Back to 2024 Abstracts
DEVELOPMENT OF NONALCOHOLIC FATTY LIVER DISEASE AFTER PANCREATICODUODENECTOMY: A SYSTEMATIC REVIEW AND META-ANALYSIS
Ronnakorn Kongsakon
*, Wasit Wongtrakul, Khemajira Karaketklang, Nonthalee Pausawasdi, Phunchai Charatcharoenwitthaya
Mahidol University Faculty of Medicine Siriraj Hospital, Bangkok, Thailand
Background: Nonalcoholic fatty liver disease (NAFLD) has been observed in patients undergoing pancreaticoduodenectomy, commonly known as the Whipple procedure, for periampullary cancer. However, the prevalence of postoperative NAFLD after pancreaticoduodenectomy has not been systematically assessed.
Methods: We conducted a systematic search of the EMBASE and MEDLINE databases from inception to October 2023 to identify studies investigating the prevalence of postoperative NAFLD after pancreaticoduodenectomy. Random-effects models were utilized to calculate prevalence point estimates with 95% confidence intervals (CI), and meta-regression with subgroup analysis was employed to address heterogeneity.
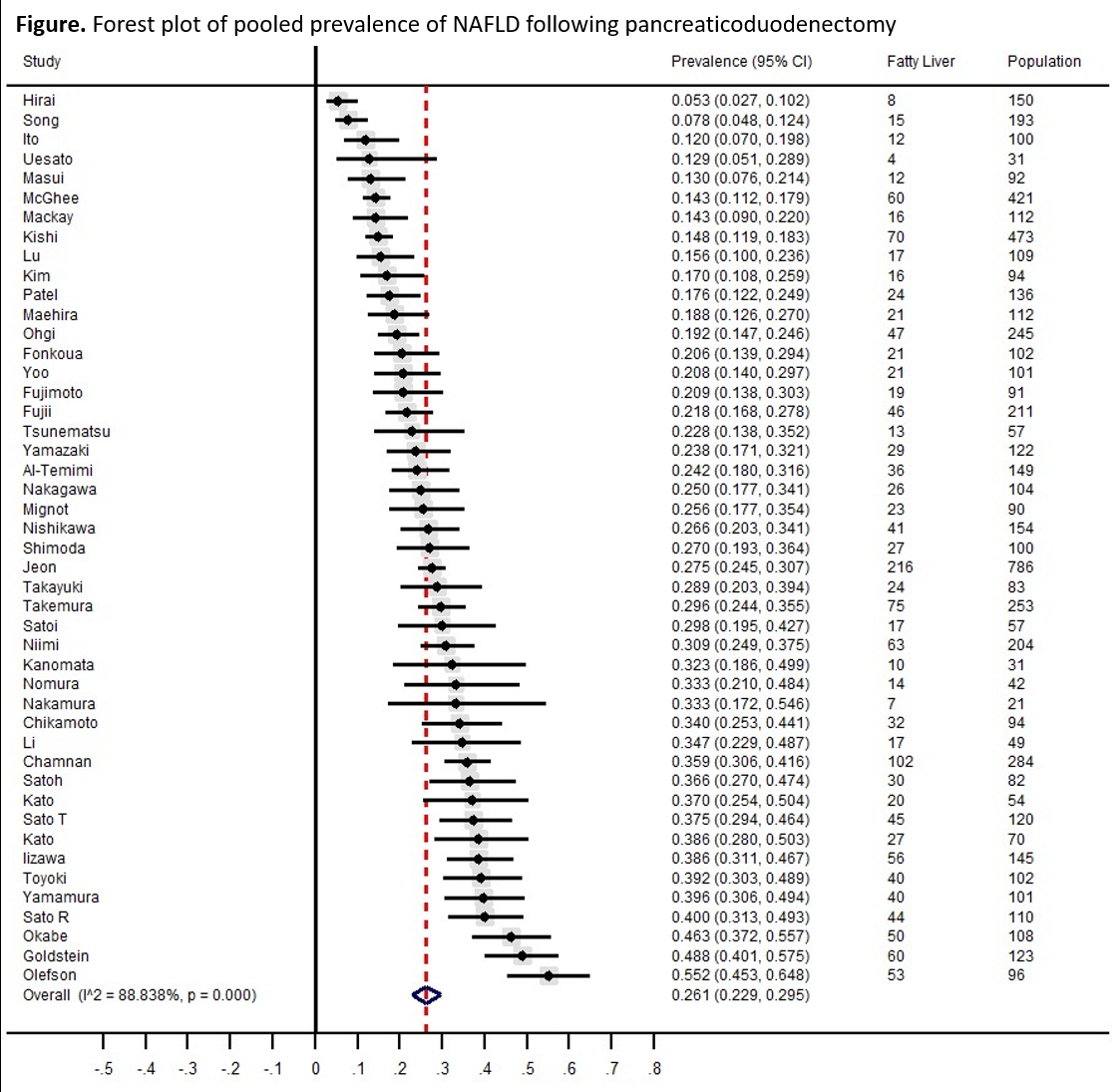
Results: Forty-six studies involving 6,564 patients who underwent pancreaticoduodenectomy (with a mean age of 65 years, 44% female, and a mean body mass index of 23 kg/m2) were included. Among these studies, 32 were full-text articles, and 14 were conference abstracts exploring the prevalence of postoperative NAFLD following pancreaticoduodenectomy. Fatty liver was primarily diagnosed using imaging techniques, predominantly computed tomography. The geographical distribution of these studies was as follows: 31 in Japan, eight in the United States, four in Korea, one in the Netherlands, one in France, and one in Thailand. The pooled prevalence of NAFLD after pancreaticoduodenectomy was 26.1% (95% CI 22.9-29.5;
I2 89%) as shown in Figure. The prevalence was 25.9% (95% CI 17.8-35.1;
I2 92%) in Western countries and 26.2% (95% CI 22.7-29.9;
I2 88%) in Eastern countries. The pooled prevalence from studies published before 2015 (25.4%, 95% CI 18.9-32.6;
I2 88%) was comparable to those published since 2015 (26.4%; 95% CI 22.6-30.4;
I2 89%). Retrospective and prospective studies yielded corresponding pooled prevalence of 25.7% (95% CI 22.4-29.2;
I2 89%) and 31.1% (95% CI 17.9-46.1;
I2 85%), respectively. When each study was removed from the analysis once at a time, the pooled prevalence of NAFLD ranged from 25.6% to 26.7%, indicating that no individual study had a significant effect on the prevalence of NAFLD following pancreaticoduodenectomy. Meta-regression analyses did not identify any significant effects of mean age, the proportion of male patients, and the percentage of pre-existing type 2 diabetes, hypertension, and hyperlipidemia on the prevalence. The funnel plot and Egger's test (p=0.117) revealed no significant publication bias.
Conclusions: This meta-analysis revealed that approximately a quarter of patients undergoing pancreaticoduodenectomy developed postoperative NAFLD. Given the established and concerning health risks associated with NAFLD, it is crucial to acknowledge and comprehensively understand this post-operative consequence. Further studies should focus on the mechanistic aspects of this phenomenon and explore associated contributing factors.
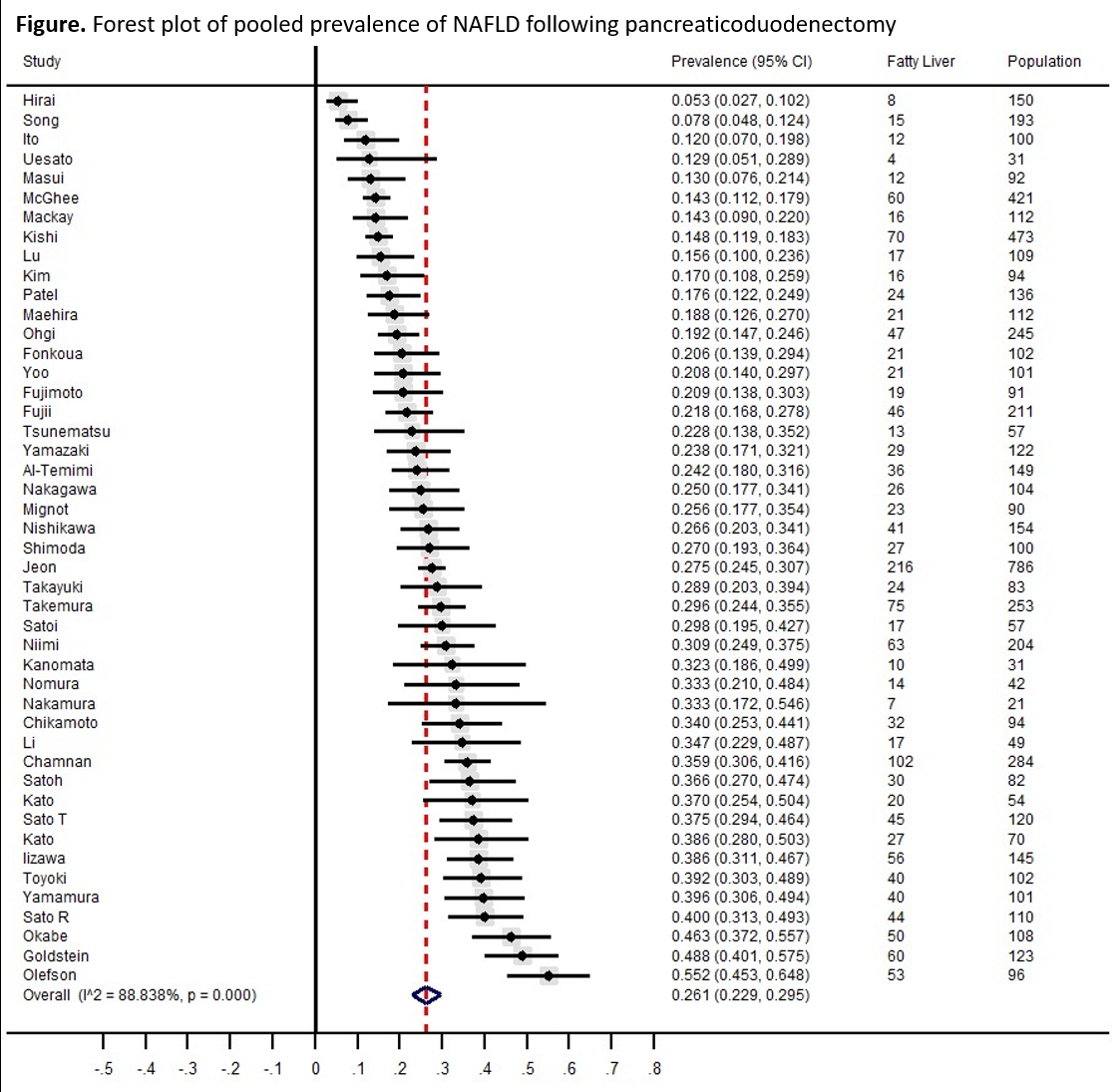 Figure.
Figure. Forest plot of pooled prevalence of NAFLD following pancreaticoduodenectomy
Back to 2024 Abstracts