Back to 2024 Abstracts
STRATIFICATION OF MANAGEMENT OF POSTOPERATIVE FLUID COLLECTIONS BY POST-RECONSTRUCTION ANATOMIC ZONES IN PANCREATICODUODENECTOMY PATIENTS
Jean Namgoong
*1, Grace C. Bloomfield
1, Piyush Gupta
2, Aradhya Nigam
2, Vasalya Panchumarthi
1, Thomas Fishbein
2, Pejman Radkani
2, Emily R. Winslow
31Georgetown University School of Medicine, Washington, ; 2MedStar Georgetown University Hospital, Washington, ; 3University of Wisconsin-Madison, Madison, WI
IntroductionIntraabdominal fluid collections (FC) are the most common radiological abnormality in patients imaged after pancreaticoduodenectomy (PD). However, there is a paucity of data on predicting if a FC is likely to be clinically problematic. The aim of the present study is to determine the relationship between the specific anatomic location of the FC and the management strategy selected.
MethodsA single-institution retrospective study of patients who underwent PD from 2016 to 2023 was performed. Patients who had CT imaging in the early postoperative period, defined as within eight weeks of PD, were reviewed for development and progress of a FC, defined as any loculated fluid in the operative field measuring ≥1cm. FC locations were categorized in three zones relative to the pancreaticojejunostomy (PJ)- FCs contiguous with the PJ (Zone 1), near the PJ in resection bed (Zone 2), and more distant in abdominal cavity (Zone 3). We defined management strategies in three groups- expectant (clinical observation), non-invasive (antibiotics, parenteral nutrition, or endoscopic procedures), and invasive management (reoperation or percutaneous drainage).
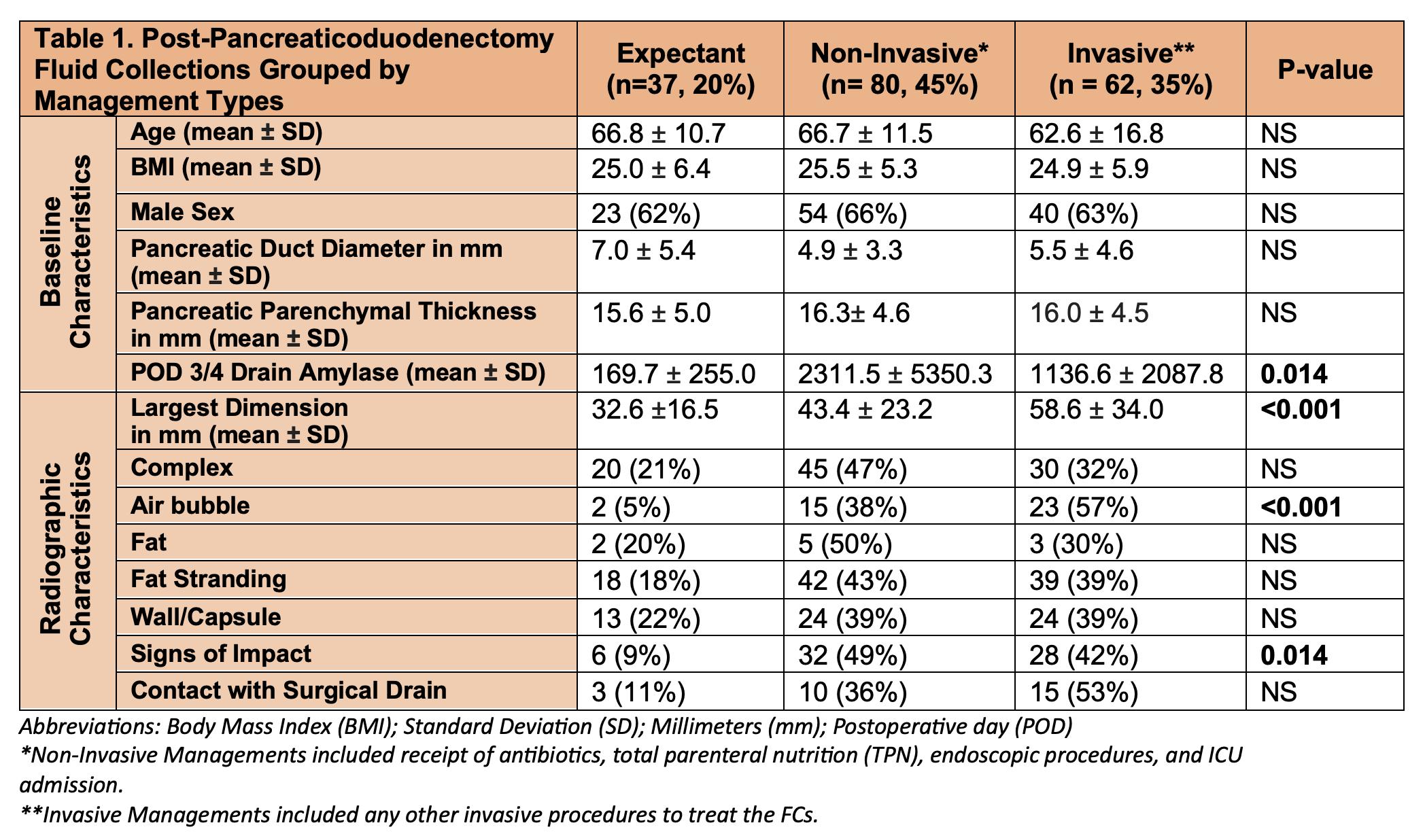
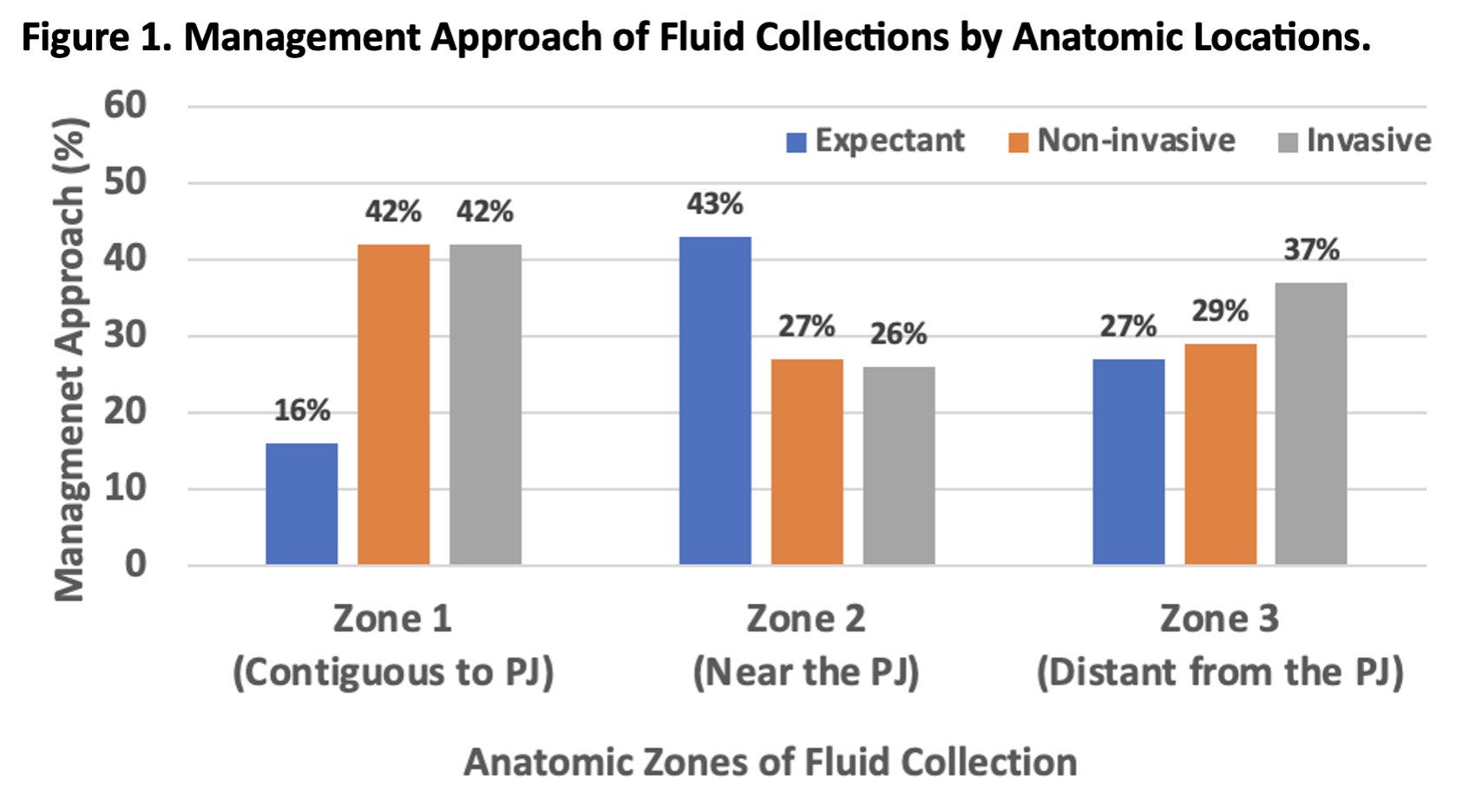
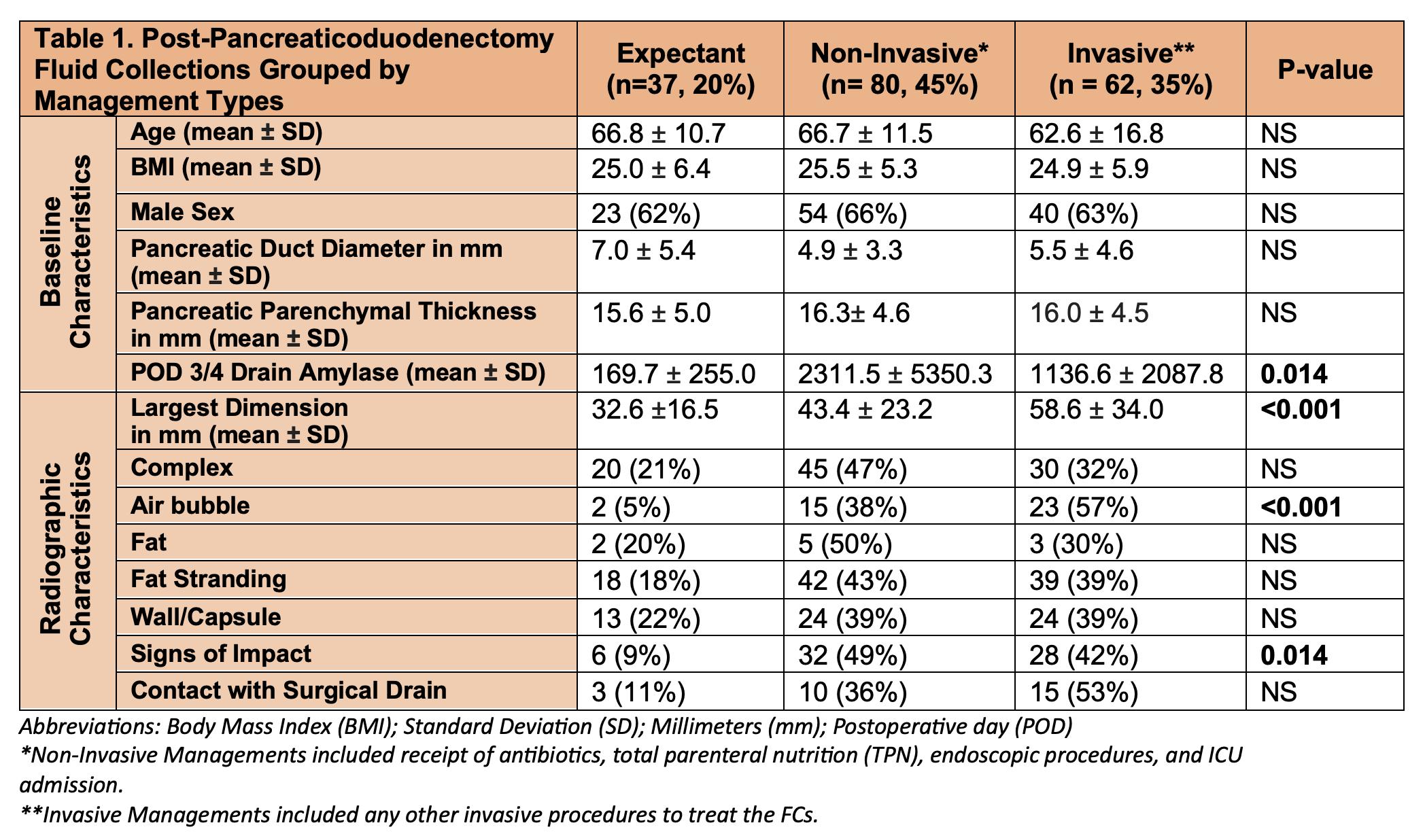
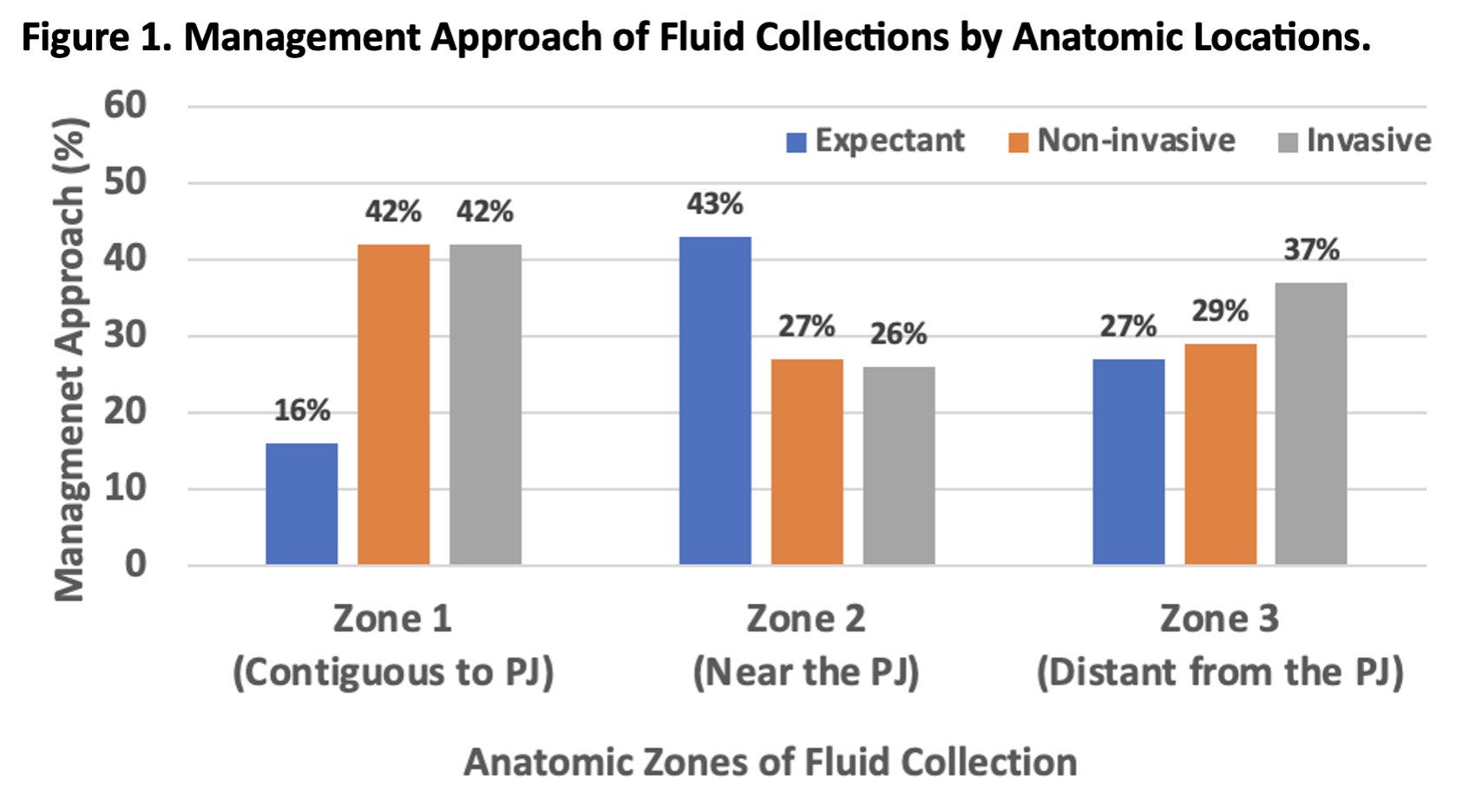
ResultsOf 304 patients, 210 (69%) had CT scans. A total of 179 FCs were identified in 118 (39%) patients with a median age of 68 years and mean FC size of 46.4 mm diameter. As shown in Table 1, 20% received only expectant management, 45% received non-invasive management, and 35% had invasive management. Baseline characteristics including age and structural factors were not associated with management approach. Drain amylase levels differed between the management groups with highest levels observed in the non-invasive group. Size of FC correlated with the invasiveness of management (p <0.001). Radiographic features, specifically the presence of air bubbles and signs of impact on surroundings, were also associated with the type of management (p <0.001 and 0.014, respectively). The majority (57%) of the FCs with air bubbles were treated with invasive measures. Similarly, high rate (42%) of FCs with signs of impact on nearby structures were invasively managed. Regarding anatomic location, 43% of FCs in zone 2 were expectantly managed compared to only 16% of zone 1 FCs (
Figure 1). FCs in zone 1 were most likely to be treated invasively (42%), followed by zone 3 (37%) FCs.
ConclusionDespite the high likelihood of FCs in patients selected for imaging post-PD, only 35% of patients with FCs required invasive interventions. Management varied based on the anatomic location of the collection in the post reconstruction state and features most strongly associated with invasive interventions were the size of FC, presence of air bubbles, and impact of adjacent structures. Future investigations would benefit from standardized reporting of the anatomic location and radiographic features of post-pancreatectomy FCs.
Back to 2024 Abstracts