Back to 2024 Abstracts
ONCOLOGIC OUTCOMES AFTER POUCH EXCISION: IS THERE A DIFFERENCE BETWEEN IBD AND FAP POUCH NEOPLASIA?
Megan Obi
*, Mikhael Belkovsky, Sarah Choi, Jie Dai, Tracy L. Hull, Olga Lavryk, Jeremy M. Lipman, David Liska, Joshua Sommovilla, Benjamin L. Cohen, Taha Qazi, Emre Gorgun, Scott Steele, Stefan D. Holubar
General Surgery, Cleveland Clinic, Cleveland, OH
BackgroundIleoanal pouch patients are at risk of neoplasia of the rectal cuff/anal transitional zone (ATZ) and the pouch, but it is unknown whether underlying diagnosis that impacted pouch construction affects oncologic outcomes after pouch excision. We hypothesized that patients with a history of inflammatory bowel disease (IBD) compared to those with a history of polyposis or prior cancer would have worse overall- and disease-free survival.
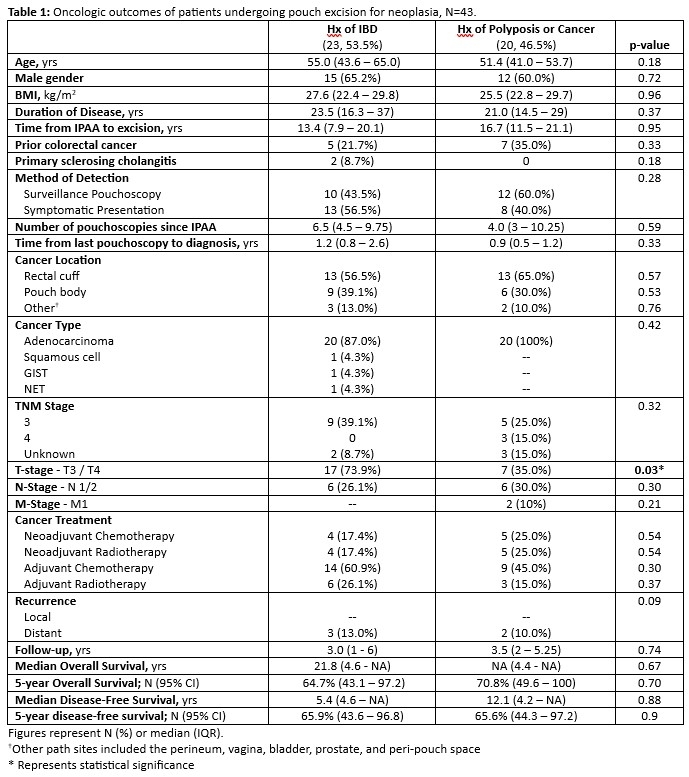
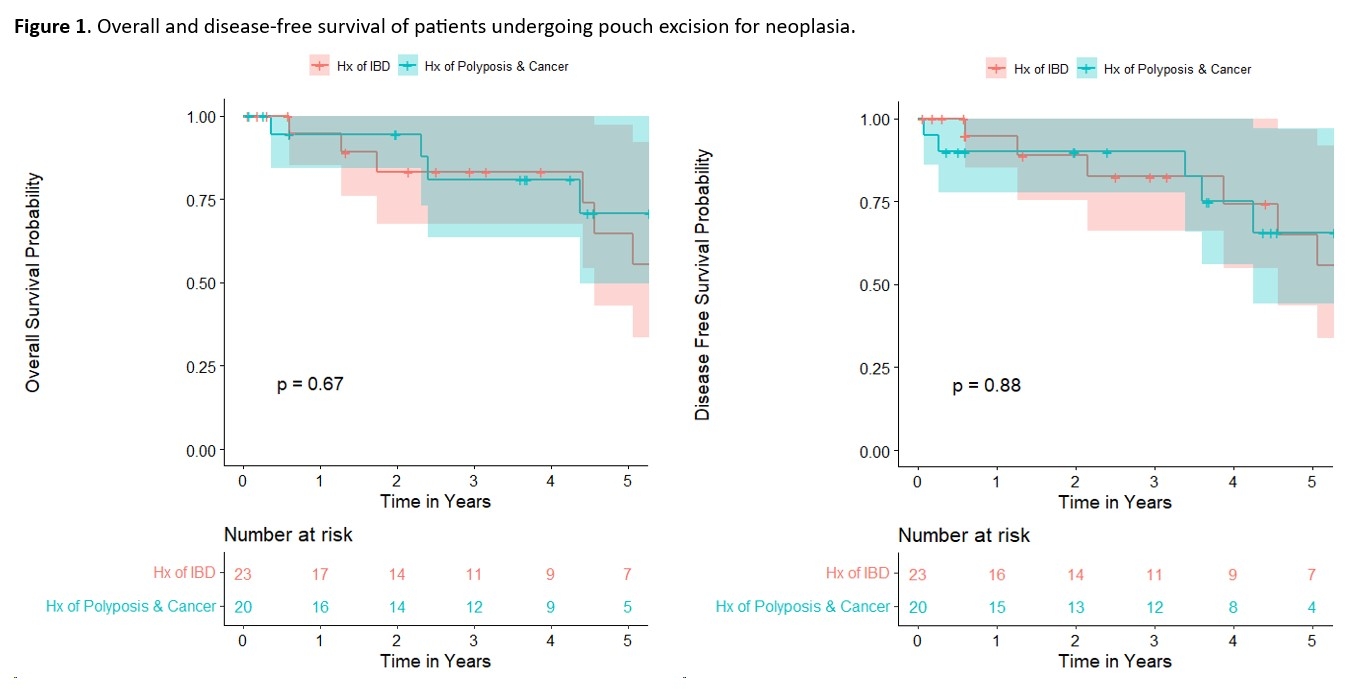
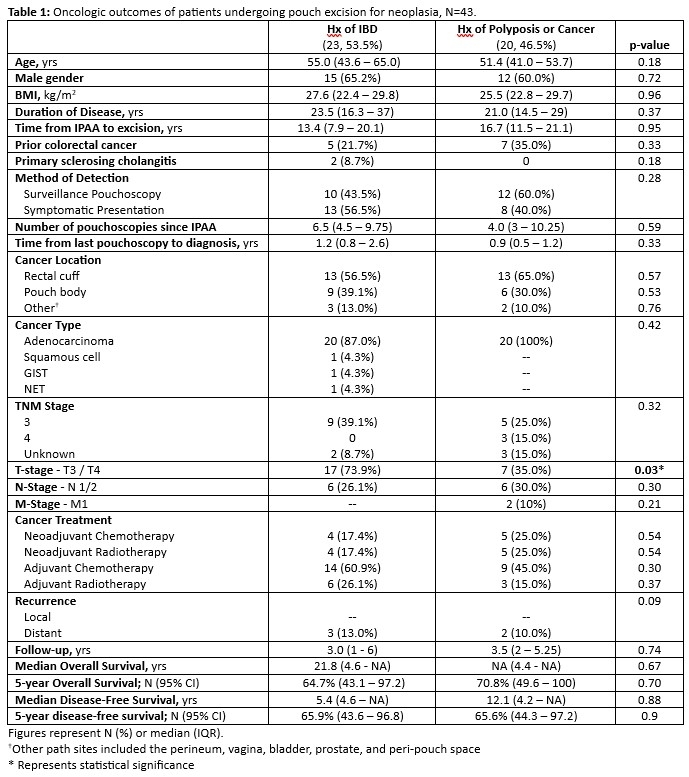
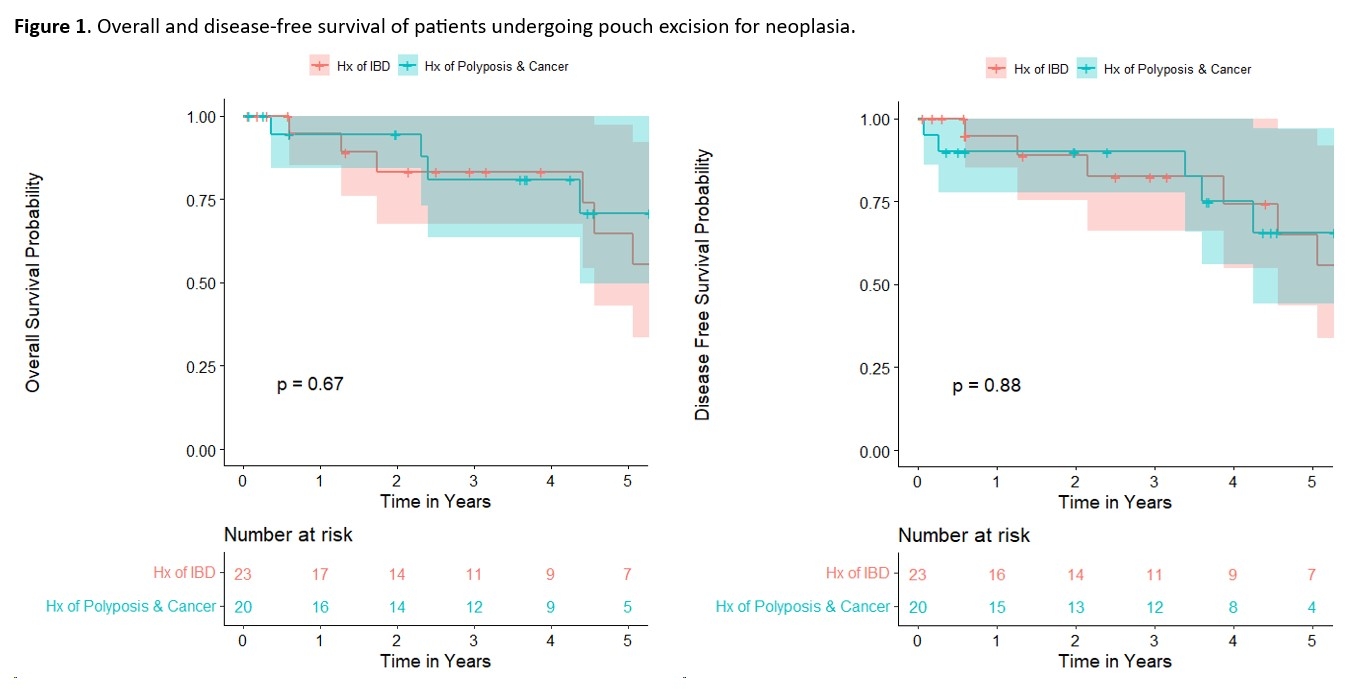
MethodsWe retrospectively reviewed a prospectively maintained database for all adult patients who underwent IPAA excision between 1984 and 2023. Pouch excisions with malignancy at any component of the specimen on final pathology were included. Patients with preoperative dysplasia but no cancer on final pathology were excluded. Patients were stratified by preoperative diagnosis, IBD vs. polyposis/cancer, and compared using Kaplan-Meier analysis.
Results A total of 814 patients underwent pouch excision, 43 (5.3%) of whom were found to have cancer on pathology. Median age at time of pouch excision was 52 years (IQR 41.8 - 59.3); 62.8% were male, 9.3% were non-white, and median BMI was 27.1 kg/m
2 (IQR 22.4 - 29.8). IBD was the underlying diagnosis in 23 (53.5%) patients and 20 (46.5%) had polyposis or cancer; 4.7% and 9.3% were receiving biologics and steroids, respectively, before their pouch excisions. Median time to excision was 16 years (IQR 9.6- 20.8), and 34 (79.1%) excisions were performed for cancer or high-grade dysplasia detected on pouchoscopy. Neoadjuvant chemoradiation was used in 9 (20.9%) cases. Two of the pouch excisions were performed robotically, and the remainder were performed open. Intraoperative complications occurred in 13 (30.2%) cases. Thirty (69.8%) patients had post-op complications. Thirteen (30.2%) patients required readmission because of postoperative complications, and the median time to readmission was 17 days. The most common histology was adenocarcinoma (40, 93.1%), with single instances of GIST, NET, and squamous cell carcinoma. Cancer locations were rectal cuff/ATZ (41.8%), pouch body (34.8%), other 5 (11.6%). Stage 2 and 3 diseases were found in 39.5% and 32.56% of cases, respectively, and IBD patients were more likely to present with T3/4 disease (p = 0.03). After pouch excision, 4 (9.3%) patients underwent surveillance only, whereas most patients (53.5%) underwent adjuvant chemotherapy treatment. The 5-year overall- and disease-free survival were 67% (CI 51-89%) and 64% (CI 47-86%) and did not differ between groups.
ConclusionsIBD-associated ileoanal pouch cancers tended to present at a more advanced T-stage than FAP/cancer patients, but long-term oncologic outcomes did not amongst the two groups.
Back to 2024 Abstracts