Back to 2024 Abstracts
PYLORIC IMPEDANCE PLANIMETRY DURING ENDOSCOPIC PER-ORAL PYLOROMYOTOMY (POP) GUIDES MYOTOMY EXTENT
Hee Kyung (Jenny) Kim
*3,1, Jamie DeCicco
2,1, Rachna Prasad
4,1, Hemasat Alkhatib
1,3, AJ Haas
1,3, Ali M. Kara
1,3, Clara Kit Nam Lai
1,3, Alejandro Feria
1,3, Sergio Bardaro
1,3, Amelia Dorsey
1,3, Kevin El-Hayek
1,3,41Surgery, The MetroHealth System, Cleveland, OH; 2Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH; 3Case Western Reserve University School of Medicine, Cleveland, OH; 4Northeast Ohio Medical University, Rootstown, OH
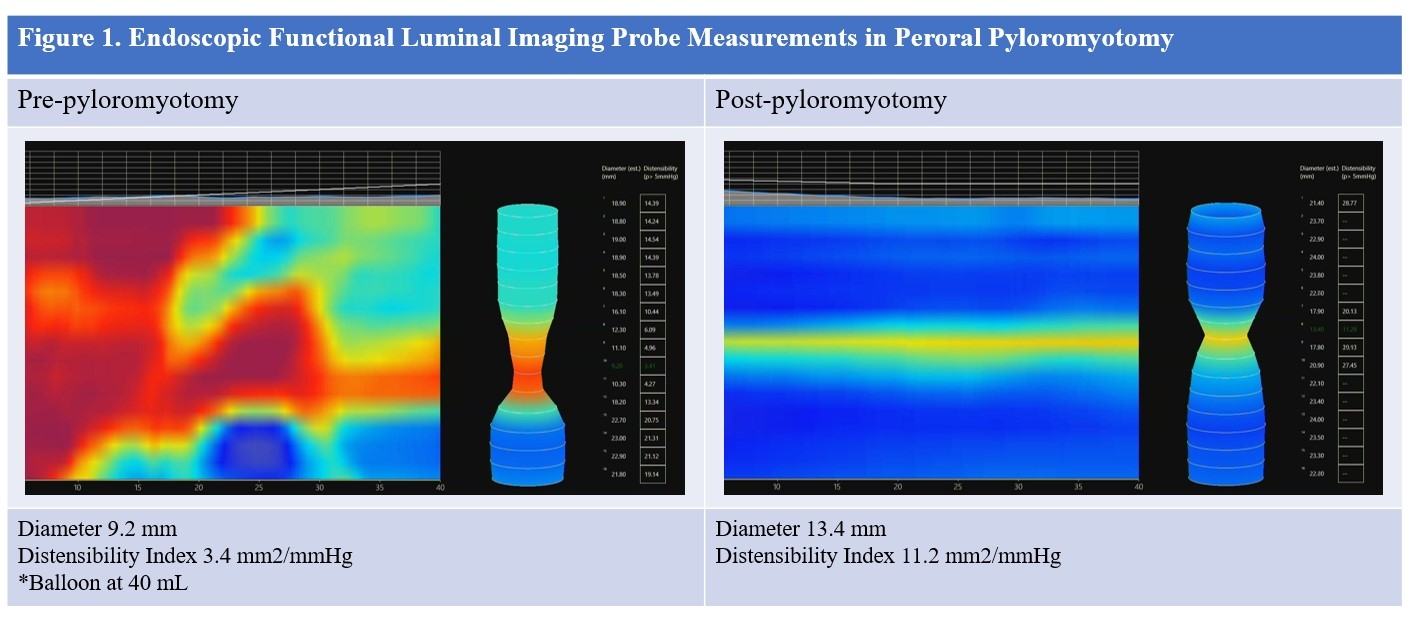
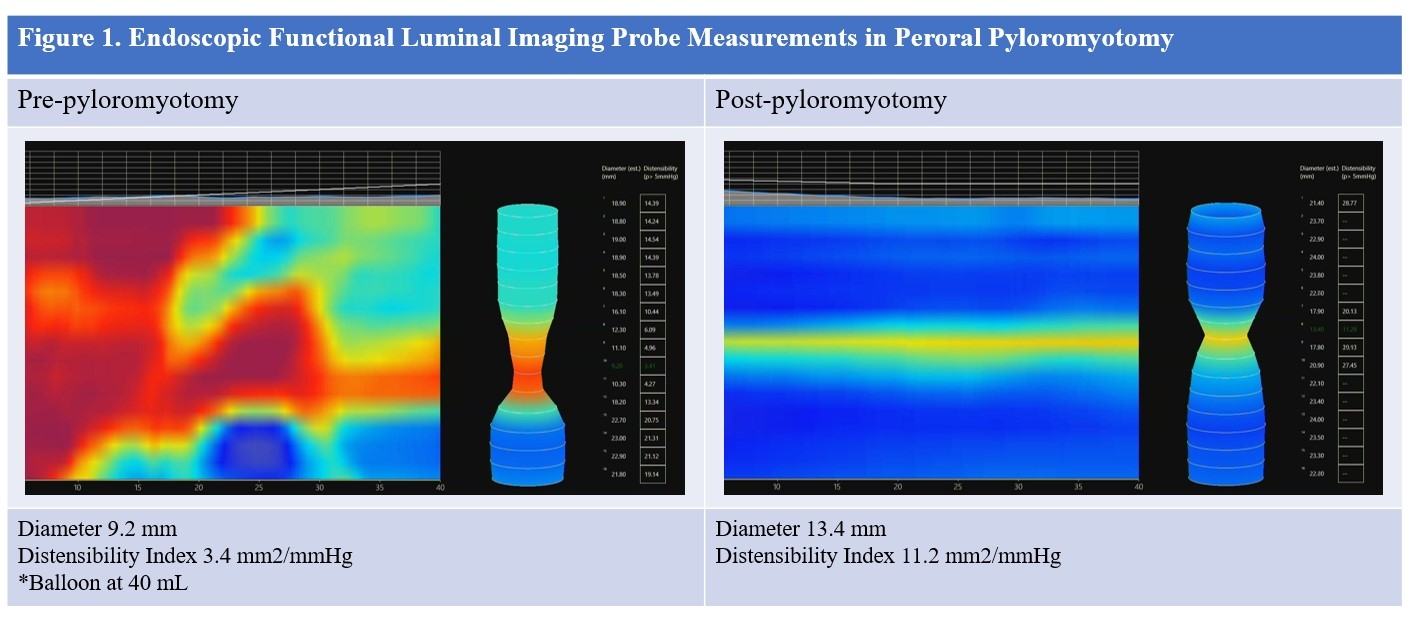
INTRODUCTION: Peroral pyloromyotomy (POP) is the first-line endoscopic intervention for medically refractory gastroparesis during which functional luminal imaging probe (FLIP) can be utilized to perform pyloric impedance planimetry. While FLIP is a safe way to objectively measure pyloric distensibility to guide treatment, its predictive value is poorly understood. Our study aimed to evaluate use and outcomes of real-time impedance planimetry with FLIP during POP. Secondary aims focused on evaluating the predictive ability of pre- and post-POP FLIP values in improving in symptoms and objective gastric emptying.
METHODS: A retrospective review was conducted from October 2019 to June 2023 of patients who received POP. FLIP measurements, symptoms measured by the validated gastroparesis cardinal symptom index (GCSI), and scintigraphic gastric emptying studies (GES) were evaluated before and after POP.
RESULTS: Twenty-nine patients (25 [86%] female, age 49.8±17.2 years, BMI 28.3±5.3 kg/m
2) underwent POP. Gastroparesis etiologies included 14 post-surgical (48%), 5 diabetes mellitus (17%), and 10 idiopathic (35%). Intraoperatively, 15 patients had FLIP measurements before and after pyloromyotomy. Mean pyloric diameter increased from 12.8±3.3 to 16.1±2.6 mm (t=4.26, p=0.0008). Median distensibility index (DI) increased from 4.5 (3,5) to 9 (6.3,11) mm
2/mmHg (S=60, p<0.0001). Management changed based on FLIP values for 3 patients (20%), prompting additional myotomy. Average operative time was 39.8±16.1 minutes. There were no complications. At 17 (11,18) days post-procedure, median GCSI score decreased from 32/45 (25,38) preoperatively to 17/45 (9,26) postoperatively (S=-131.5, p<0.0001). At mean follow-up of 4.4 (3.7,8.8) months, improvement in GCSI score persisted with a median score of 21/45 (13,29) (S=93, p<0.0001). Improvements occurred across all symptom categories including nausea, vomiting, early satiety, and bloating. Median retention at 4 hours on GES decreased from 29.0% (16.5,57.5) preoperatively to 15.5% (4.3,32.5) at 3.2 (2.9,3.9) months post-procedure (S=-71, p=0.0062). There was 75% improvement and 40% normalization of objective gastric emptying in patients who had pre- and post-POP GES (n=20).
CONCLUSION: POP with FLIP resulted in clinical and radiographic improvement in patients with gastroparesis. FLIP detected insufficient increase in diameter and DI for 20% of patients who had FLIP, changing operative management. There were no other indications that these patients would have required more extensive myotomy, highlighting the distinct utility of FLIP. The additional intervention was not associated with adverse outcomes, and these patients had equivalent outcomes to their counterparts who did not need additional myotomy. Future research will focus on long-term outcomes to better elucidate potential benefits of FLIP-guided POP procedures.
Back to 2024 Abstracts