Back to 2024 Abstracts
ENDOSCOPIC THERAPIES FOR POST-BARIATRIC GASTRIC SLEEVE LEAKS: A COMPREHENSIVE 10-YEAR ANALYSIS OF EFFICACY, SAFETY, AND OUTCOMES
Kimberly F. Schuster
*1,2, Cem Simsek
3, Christopher C. Thompson
11Division of Gastroenterology, Hepatology and Endoscopy, Brigham and Women's Hospital, Boston, MA; 2Tufts University School of Medicine, Boston, MA; 3Hacettepe Universitesi Tip Fakultesi, Ankara, Ankara, Turkey
Introduction:Gastric leaks represent a formidable complication of bariatric surgery. The absence of a standardized algorithm for leak management, coupled with intricate anatomical factors like stenosis or angulation, renders leaks uniquely challenging to treat. This study aims to evaluate endoscopic therapy outcomes, efficacy and safety for sleeve leaks post-bariatric surgery.
Method:We performed a 10-year (2010-2020) retrospective analysis of a prospectively maintained database of bariatric surgery patients with development of sleeve leaks. Primary outcomes were technical success of endoscopic therapies and clinical symptom resolution. Secondary outcomes included need for additional interventions, recurrence, and adverse events. Statistical tests included T-test, X2, and multivariate logistic regression, with p<0.05 significant.
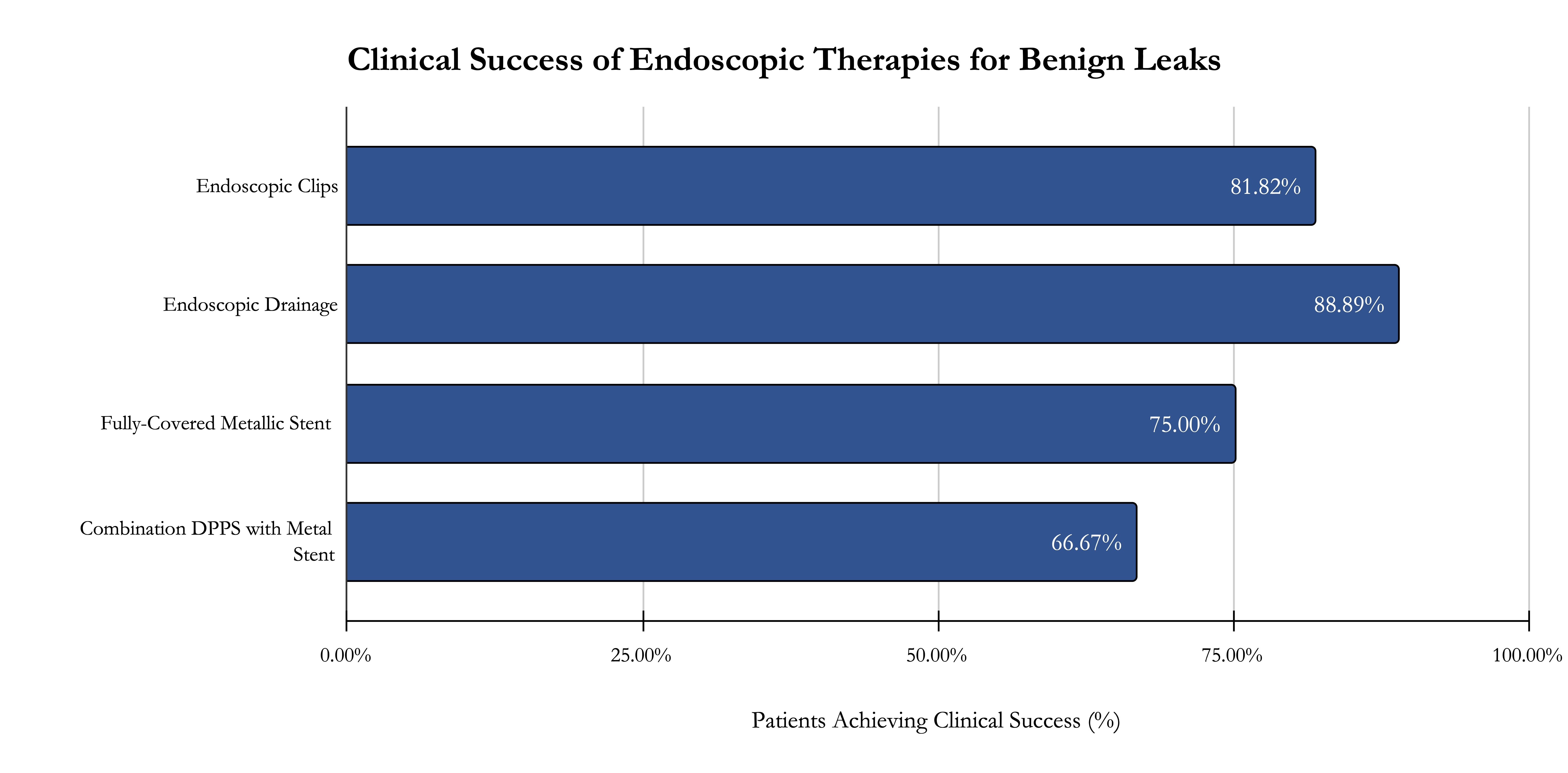
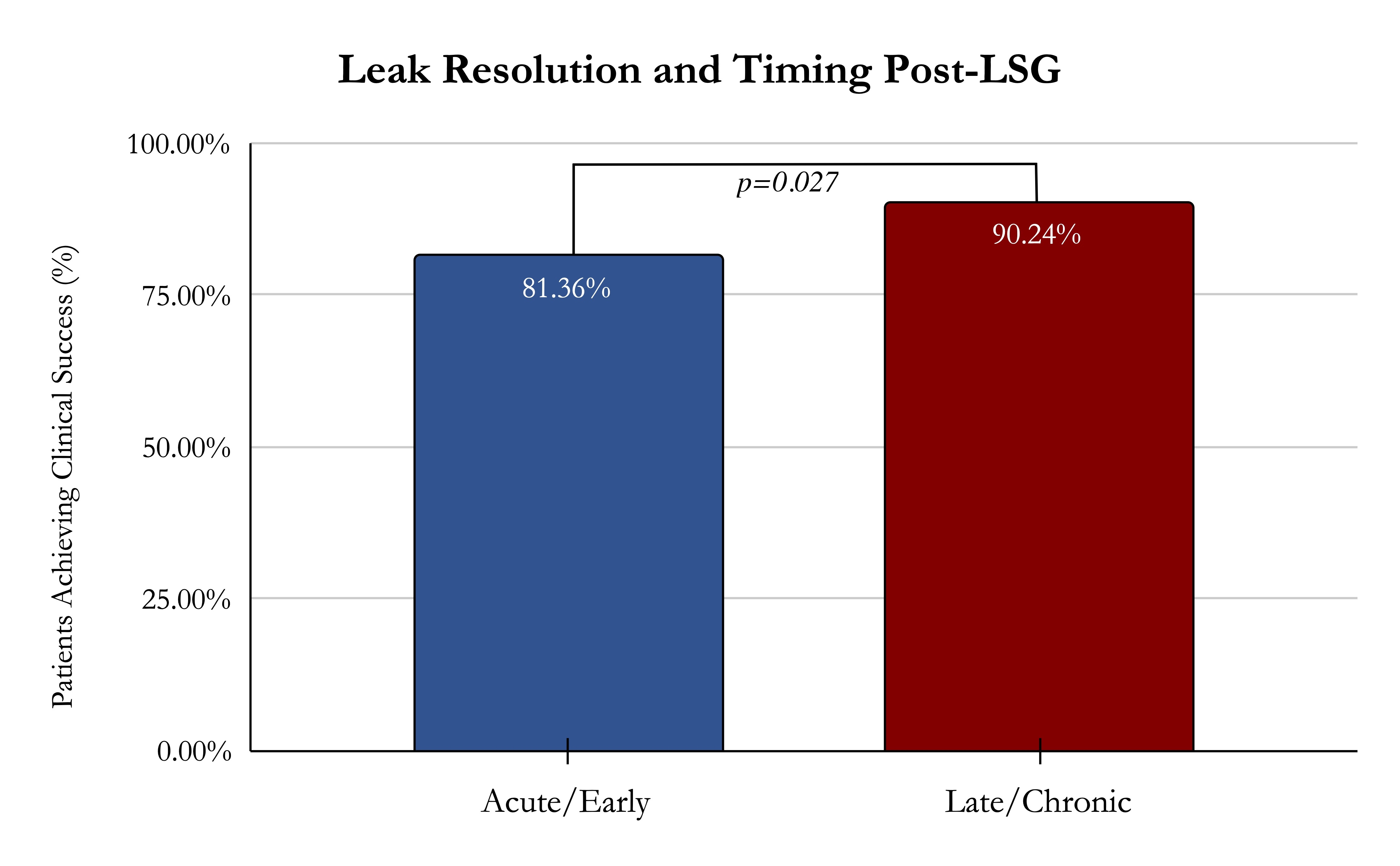
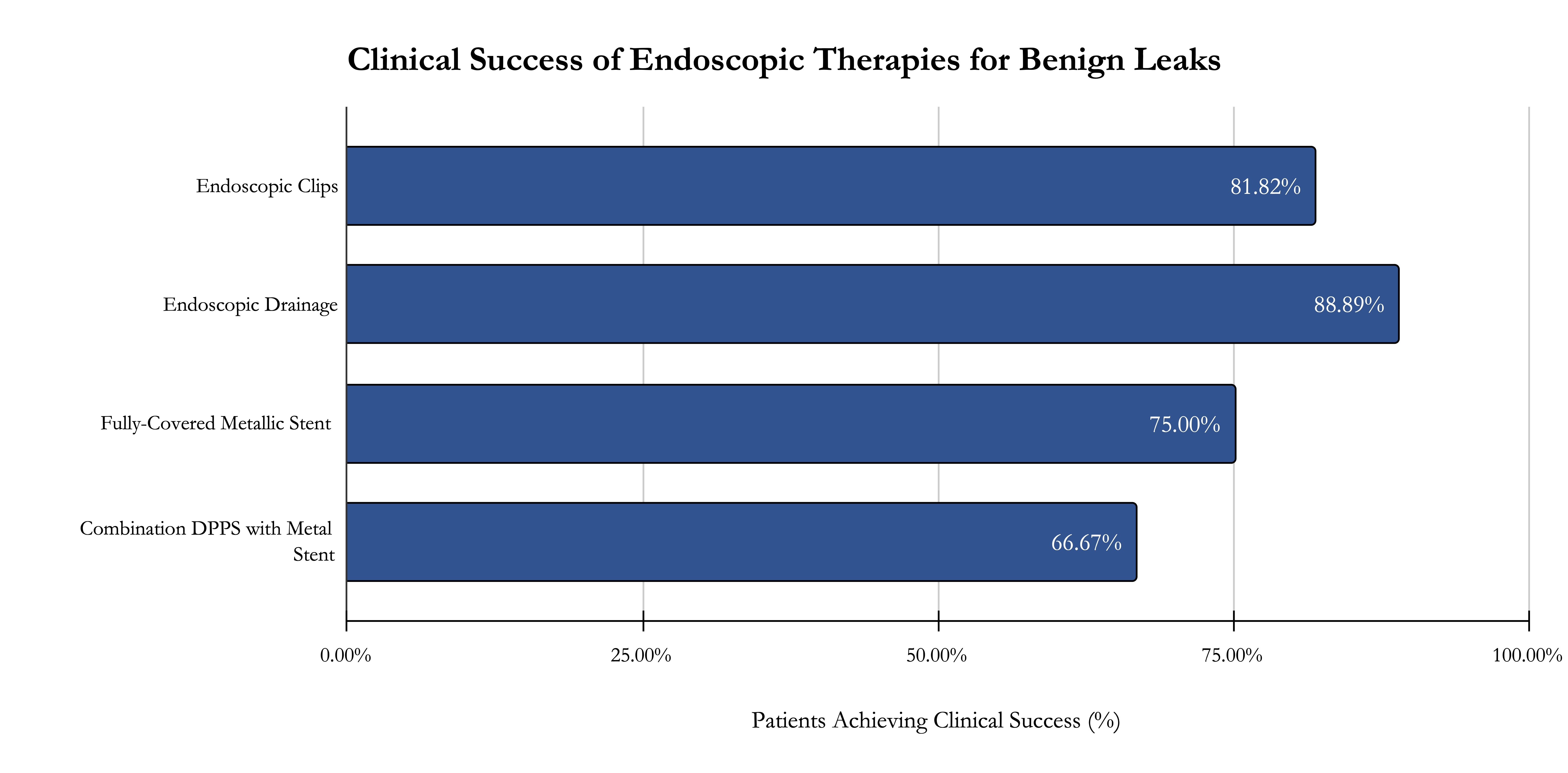
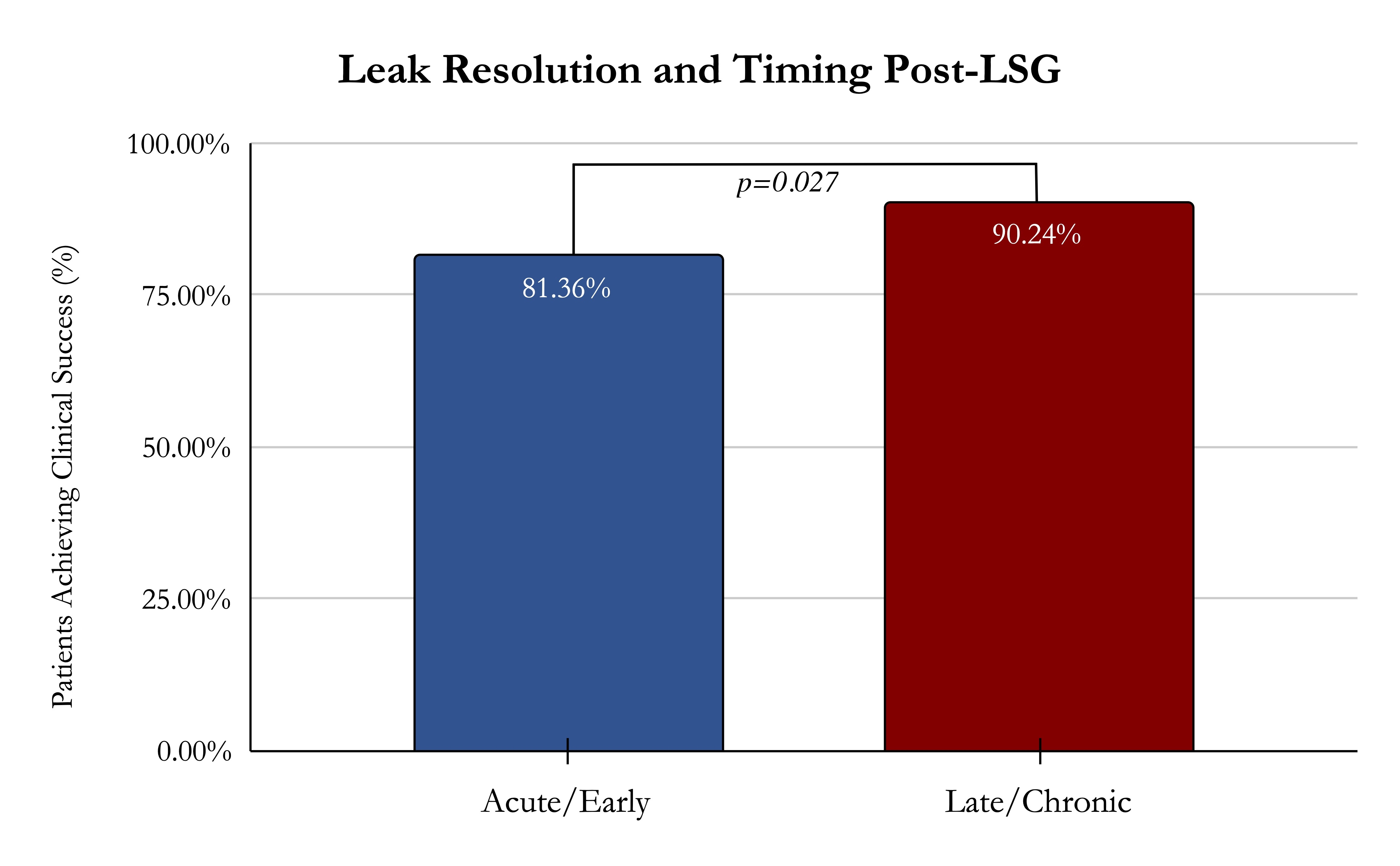
Results:Of 9,930 bariatric surgery patients, 101 (1.08%) experienced postoperative gastric leaks, with breakdowns by procedure: 86 from sleeve gastrectomy, 14 from Roux-en-Y gastric bypass, and 1 from duodenal switch. Demographics included 71% females, mean age 52.8±12.4 years, and preoperative BMI 43.1±8.3 kg/m2. Median time to leak manifestation was 60.5 weeks (IQR: 14-151). Leaks were categorized as acute (n=22), early (n=37), late (n=17), or chronic (n=25). Symptoms varied, and 26 cases were asymptomatic. Proximal sleeve leaks were predominant (90.5%), followed by distal (8.3%) and middle (1.2%) thirds. Mean diameter was 2.7±2.3cm; 48.5% had concurrent sleeve stenosis treated with endoscopic dilation. Sixteen critically ill patients underwent emergent laparotomy. Intravenous antibiotics alone were provided to 27 patients (31%), and drainage involved endoscopic (n=36) or interventional radiology (n=32) procedures. Treatments included conservative management (5.8%), endoscopic clips (12.7%), double pigtail plastic stents (35.6%), and esophageal stents (58.1%), with a mean dwell time of 50.1 days (Figure 1). Stent-related complications occurred (migration n=14, ulceration n=2). On average, patients underwent 2.1 endoscopic treatments, achieving technical success in all and clinical success in 77.6%. Among failures, 10 patients underwent Roux-en-Y Gastric Bypass conversion, with 3 experiencing subsequent leaks. Complications occurred in 22 patients, and mean follow-up was 69.7±90.7 months, with a 1.9% (n=2) mortality rate. Regression analyses linked chronicity to endoscopic success and smoking history to failure (p=0.012). Success rates for late/chronic versus acute/early leaks were 90.2% and 81.4%, respectively (p=0.027) (Figure 2).
Discussion:This study underscores the complexity of gastric leaks post-bariatric surgery. Endoscopic treatment is an effective alternative for leak management, with chronicity and non-smoking associated with higher success rates.
Back to 2024 Abstracts