Back to 2024 Abstracts
GASTROPEXY ALONE FOR GIANT PARAESOPHAGEAL HERNIA (PEH)?
Gregory T. Kennedy
*, Feredun Azari, Nicholas Kelly, Amy Lorenzo, Daniel Dempsey
Surgery, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA
Background: Chronic morbidity and/or symptomatic recurrence remain problematic after operation for large PEH (type II, III, IV with >30% stomach in mediastinum), often performed for mechanical symptoms (not GERD) in frail elderly patients. Laparoscopic gastropexy alone(LG) may be a reasonable treatment option, but data comparing the long term outcomes of LG to laparoscopic formal repair (LFR) are lacking. The purpose of this study is to evaluate the hypothesis that treatment outcomes of LG are noninferior to LFR in patients with large PEH and predominant mechanical symptoms.
Methods: After IRB approval, patients who had undergone an elective initial operation for PEH by a single surgeon were interviewed and completed an outcomes survey including GI Quality of Life Index (GIQOLI) and Eckardt Score. EMR was reviewed for demographic and perioperative variables. Statistical analysis was done with SPSS version 27. In LG (performed only for mechanical non-GERD symptoms and very large hernia), stomach was reduced (no sac or crural dissection) and approximated to the LUQ with 8 to 12 heavy nonabsorbable transfixing sutures (greater curvature to full thickness musculofascial abdominal wall). LFR consisted of sac removal, esophageal mobilization, complete hernia reduction, posterior crural repair (no mesh), and posterior hemifundoplication (no esophageal lengthening).
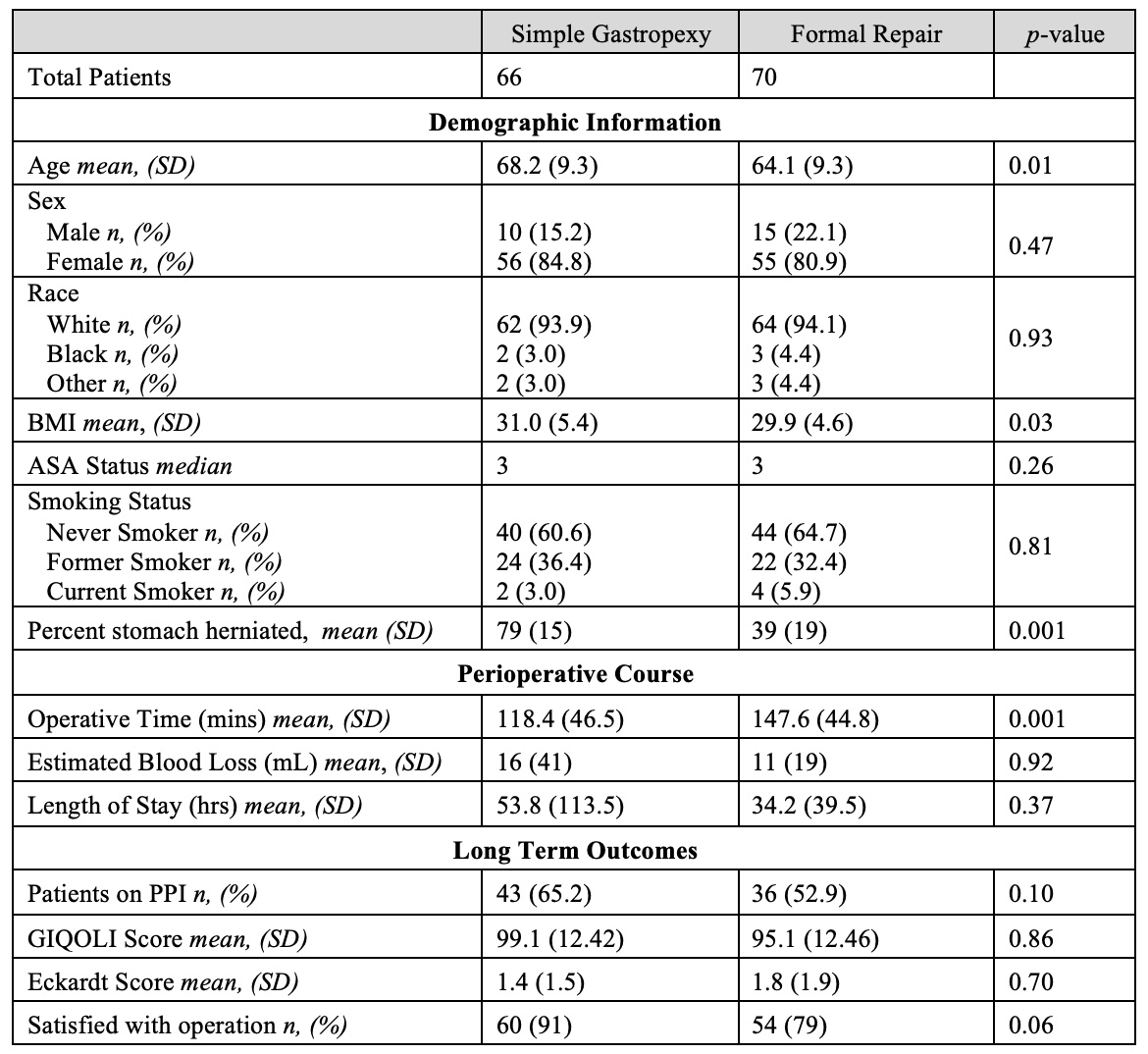
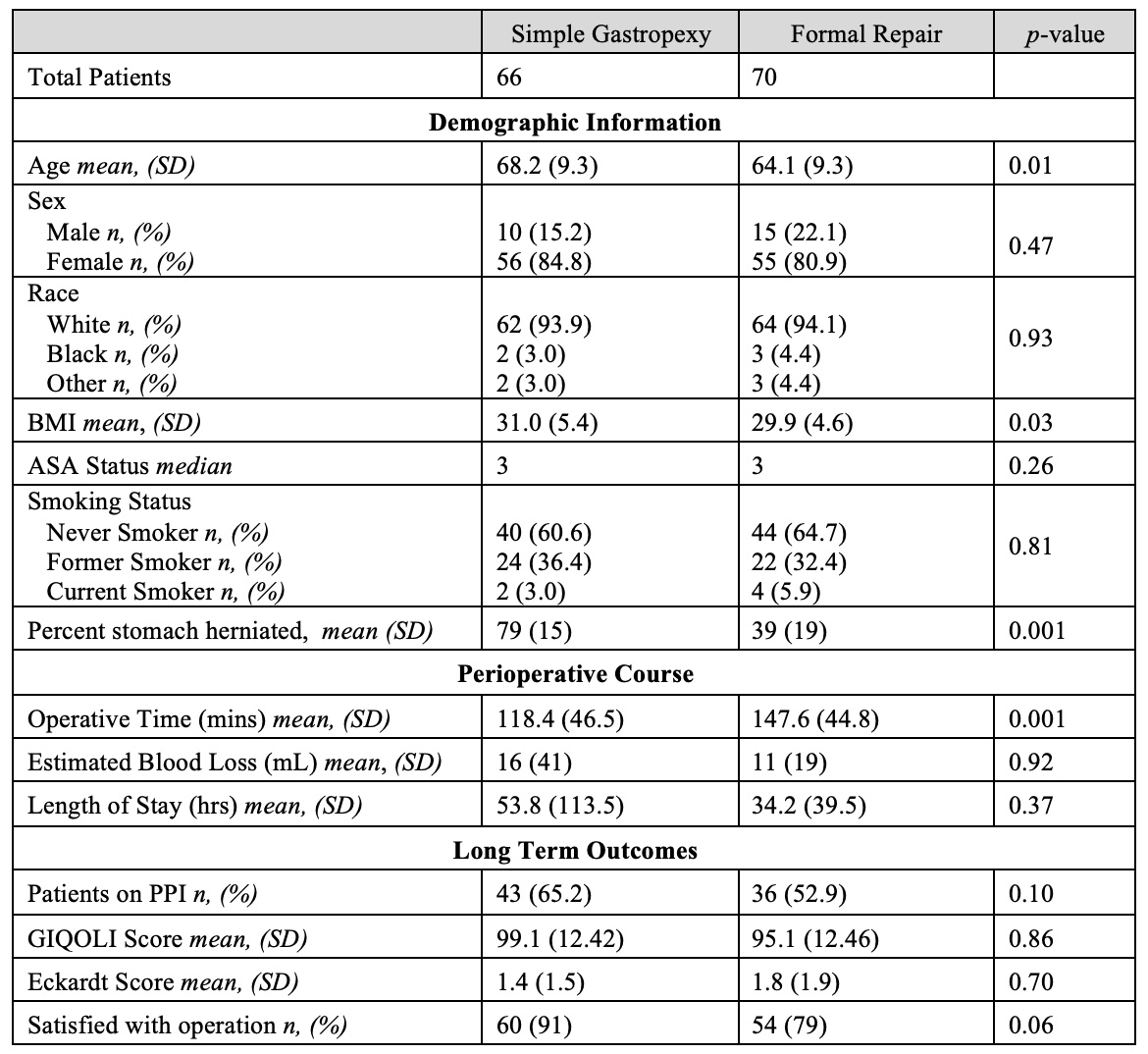
Results (Table): The study population consisted of 136 patients with first time elective operations (66 LG and 70 LFR). There were no mortalities and no conversions to open operation. Mean follow up was 5.8 years (IQR: 4.2-7.1 years). LG group was older (mean age 68.2 v. 64.1yrs,
p=0.007), with more herniated stomach (79% v. 39%, p=0.001) and shorter operation (118.5±46.5 v. 147±44.7 minutes,
p=0.001). LG group also had higher BMI. There were no other significant demographic or perioperative differences between the two cohorts. From a functional perspective (PPI use, GIQOLI, Eckardt Score), LG was not inferior to LFR. There was a trend to higher satisfaction in the LG group (
p=0.06).
Conclusions: LG is a reasonable option for large PEH with predominant mechanical symptoms in elderly patients. An RCT comparing LG to LFR in this group should be considered.
Back to 2024 Abstracts