Back to 2024 Abstracts
DOES MESORECTAL FASCIA INVOLVEMENT (MRF) AFFECT THE RESPONSE TO TNT IN LOCALLY ADVANCED RECTAL CANCERS?
Kamil Erozkan
*, Doua Elamin, Enes Tasci, David Liska, Michael Valente, Ali Alipouriani, Lukas Schabl, Olga Lavryk, Brogan Catalano, Jacob Miller, Andrei Purysko, Scott Steele, Emre Gorgun
Colorectal Surgery, Cleveland Clinic, Cleveland, OH
Background: In the treatment of locally advanced rectal cancer (LARC), there has been a paradigm shift towards the routine use of total neoadjuvant treatment (TNT). Despite its growing acceptance, there are limited studies examining factors predictive of response to TNT. Our previous series with 119 patients revealed that the complete response (CR) rate was 37%, and low rectal tumors and the absence of extramural vascular invasion (EMVI) were associated with CR. Due to low numbers in previous publications, only a limited number of factors were able to be evaluated. Therefore, we aim to determine factors associated with CR.
Methods: A retrospective analysis of patients who completed TNT for LARC at our tertiary care center between 2015 and 2022 was performed. Our primary outcome was to determine predictors of CR. As a secondary outcome, we evaluated the 2-year disease-free and overall survival rates. Complete response (CR) was defined as patients who sustained clinical CR (cCR) for at least 12 months under watch-and-wait (WW) or had a pathological CR (pCR) after surgery.
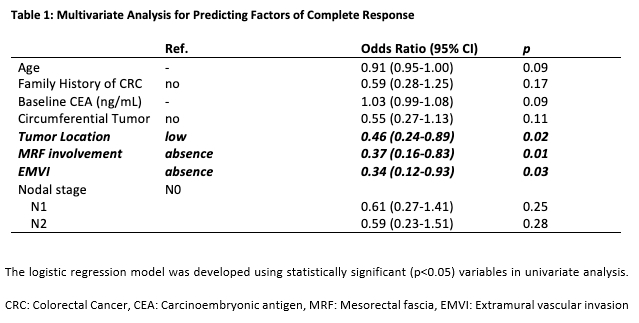
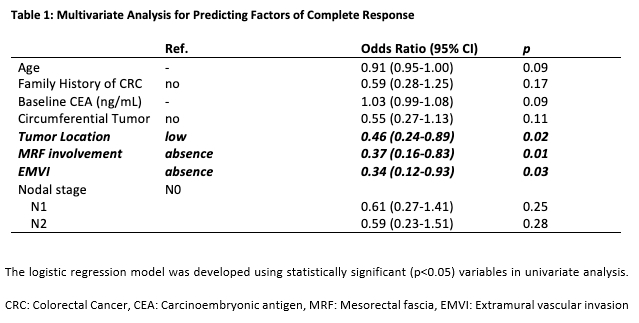
Results: Out of 339 patients with LARC, 208 (61.3%) successfully completed TNT. Among them, 57 (27.4%) patients achieved cCR, and 80% developed no tumor regrowth after 1 year of follow-up. The remaining 151 (72.6%) patients underwent surgery, and 42 had pCR. The final CR rate was 42.3%. The median age of the patients was 56 (49-66), and 63.5% of the participants were male (n=132), while 36.5% were female (n=76). The median tumor size was 4.95 cm (3.6-6.43), with most tumors in the low rectum (119, 57.2%). The MRF involvement rate was 25% (n=52), and EMVI was observed in 20.7% of patients (n=43) based on MRI findings. Low rectal tumors, the absence of MRF involvement, and the absence of EMVI were associated with a CR (Table 1). With a median follow-up of 24.7 months, 2-year disease-free survival and overall survival were significantly higher among patients with a CR (91.3% vs 71%, p< 0.01 and 98.8% vs 90.2% p=0.03, respectively).
Conclusion: In our updated dataset, we observed an increasing CR rate compared to our previous study. We found the absence of MRF involvement, the absence of EMVI, and low tumor location to be associated with a CR.
Print
Back to 2024 Abstracts