Back to 2024 Abstracts
POST-ESOPHAGECTOMY HIATAL HERNIA FOLLOWING MINIMALLY INVASIVE ESOPHAGECTOMY IN ESOPHAGEAL CANCER PATIENTS
Thitiporn Chobarporn
*1,2, Stephanie G. Wood
21Chulalongkorn University, Bangkok, Bangkok, Thailand; 2Oregon Health & Science University, Portland, OR
Introduction: Minimally invasive esophagectomy (MIE) has emerged as the primary surgical approach for esophageal cancer, aiming to reduce morbidities from open esophagectomy. The enhanced survival resulting from multimodal treatment has brought to light post-esophagectomy hiatal hernia (PEHH), a previously uncommon long-term complication in the era of open esophagectomy. The aim of this study is to examine the risk factors and incidence of post-esophagectomy hiatal hernia after MIE in esophageal adenocarcinoma patients.
Methods: A retrospective review of the clinical follow-up data of esophageal cancer patients who underwent MIE at our institution from January 2013 to August 2023 was performed. All patients with symptomatic or incidentally found PEHH were identified by reviewing computed tomography scans for cancer surveillance. Patients who had PEHH were compared with those who did not have PEHH. The univariate analysis was performed by using the Chi-Square test for categorical variables and the t-test for continuous variables. Variables with a p-value less than 0.2 on univariate analysis were further analyzed in a multivariate logistic regression model.
Results: In total, 373 esophageal cancer patients who underwent MIE were included. The mean age was 65.9 ± 9.1 years, and 85% were male. Most patients were staged with locally advanced disease, and 90.6% received neoadjuvant chemoradiotherapy. The incidence of post-esophagectomy hiatal hernia was 25 out of 373 patients (6.7%), with 21 (84%) requiring surgical repair. Only 9 patients (36%) were asymptomatic. Emergency operations accounted for 12 (57.1%) of the operations. The most common herniated organ was the colon (68%). The laparoscopic approach was successfully performed in 11 patients (52.4%). Primary crural repair could be successfully performed in 14 cases (66.7%). The diagnosis was made at a median time of 24 months after MIE. There were a significantly lower BMI, a shorter ICU, and shorter hospital stays in the PEHH group. Higher BMI (more than 25 kg/m2) and longer ICU stays were independently associated with a reduction in the likelihood ratio of developing PEHH.
Conclusion: The incidence of PEHH following MIE should not be understated, as it has the potential to cause severe complications, even over a long period of time. The majority of PEHH cases were effectively treated through a minimally invasive method involving primary crural repair.
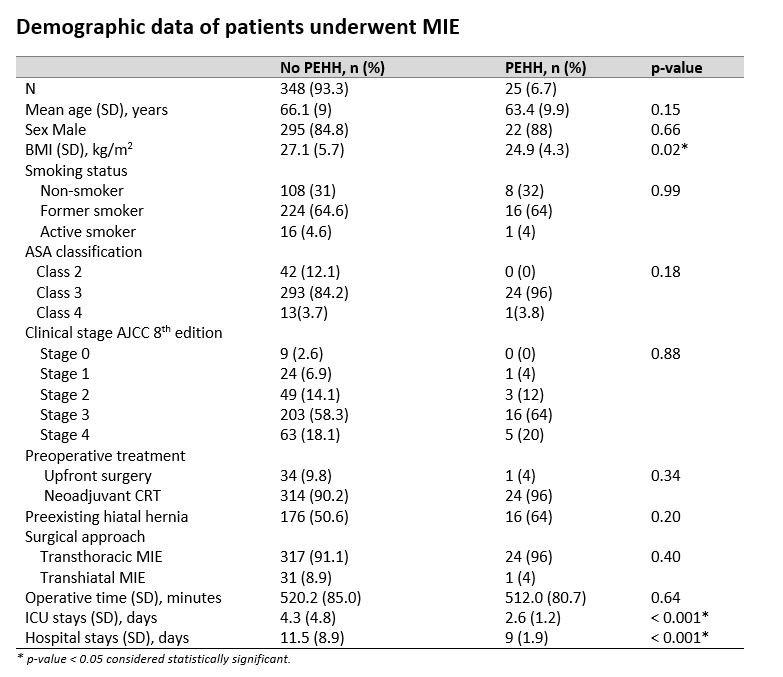 Table 1 Demographic data of patients underwent MIE
Table 1 Demographic data of patients underwent MIE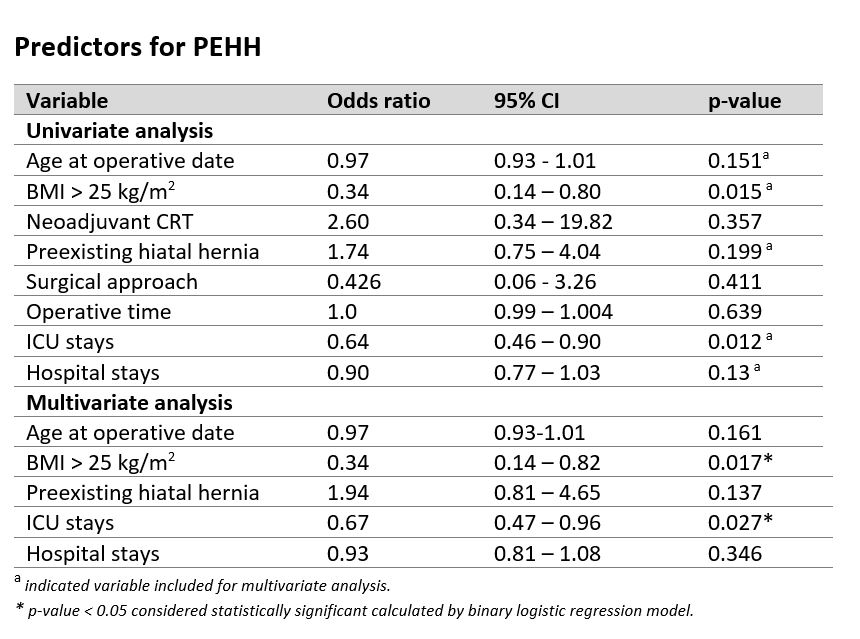 Table 2 Predictors for PEHH
Table 2 Predictors for PEHH
Back to 2024 Abstracts