Back to 2024 Abstracts
CHYLE LEAK FOLLOWING PANCREATIC RESECTION: AN UNDERAPPRECIATED CAUSE OF DELAYED POSTOPERATIVE RECOVERY
Grace C. Bloomfield
*1, Jean Namgoong
1, Piyush Gupta
2, Aradhya Nigam
2, Thomas Fishbein
2, Pejman Radkani
2, Emily R. Winslow
21Medical Student, Georgetown University School of Medicine, Washington, ; 2Georgetown University Medical Center, Washington,
IntroductionChyle leaks are not uncommon following pancreatic resection surgery but are often regarded as clinically insignificant relative to other complications. Our aim was to investigate the recovery of patients who develop post-pancreatectomy chyle leaks and compare the incidence of associated morbidity with pancreatic leaks.
MethodsPatients who developed chyle leak and pancreatic leak (POPF) were identified from an existing institutional database of consecutive pancreatic resection cases between 2017-2022. Preoperative characteristics, operative notes, and outcomes occurring within 90 days postoperatively were reviewed retrospectively. Postoperative data were collected on nutrition, drain management, and health care utilization including length of stay (LOS) and readmission, and compared between groups with a significance level set to p<0.05.
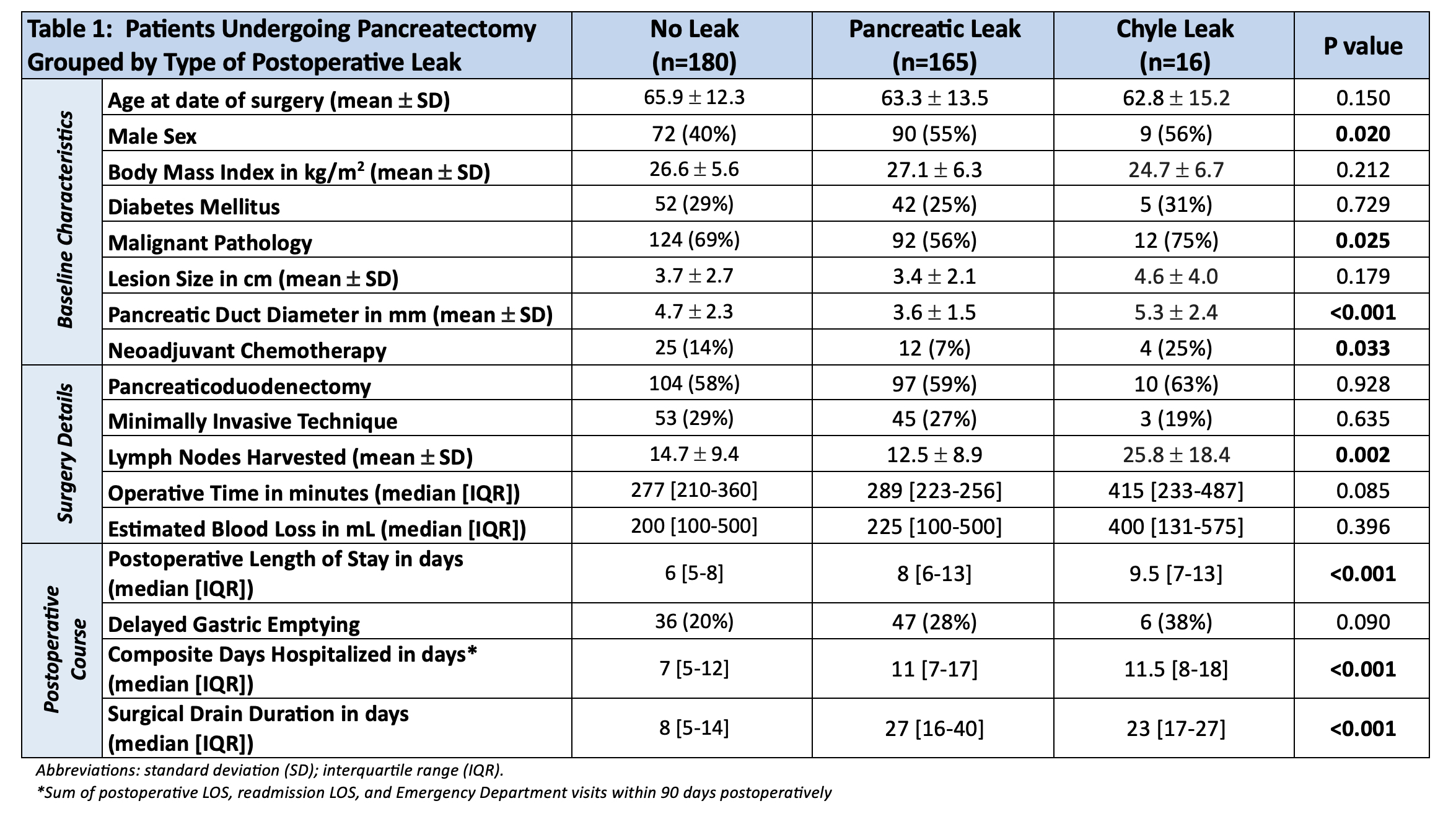
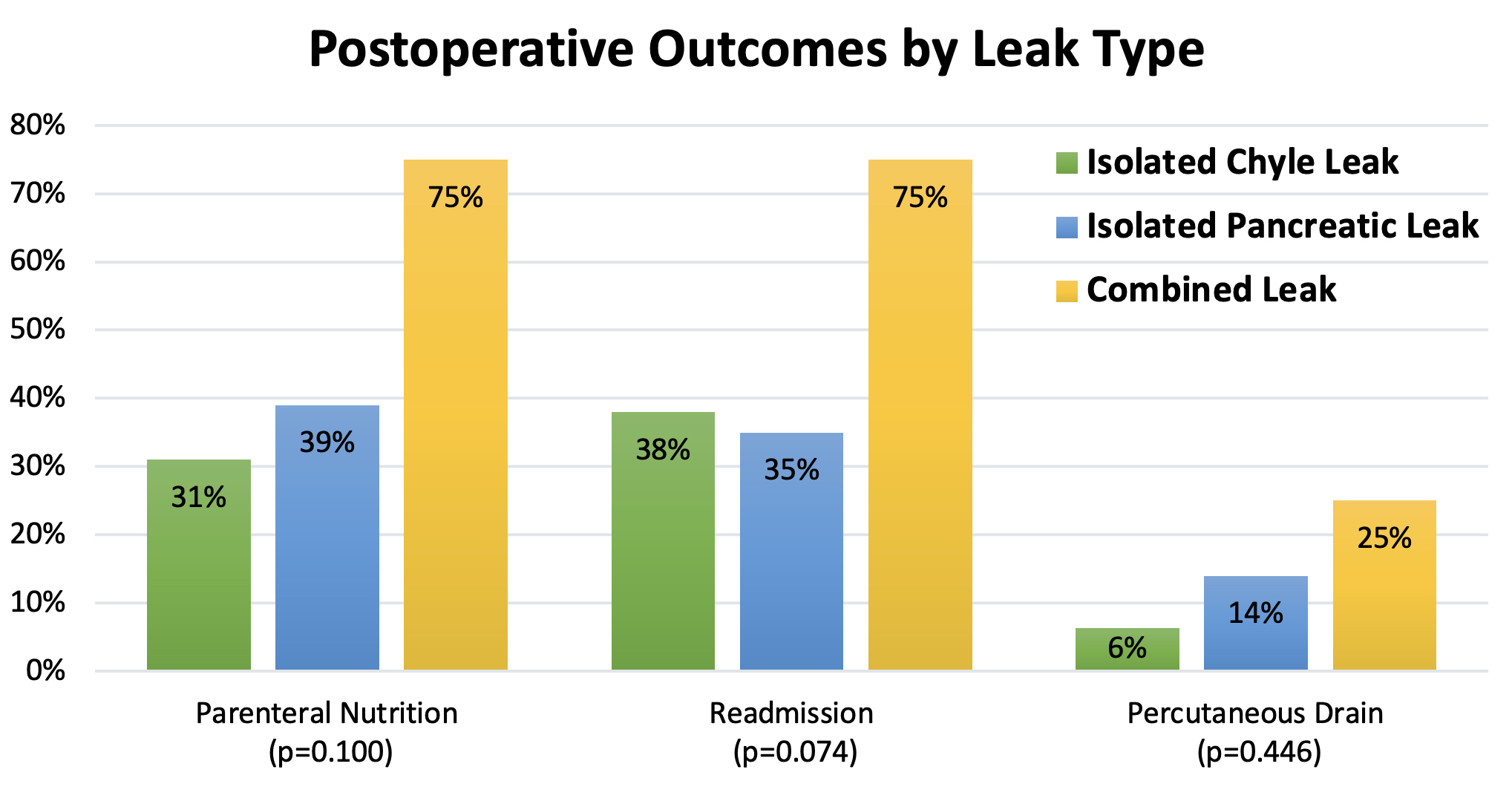
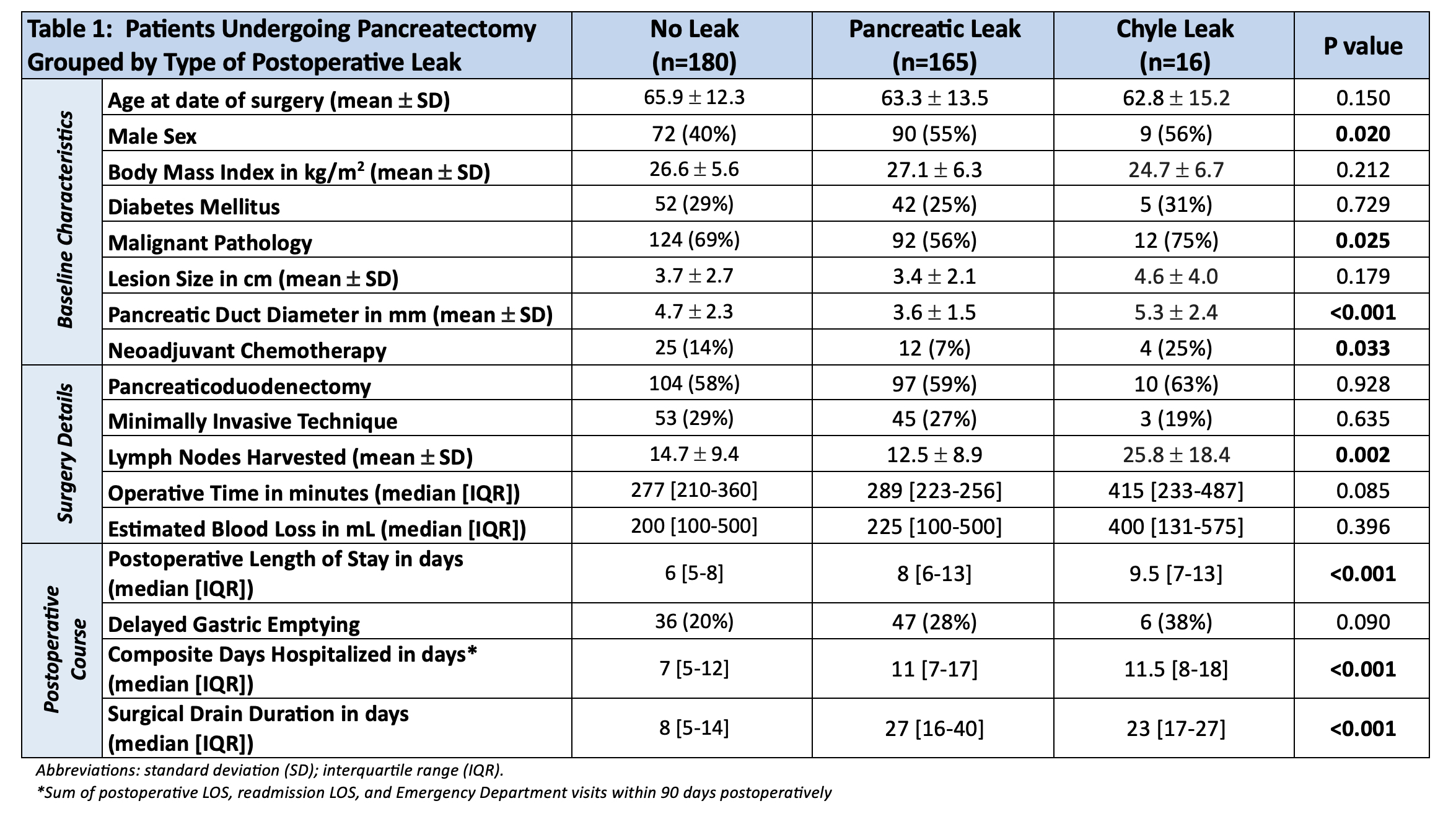
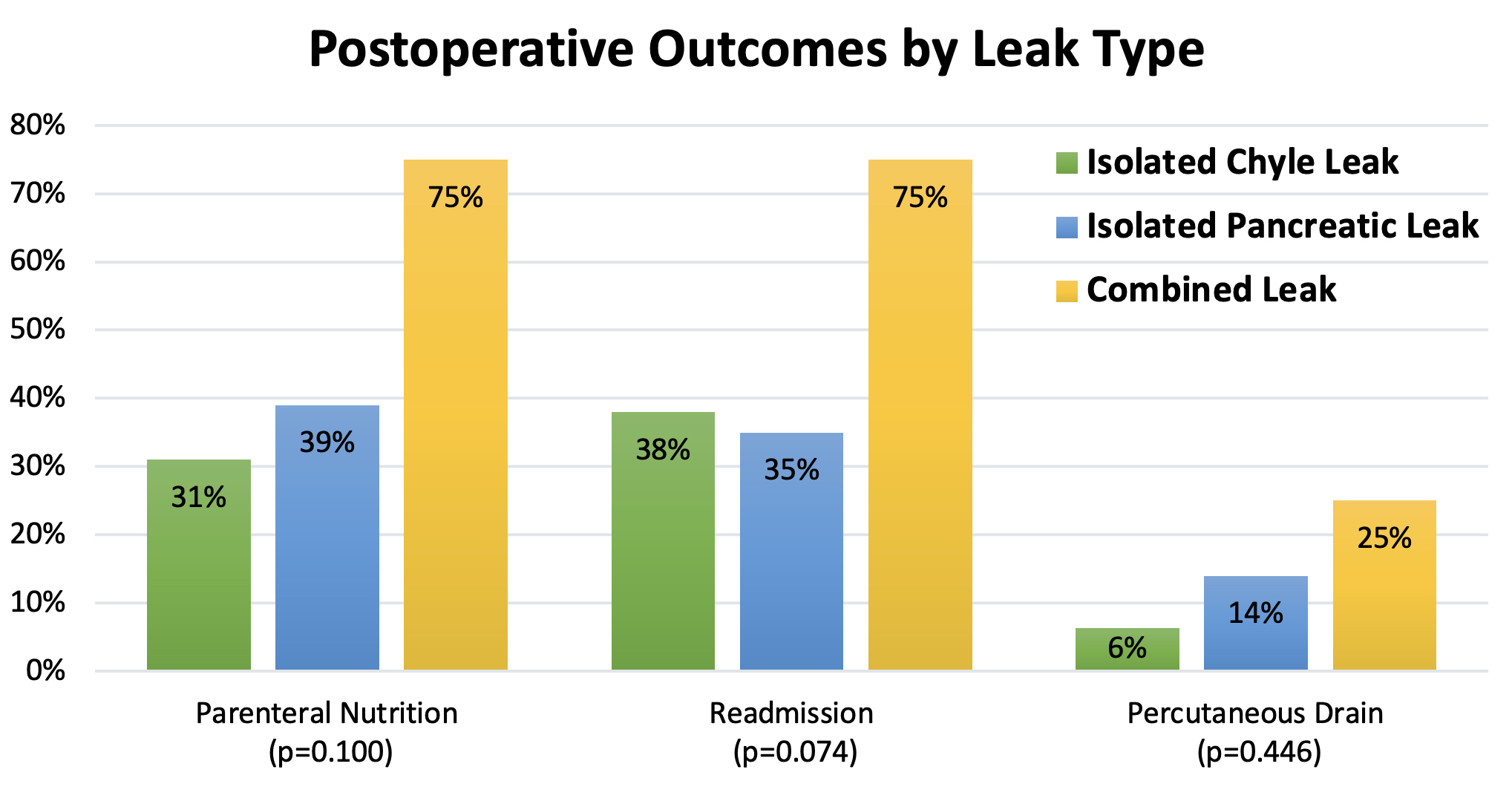
ResultsOf 369 pancreatectomy cases, we identified 24 patients (6.5%) with chyle leak: 16 (4.3%) with isolated chyle leak and 8 (2.2%) meeting criteria for both pancreatic and chyle leaks (combined leak group). The median postoperative day of isolated chyle leak recognition was day seven with a median surgical drain triglyceride level of 619 mg/dL. Parenteral nutrition was utilized in 31% for a median of 35 days while a low-fat diet was utilized in 44%. Relative to the 165 patients with pancreatic leak, the isolated chyle leak group had larger pancreatic duct diameters (p=0.001), higher rates of neoadjuvant chemotherapy (p=0.039), and more lymph nodes harvested during pancreatectomy (p=0.002). As expected and seen in Table 1, patients without any leak had more favorable postoperative courses with shorter LOS and time to drain removal. However, comparing patients with chyle leaks to those with pancreatic leaks, there were no significant differences with regards to days hospitalized or surgically-placed drain duration, or in the rates of parenteral nutrition, readmission, percutaneous drainage, reoperation, or mortality. Interestingly, the combined leak group had more healthcare utilization than those with isolated leaks, with a median surgical LOS of 13 days and hospitalization period of 22 days within 90 days after pancreatectomy. Further, 75% of this group were readmitted and the same percentage received parenteral nutrition. In addition, the combined leak group required a median surgical drain duration of 33 days and percutaneous drains for postsurgical fluid collections were placed in 25% of these patients.
ConclusionOur data suggest that post-pancreatectomy chyle leaks can have as significant an impact on the course of postoperative recovery as pancreatic leaks. When the two leaks occur together, they impose further burden on the patient and require increased healthcare utilization. Additional study of this subgroup would be useful to help further improve outcomes of patients undergoing pancreatectomy.
Back to 2024 Abstracts