Back to 2024 Abstracts
ASSESSING THE DIAGNOSTIC CONCORDANCE BETWEEN SURGEONS AND RADIOLOGISTS IN PANCREATIC CYST IMAGING
Gerik Cervantes
*1, juan malo
2, Houssam Osman
2, D Rohan Jeyarajah
21Texas Christian University Anne Burnett Marion School of Medicine, Fort Worth, TX; 2Methodist Richardson Medical Center, Richardson, TX
Background:Pancreatic cysts are often encountered as incidentally. The array of pancreatic cysts includes benign cyst types and those with malignant potential such as mucinous cystic neoplasms (MCNs) and intrapapillary mucinous cystic neoplasms (IPMNs). Granting the capacity to determine malignant potential is crucial. However, specificity for recognition of these cysts is limited and focuses primarily on clinical and morphological parameters for diagnosis. The aim of this study is to evaluate accuracy of hepatopancreaticobiliary (HPB) surgeons and radiologists in identifying these cysts on imaging solely and identify areas of improvement in analysis of pancreatic neoplasms.
Methods:
We analyzed 17 CT and MRI imaging results of patients with pathology proven pancreatic cysts and blindly surveyed 4 HPB surgeons and 4 radiologists for diagnosis. Questionnaires were distributed via online surveying with choice options of IPMN, MCN or Pseudocyst. Option for free writing was available. No clinical background was provided regarding the patient's clinical course or symptomatology. Radiologic interpretation of these images were compared to final pathology results and analyzed.
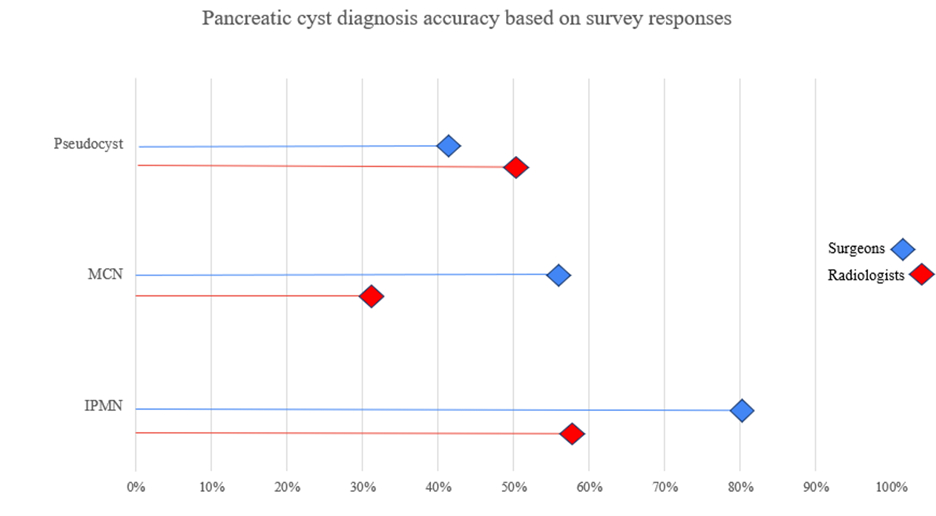
Results:A total of 17 radiologic images were compared to final pathology. Nine (52.94%) were MRI and eight (47.06%) were CT. 10 images (58.82%) were IPMN, 4 images (23.52%) were MCN, and 3 images (17.65%) were pseudocysts. 4 HPB surgeons completely agreed on 7 (41.17%) images however, there was no complete agreements in radiologists. Responses were considered as a partial agreement, defined as at least 50% correct responses in four (23.53%) cases with HPB surgeons and 12 (70.59%) within radiologists. Only one (5.88%) of these cases had no consensus with complete disagreement in HPB surgeons, meaning all reported different diagnoses, however in radiologists there was no complete disagreement. IPMN cases yielded 32 correct responses (80%) among the HPB surgeons. This was the most accurately diagnosed pancreatic cyst in HPB surgeons. Pseudocysts responses with HPB surgeons were 5 (41%) correct responses, however 6 (50%) correct responses in radiologists, with pseudocysts being the most correctly identified in radiologists. Pseudocyst was the only cyst that did not have complete agreement in surgeons. There was only one case in surgeons where complete agreement on diagnosis was wrong, noting all 4 surgeons called an MCN a pseudocyst. A similar result was noted in radiologists where IPMN was reported as a pseudocyst by all 4 radiologists incorrectly.
Conclusions:In evaluation of pancreatic cysts, it is important for hepatobiliary surgeons and radiologists to identify those that have a higher potential for malignant transformation. We demonstrate in our study that HPB surgeons demonstrate higher accuracy in identifying such lesions, emphasizing the importance of a precise clinical diagnosis.
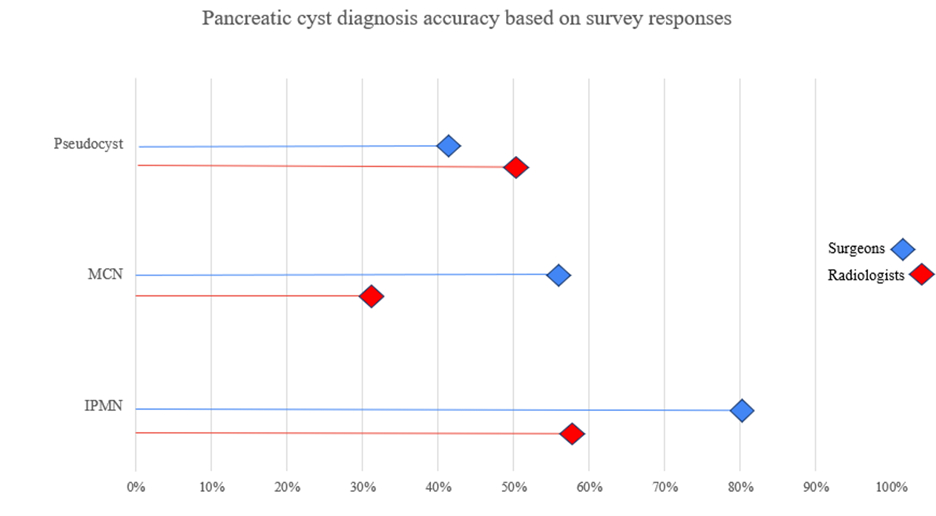 Figure 1. Observed accuracy of diagnosis based on pancreatic cyst type in surgeons and radiologists. Credit: Gerik Cervantes
Figure 1. Observed accuracy of diagnosis based on pancreatic cyst type in surgeons and radiologists. Credit: Gerik Cervantes
Back to 2024 Abstracts