Back to 2024 Abstracts
TOTAL NEOADJUVANT THERAPY IN DISTAL PANCREATIC ADENOCARCINOMA: DOES LOCATION IMPACT THERAPY RESPONSE?
Andrew B. Crocker
*1, Maryclare E. Taylor
1, Emily Papai
1, Max Perilstein
2, Malek Maddah
2, Karen Ruth
1, Anthony Villano
1, Sanjay S. Reddy
11Surgical Oncology, Fox Chase Cancer Center, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: The role of total neoadjuvant therapy (TNT) in pancreatic ductal adenocarcinoma (PDAC) remains controversial with mixed data in the literature. Due to its relative rarity, adenocarcinoma of the distal pancreas is largely understudied, and the impact of TNT for these pancreatic malignancies remains unclear. Therefore, in the analysis we aim to investigate how TNT impacts survival and pathologic response in this patient population.
Methods: A single-institution retrospective review of patients with pathologically confirmed PDAC who underwent distal pancreatectomy between 2008 and 2022 was performed. TNT was defined as receipt of both neoadjuvant chemotherapy and chemoradiation, while single modality neoadjuvant therapy (SMNT) included patients who received only neoadjuvant chemotherapy or chemoradiation. Surgery first (SF) patients did not receive neoadjuvant therapy. Patient characteristics and outcomes were compared using Kruskal-Wallis and Fisher's exact tests. Survival estimates were determined using Kaplan-Meier methodology and compared with log rank tests.
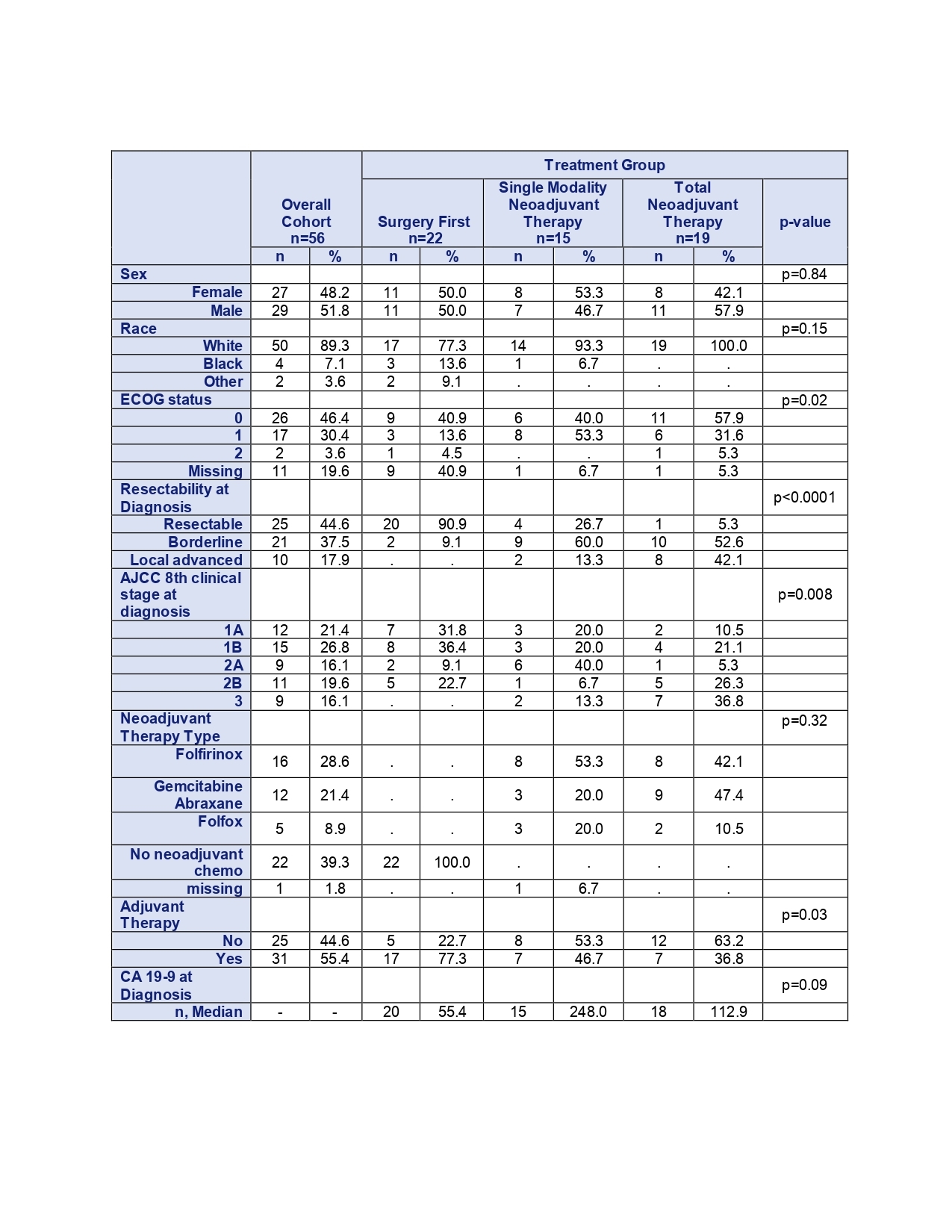
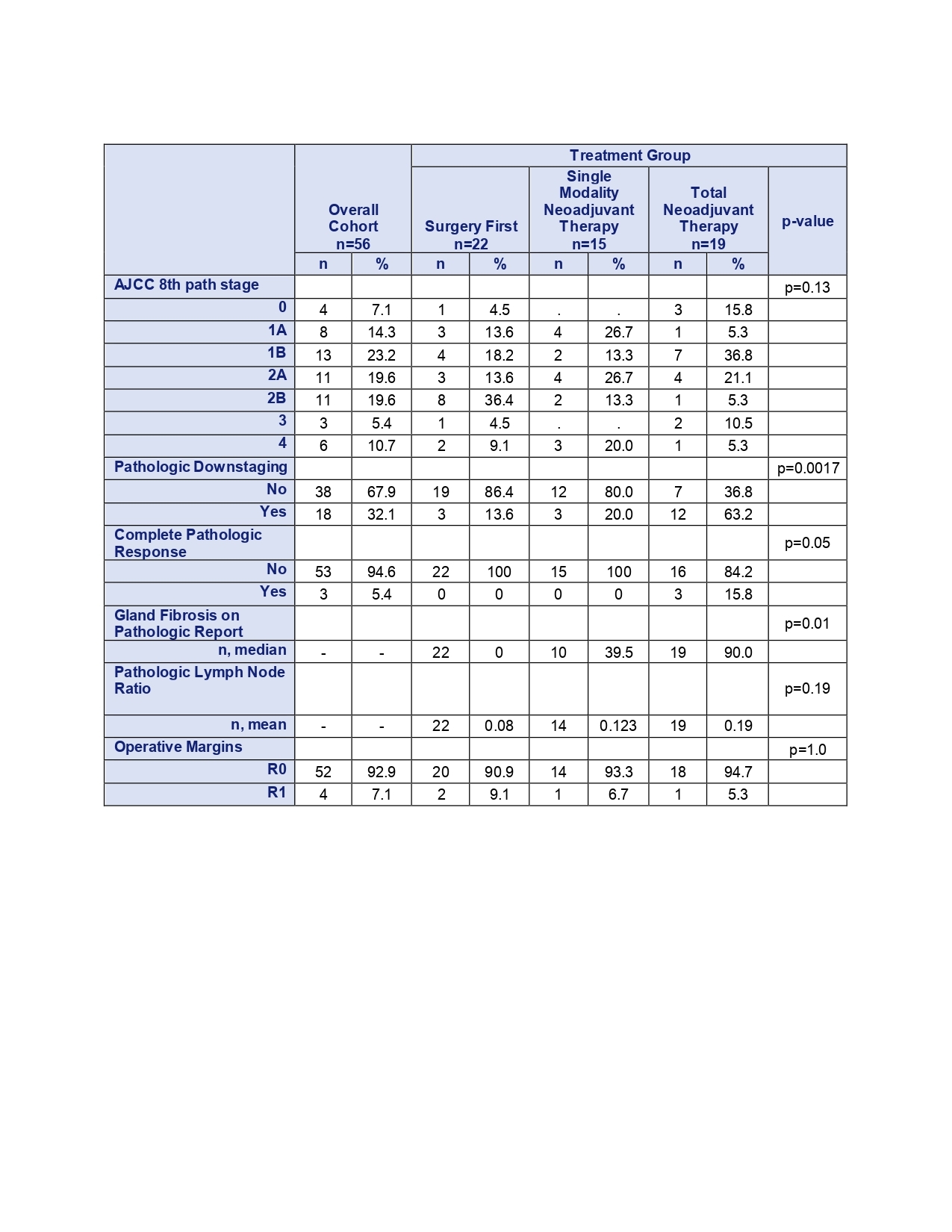
Results: As shown in Table 1, 56 patients met inclusion criteria, with 19 patients undergoing TNT (33.9%), 15 patients receiving SMNT (26.8%), and 22 patients in the SF group (39.3%). Overall median age at diagnosis was 66.5 years and did not differ by treatment group (p=0.12). Patients in the SF group were significantly more likely to be resectable, compared to higher rates of borderline and locally advanced disease in the SMNT and TNT groups (p<0.0001). SMNT patients demonstrated the highest median CA 19-9 at diagnosis (248.0), followed by TNT (112.9) and SF patients (55.4) (p=0.09). The SF cohort was more likely to receive adjuvant therapy (77.3%) compared to both the SMNT (46.7%) and TNT (36.8%) groups (p=0.03). Fibrosis on pathologic analysis was reported in 91.1% of patients, with the TNT group having the highest median fibrosis (90.0%) compared to the SMNT (39.5%), and SF groups (0%) (p=0.01, Table 2). There was no significant difference in positive lymph node ratio across treatment groups (p=0.19). Patients in the TNT group were more likely to demonstrate pathologic downstaging (63.2%), relative to SMNT (20.0%) and SF (13.6%) (p=0.0017). TNT patients were also the most likely to have complete pathologic response (15.8%), though this was the only patient group with any complete responders (p=0.05). Notably, there were no significant differences in overall survival (p=0.90) or disease-free survival (p=0.51) among treatment groups.
Conclusions: TNT in distal PDAC was associated with improved pathologic downstaging, but no differences in overall or disease-free survival. Given the limitations of sample size in the context of distal disease incidence, additional studies are warranted to further understand the potential efficacy of TNT in distal PDAC.
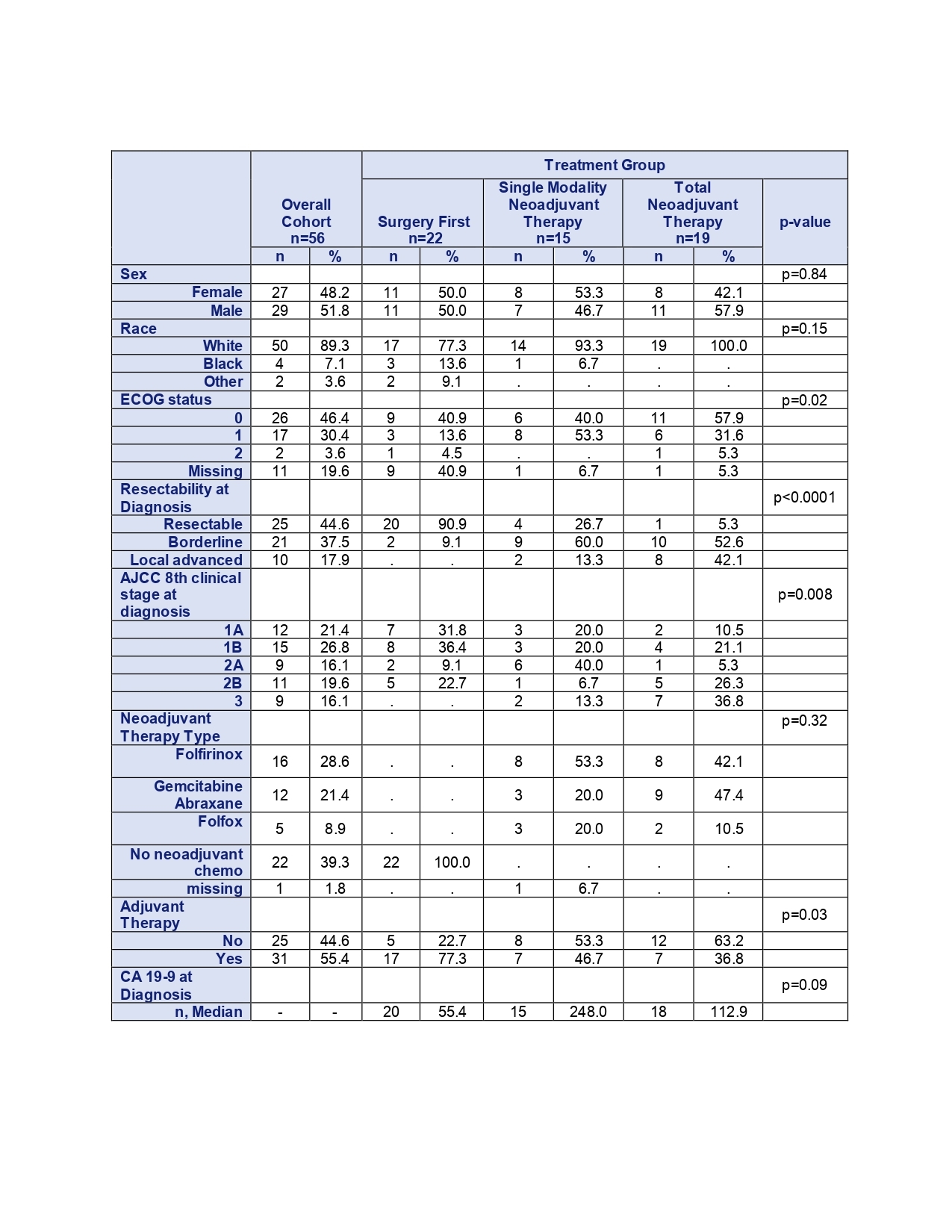 Table 1: Demographic and Clinicopathologic Characteristics by Therapy Type
Table 1: Demographic and Clinicopathologic Characteristics by Therapy Type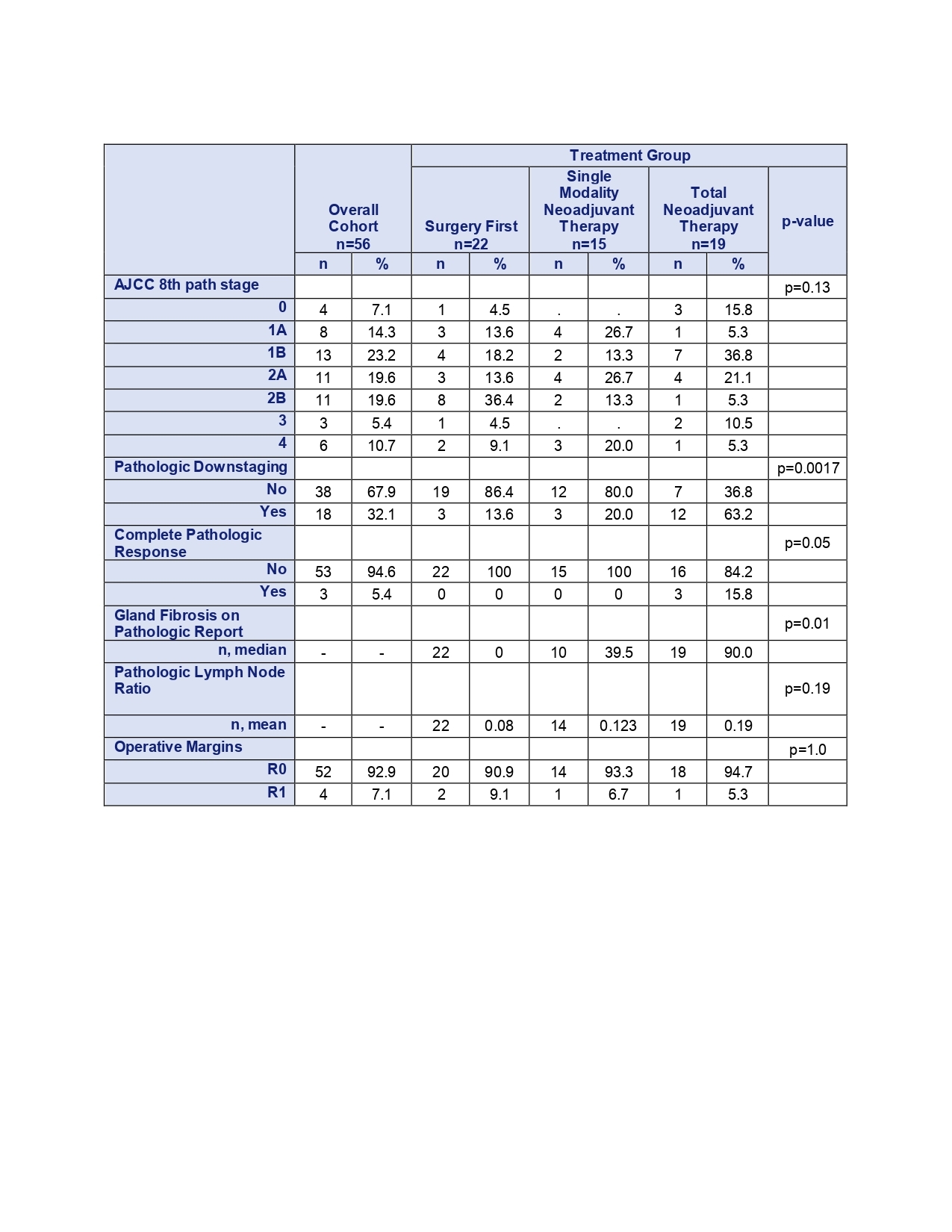 Table 2: Pathologic Factors after Resection by Treatment Group
Table 2: Pathologic Factors after Resection by Treatment Group
Back to 2024 Abstracts