Back to 2024 Abstracts
ASSOCIATION OF PREOPERATIVE CHOLANGITIS WITH OUTCOMES AND EXPENDITURES AMONG PATIENTS UNDERGOING PANCREATICODUODENECTOMY
Zayed Rashid
*, Selamawit Woldesenbet, Mujtaba Khalil, Muhammad Muntazir Mehdi Khan, Yutaka Endo, Diamantis Tsilimigras, Erryk Katayama, Muhammad Muntazir M. Khan, Abdullah Altaf, Mary Dillhoff, Timothy M. Pawlik
Surgery, The Ohio State Wexner Medical Center, Columbus, OH
Introduction: Preoperative cholangitis (PC) is an important risk factor for postoperative morbidity among patients undergoing pancreatic surgery. We sought to characterize the impact of PC on surgical outcomes and healthcare costs.
Methods: Patients who underwent pancreaticoduodenectomy (PD) between 2013 and 2021 were identified using 100% Medicare Standard Analytic Files. Patients who had at least 1 episode of acute cholangitis within 1-year prior to surgery and who had at least 90 days post-surgery follow-up were included. Multivariable regression analyses were utilized to ascertain variations in the postoperative incidence of surgical site infections (SSI), sepsis, textbook outcomes (TO), as well as healthcare expenditures relative to PC.
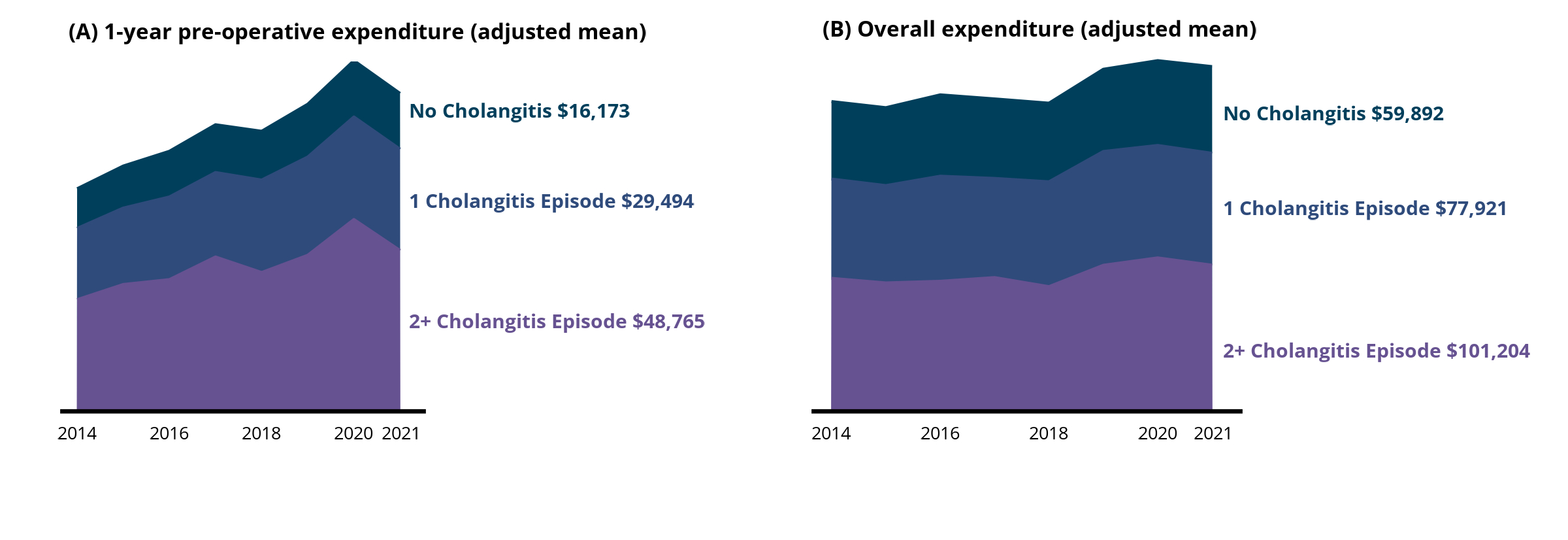
Results: Among 23,455 Medicare beneficiaries who underwent PD, 9.5% (n=2,217) of patients had at least one episode of PC. Median age was 73 years (IQR: 69–78), approximately half were male (n=12,180, 51.9%) and the majority were non-Hispanic White (n=20,354, 86.8%) who underwent PD for a malignant indication (n=14,729, 62.8%). Patients with malignant disease had a higher incidence of PC (malignant: PC, n=1,567, 10.6%; nonmalignant: PC, n=650, 7.4%; all p<0.001). Perhaps not surprisingly, the incidence of PC was higher among patients who required a preoperative endoscopic retrograde cholangiopancreatography (ERCP) with a subset of individuals requiring multiple ERCPs (one ERCP: PC, n=1,046 47.2% vs. no PC, n= 5,227, 24.6%; two ERCPs: PC, n=409, 18.4% vs. no PC, n= 371 1.7%; multiple ERCPs: PC, n=109, 4.9% vs. no PC, n=23, 0.1%; all p<0.001). On multivariable analyses, PC was associated with elevated odds of SSI (OR 1.14, 95%CI 1.01-1.29), sepsis (OR 1.17, 95%CI 1.01-1.37), extended length of stay (OR 1.13, 95%CI 1.01-1.26), as well as readmission within 90-days (OR 1.14, 95%CI 1.04-1.26) (all p<0.05). In turn, patients with a history of PC prior to PD had a reduced likelihood of achieving a TO (OR 0.83, 95%CI 0.75-0.92; p<0.001). Moreover, the incidence of PC was associated with increased preoperative (ref. No PC; percent difference [%diff] 87.79, 95%CI 79.51–96.44; p<0.001) and postoperative (%diff 18.44, 95%CI 9.75-27.82; p<0.001) healthcare costs. In fact, overall healthcare costs increased substantially among patients with more than one PC episode (no episode: $59,893, 95%CI $57,827–$61,959 vs. one episode: $77,922, 95%CI $73,854–$81,990 vs. multiple episodes: $101,205, 95%CI $94,871–$107,539) (
Figure).
Conclusion: Roughly 1 in 10 patients undergoing PD experienced an antecedent PC episode, which was associated with adverse surgical outcomes and greater healthcare expenditures. Prevention and management of PC among patients undergoing PD should be targeted for quality improvement efforts.
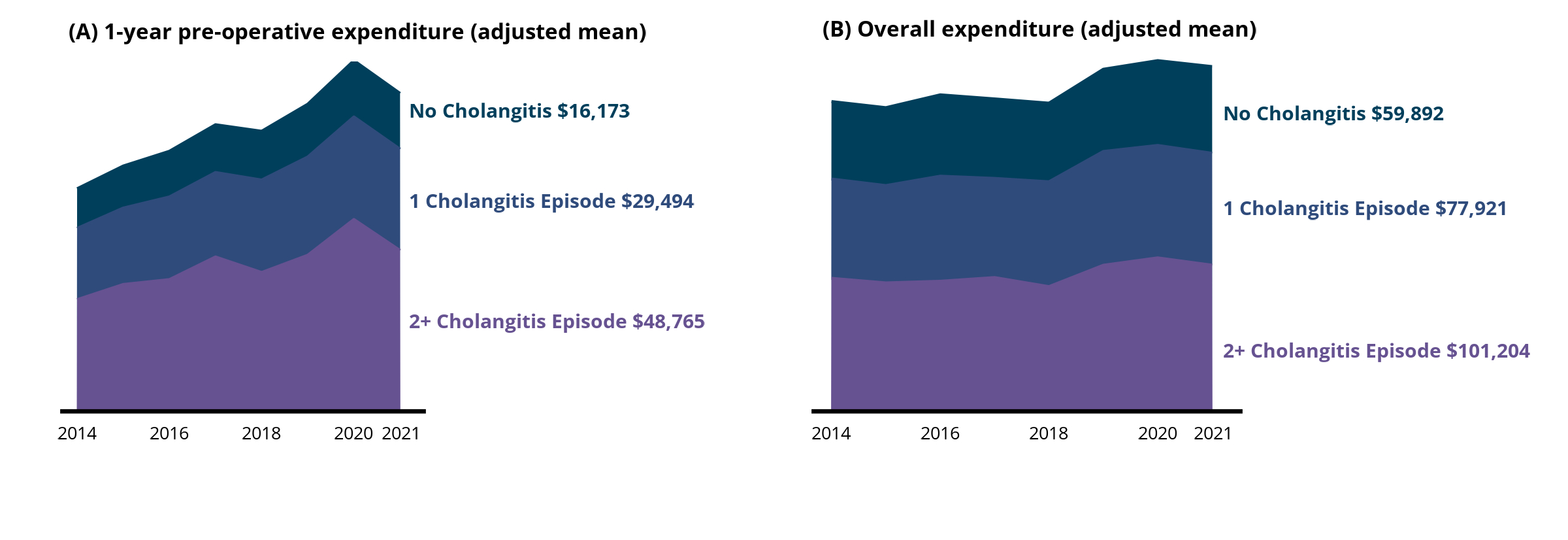
Trends in healthcare costs relative to the number of preoperative cholangitis episodes among patients undergoing pancreaticoduodenectomy.
Back to 2024 Abstracts