACT-1 trial compared neoadjuvant FOLFIRINOX (4 cycles + surgery + 8 cycles) versus adjuvant FOLFIRINOX (surgery + 12 cycles) and reported worse median survival of 25.1 months in the NAC group versus 38.5 months with upfront surgery. The trial also showed the challenge of delivering all intended treatment. Surgery was performed in 81.8% of the NAC arm and 88.9% of the upfront surgery arm, NAC was given in 79.2% of eligible patients, and AC was initiated in 66.2% and 74.6% of the two groups. We sought to evaluate the benefits of NAC in patients with resectable PDAC in a real-world cohort, using an intention-to-treat approach.
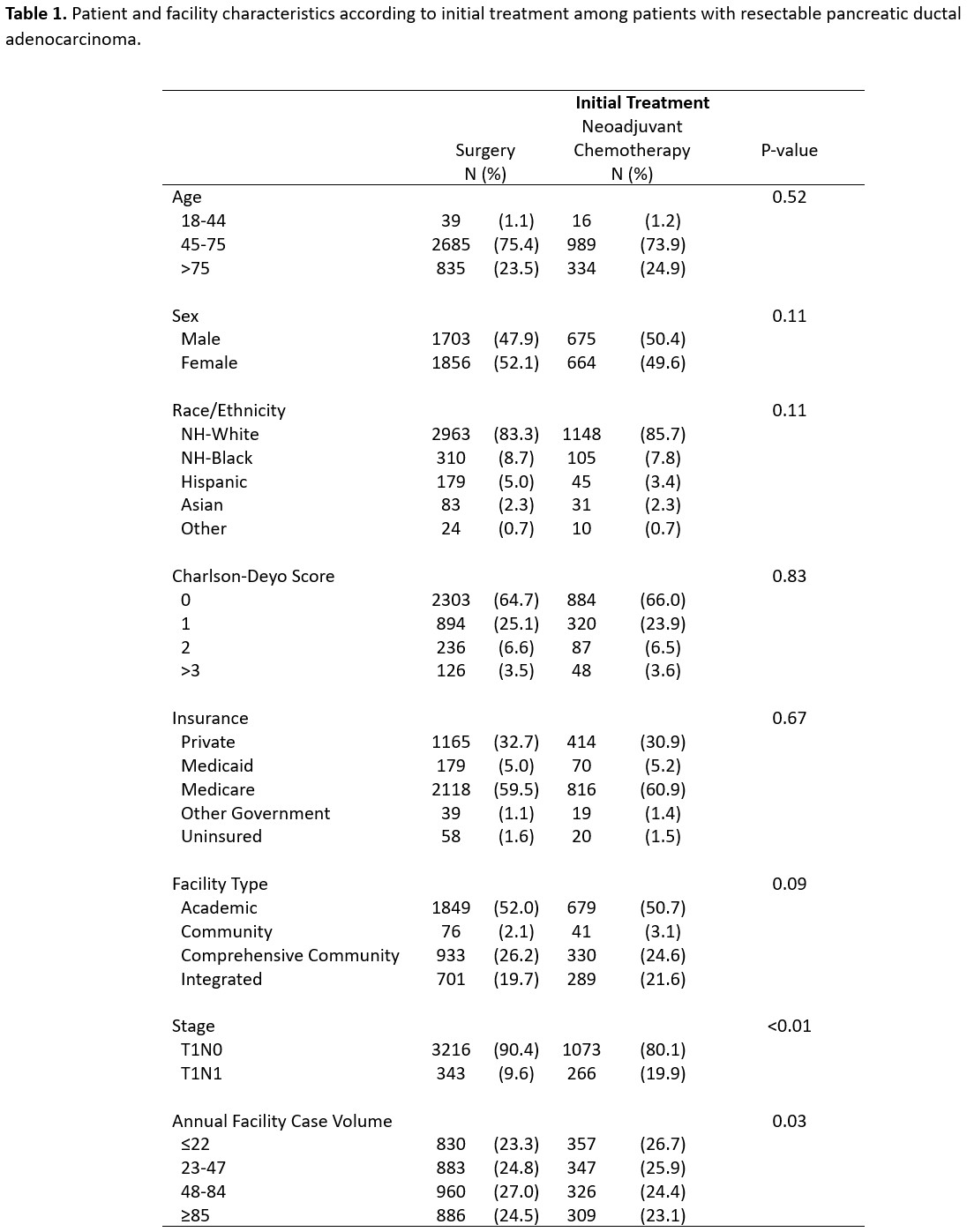
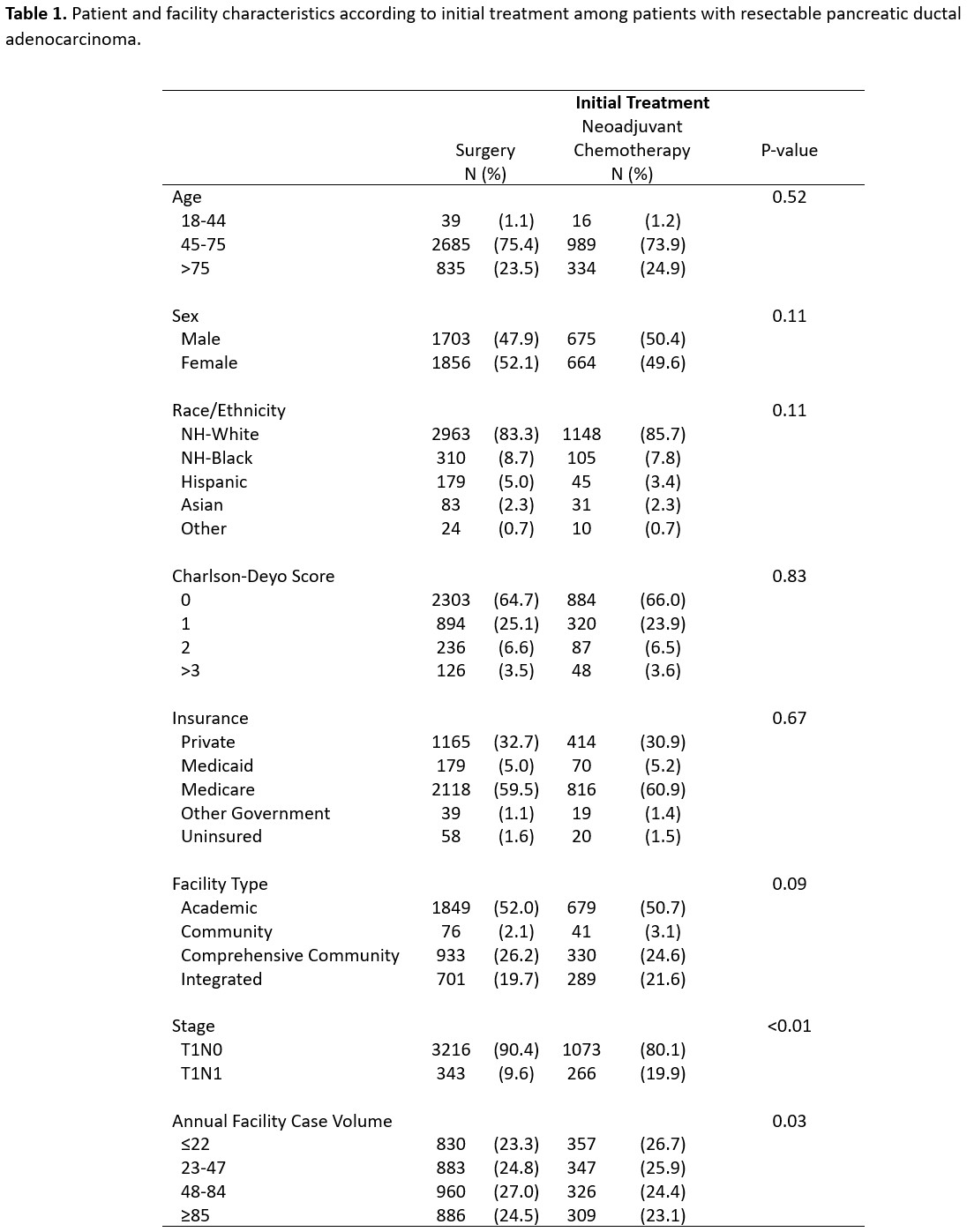
METHODSPatients with clinical T1N0 or T1N1 and M0 PDAC of the head were identified in the 2006-2019 National Cancer Database. Patients coded as receiving palliative-intent treatment were excluded. Patients were categorized into the NAC group if they received NAC prior to surgery or began chemotherapy within 6 weeks of diagnosis but did not undergo resection. Patients were categorized into the upfront surgery group if they had surgery with or without AC. Chi-squared tests compared baseline characteristics, while Kaplan-Meier methods and Cox regression assessed overall survival (OS).
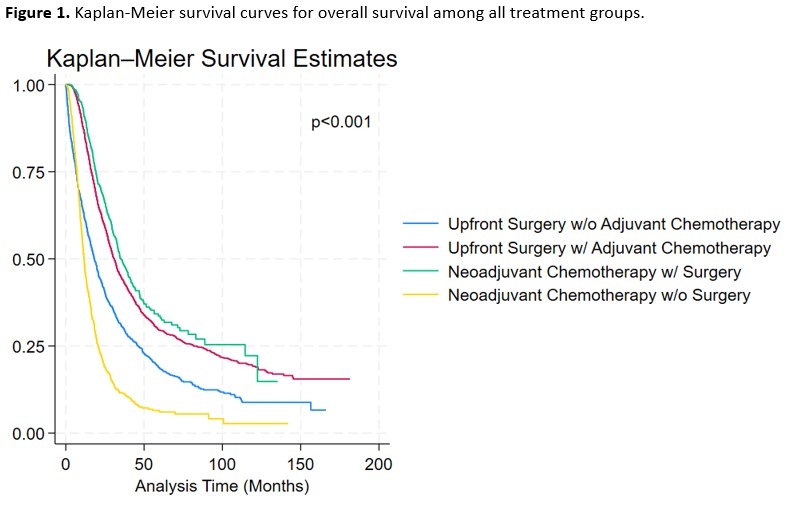
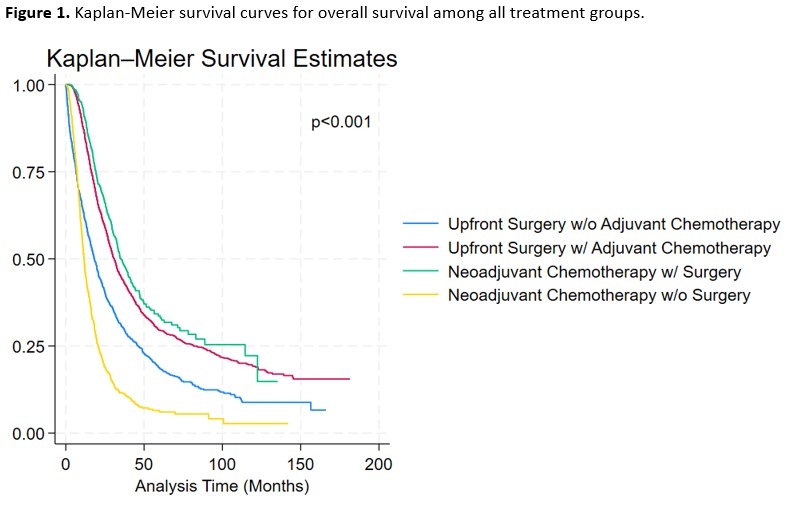
RESULTSOf 4,898 patients, 3,559 (72.7%) received upfront surgery and 1,339 (27.3%) received NAC. In the upfront surgery group, 2,462 (69.2%) received AC. In the NAC group, 721 (53.9%) underwent resection following NAC and 280 (20.9%) received AC. Bivariate analysis by intention-to-treat are shown in Table 1. In the intention-to-treat analysis, median survival for the upfront surgery group was 27.2 months (95%CI 26.1-28.5) versus 20.9 months (95%CI 19.6-23.1) in the NAC group (p<0.01, Figure 1). On multivariable Cox regression, treatment with NAC independently predicted worse OS (HR 1.2; 95%CI 1.1-1.3). However, among patients who received undergo both surgery and systemic therapy, median survival was 30.8 months (95%CI 29.3-32.4) for upfront surgery with AC compared to 35.5 months (95%CI 32.9-39.7) in the NAC plus surgery group (p<0.01).
CONCLUSIONAlthough limited by inferences regarding treatment intent, our analyses by initial therapy showed that upfront surgery was associated with better OS. The decision to proceed with upfront surgery versus NAC for resectable PDAC is complex and should be personalized for each patient. Results from this real-world cohort support upfront surgery, in line with the recently reported randomized trial.
Back to 2024 Abstracts