Back to 2024 Abstracts
READMISSION AFTER DISTAL PANCREATECTOMY FOR CHRONIC PANCREATITIS: COMMON AND CONSEQUENTIAL
Katelyn Flick
*, Kyle A. Lewellen, James Butler, Eugene P. Ceppa, Ryan J. Ellis, Michael G. House, Trang Nguyen, Alexandra M. Roch, C. Max Schmidt, Nicholas J. Zyromski, Thomas K. Maatman
Indiana University School of Medicine, Indianapolis, IN
Introduction:
Patients with chronic pancreatitis (CP) predominantly involving the pancreatic body/tail benefit from distal pancreatectomy (DP), with most experiencing long-term improvements in symptoms after recovery from surgery. Chronic inflammatory changes in the left upper quadrant can make for a technically demanding operation and disease-specific comorbidities impact postoperative recovery. The aim of this study was to evaluate the incidence, etiology, and risk factors for hospital readmission after DP for CP.
Methods:
An institutional prospectively maintained database was retrospectively reviewed to identify patients who underwent DP for CP between 2007 and 2022. Ninety-day hospital readmission rates and etiologies of readmission were evaluated. Etiologies of readmission were grouped into themes – multiple were possible for each individual patient. Postoperative complication definitions aligned with the International Study Group in Pancreatic Surgery (ISGPS) and National Surgical Quality Improvement Program (NSQIP). Total postoperative hospital days was defined as postoperative length of stay plus inpatient length of stay for readmission(s). Descriptive statistics and univariable analysis were utilized.
P values <0.05 were accepted as statistically significant.
Results:
During the study period, 186 patients underwent DP for CP. Mean age was 50.1±12.6 years and 59% were male. Common preoperative comorbidities included: hypertension (51%), tobacco use (41%), and diabetes mellitus (36%). Most (92%) patients were ASA class three or higher. Open surgical technique was utilized in 74% of cases and mean postoperative length of stay was 8.3±6.8 days. Mortality rates at 30-days and 90-days were 0% and 0.5%, respectively. The incidence of hospital readmission was 12% and the median number of readmissions was 1 (range, 1-4). Preoperative endoscopic pancreatic duct (PD) therapy was the only preoperative factor associated with readmission on univariate analysis (No PD therapy, 6.7%; PD therapy, 17.5%;
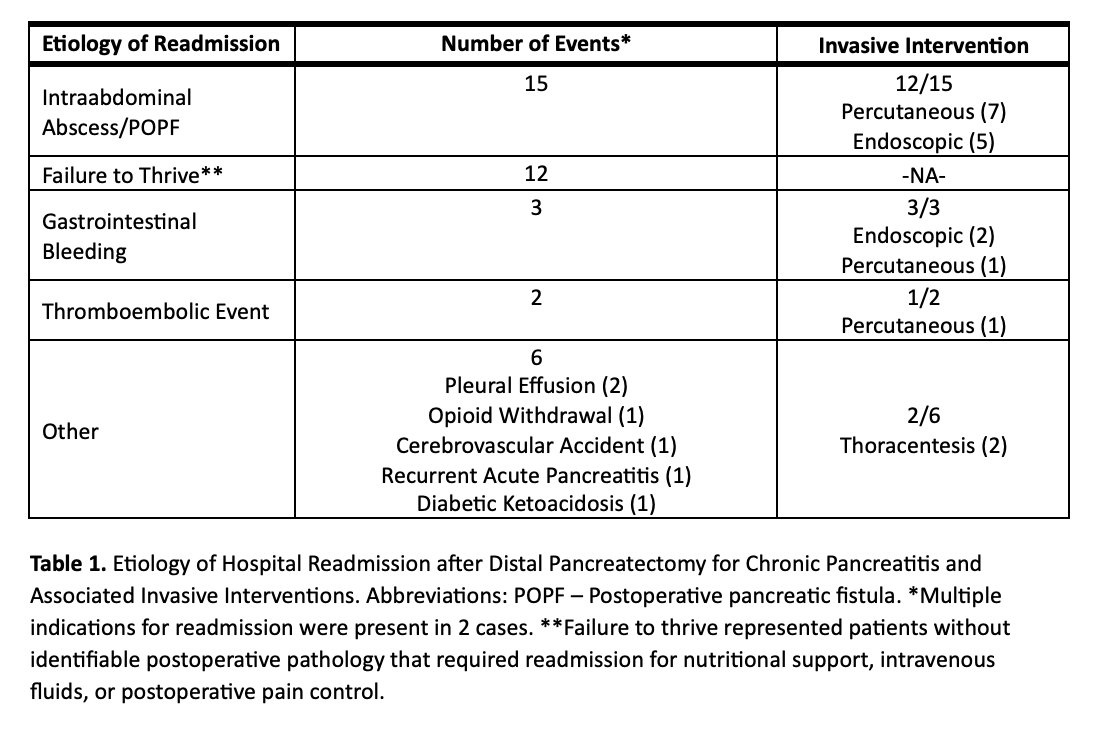
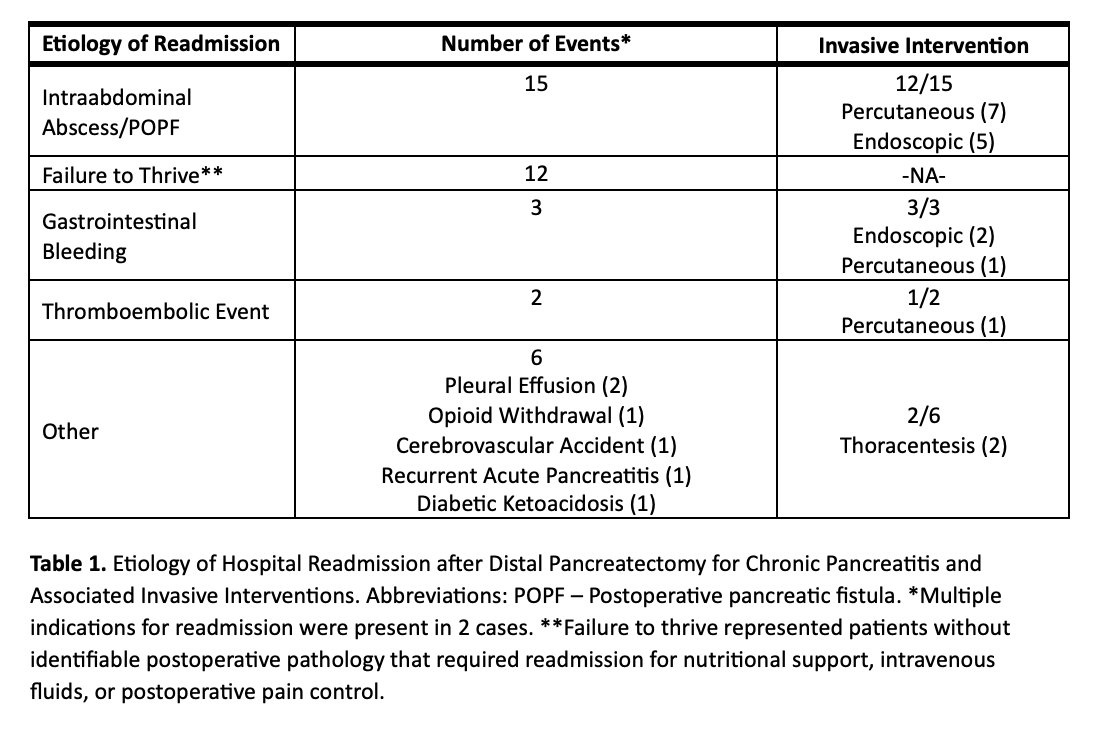
P = 0.026). Readmission etiologies are outlined in Table 1. Of the 23 patients that were readmitted, a total of 38 etiologies for readmission were identified and 18 invasive interventions were performed in treatment. Failure to thrive without identifiable pathology resulted in hospital readmission in 32% of cases. Among patients that required readmission, the mean number of total postoperative hospital days was 16.6±9.8 days.
Conclusion:
Readmission after distal pancreatectomy for chronic pancreatitis was observed in 12% of patients and frequently represented a major postoperative morbidity that required an invasive intervention. One-third of hospital readmissions were attributable to failure to thrive and may be preventable.
Back to 2024 Abstracts