Back to 2024 Abstracts
RISK FACTORS FOR REGROWTH AFTER NONOPERATIVE MANAGEMENT FOR RECTAL CANCER
Neal Bhutiani
*, Kentaro Ochiai, Tsuyoshi Konishi, Oliver Peacock, Y. Nancy You, Brian K. Bednarski, Craig A. Messick, Atsushi Ikeda, Michael White, John M. Skibber, George J. Chang, Abhineet Uppal
Surgical Oncology, The University of Texas MD Anderson Cancer Center Division of Surgery, Houston, TX
BackgroundRecently, nonoperative management (NOM) for rectal cancer has demonstrated promise as a viable treatment strategy that allows a subset of patients to safely avoid rectal resection. However, despite initial excellent response on post-treatment radiographic and clinical examination, a subset of patients experience regrowth of their tumor and require salvage rectal resection. We sought to identify clinicopathologic factors associated with tumor regrowth to assist in patient selection for NOM.
Methods Patients receiving treatment for rectal cancer at a single NCI-designated Comprehensive Cancer Center in whom NOM was pursued based on a complete clinical response (cCR) or near-complete response (nCR) were identified. Patients with metastatic disease, treated with immunotherapy, or who were not surgical candidates or declined surgery, were excluded. Patients were stratified with respect to initial endoscopic findings (incomplete, near-complete: nCR or complete clinical response: cCR) after completion of all planned radiotherapy and/or chemotherapy. Groups were compared with respect to tumor characteristics and treatment details to identify factors associated with regrowth-free survival (RFS).
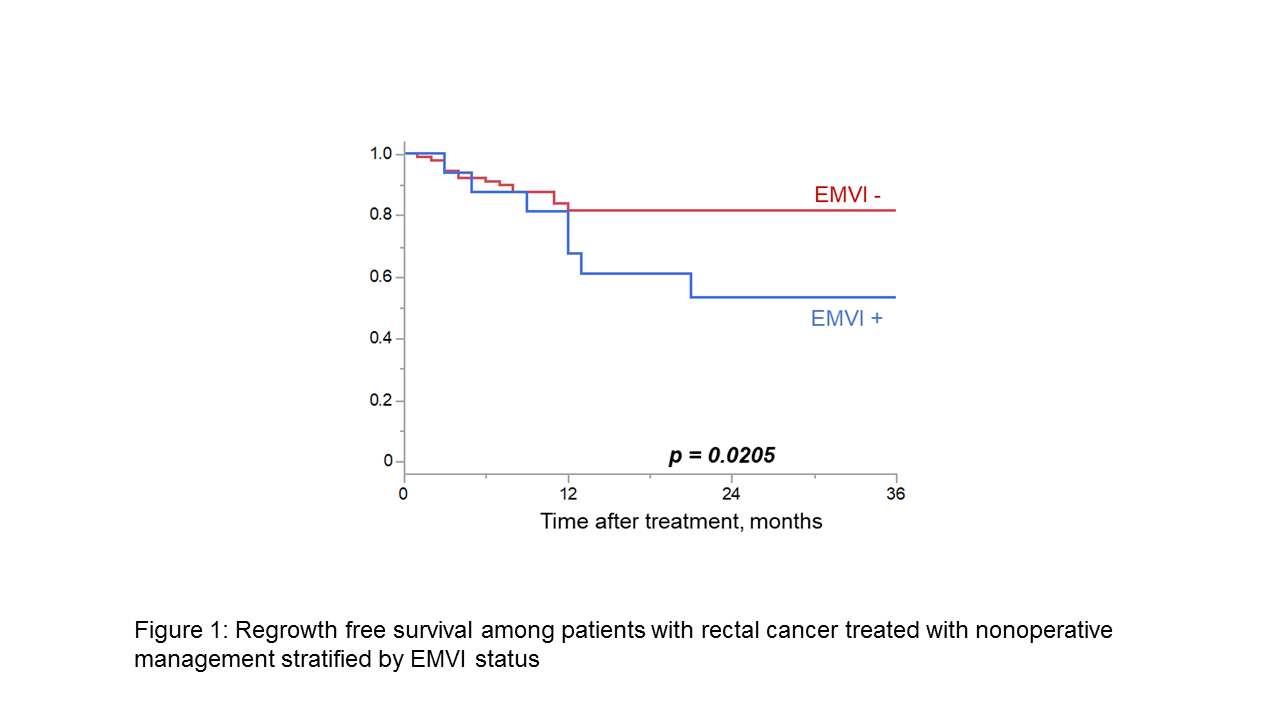
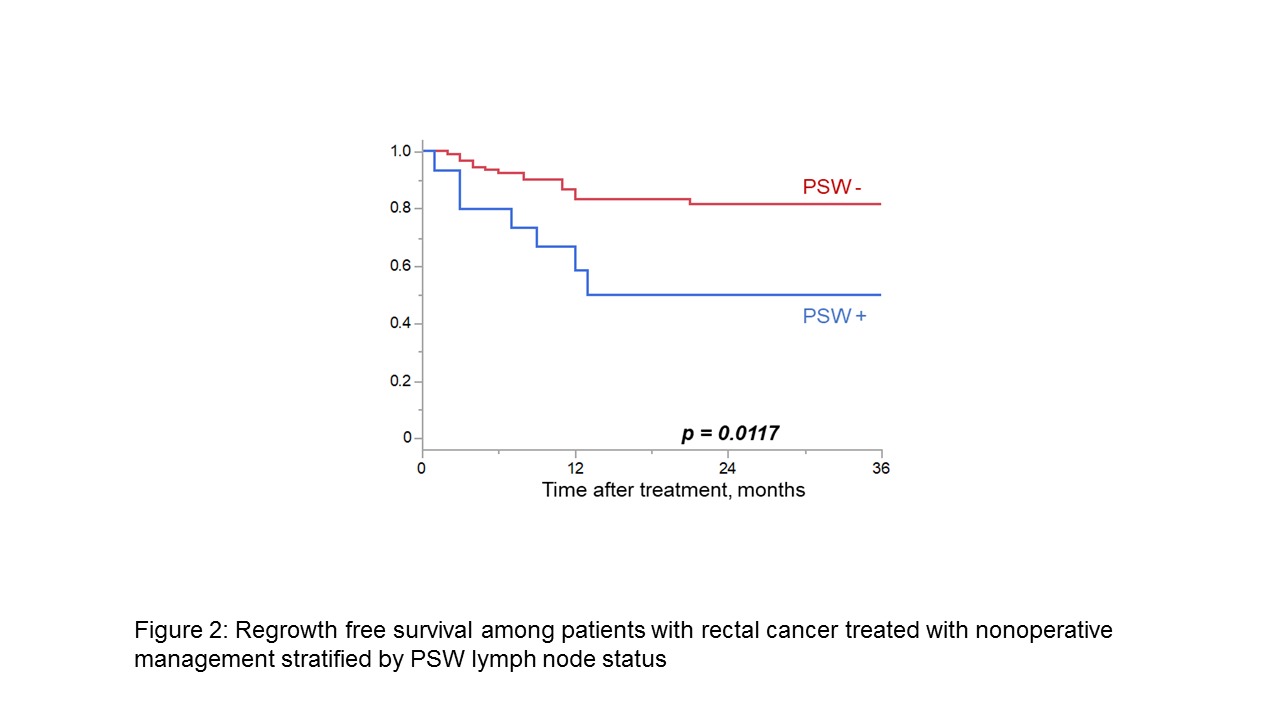
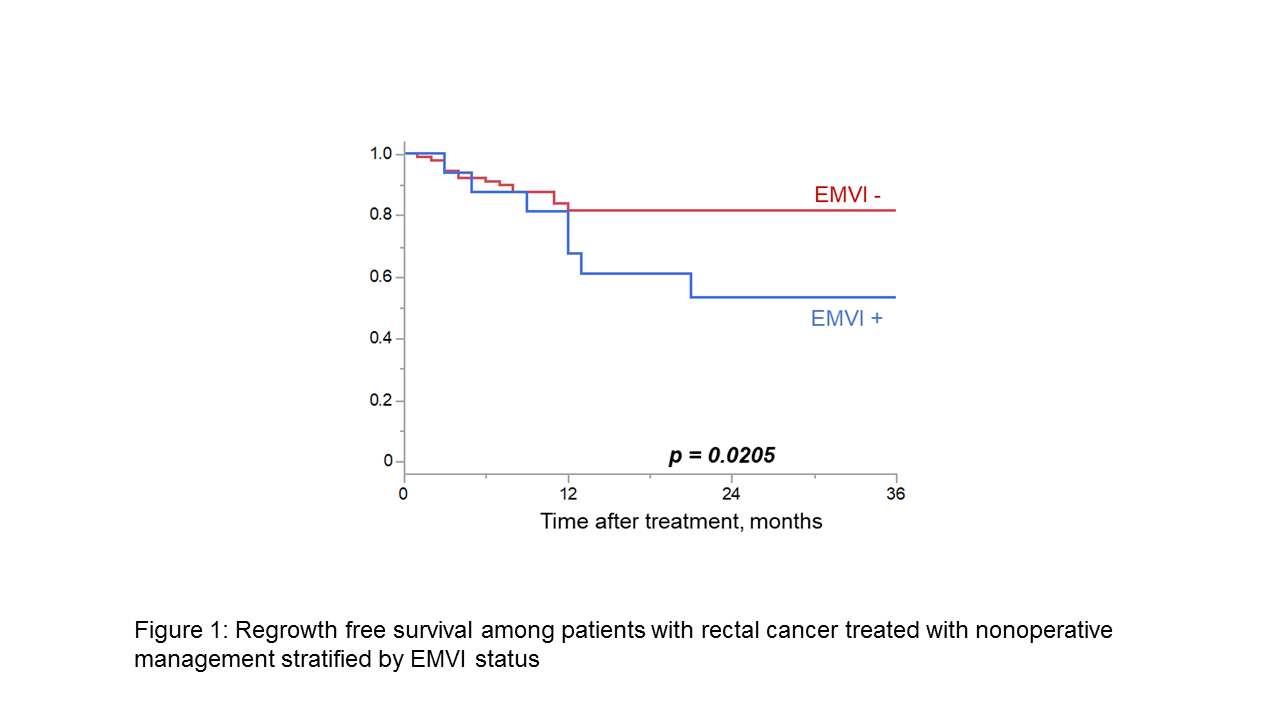
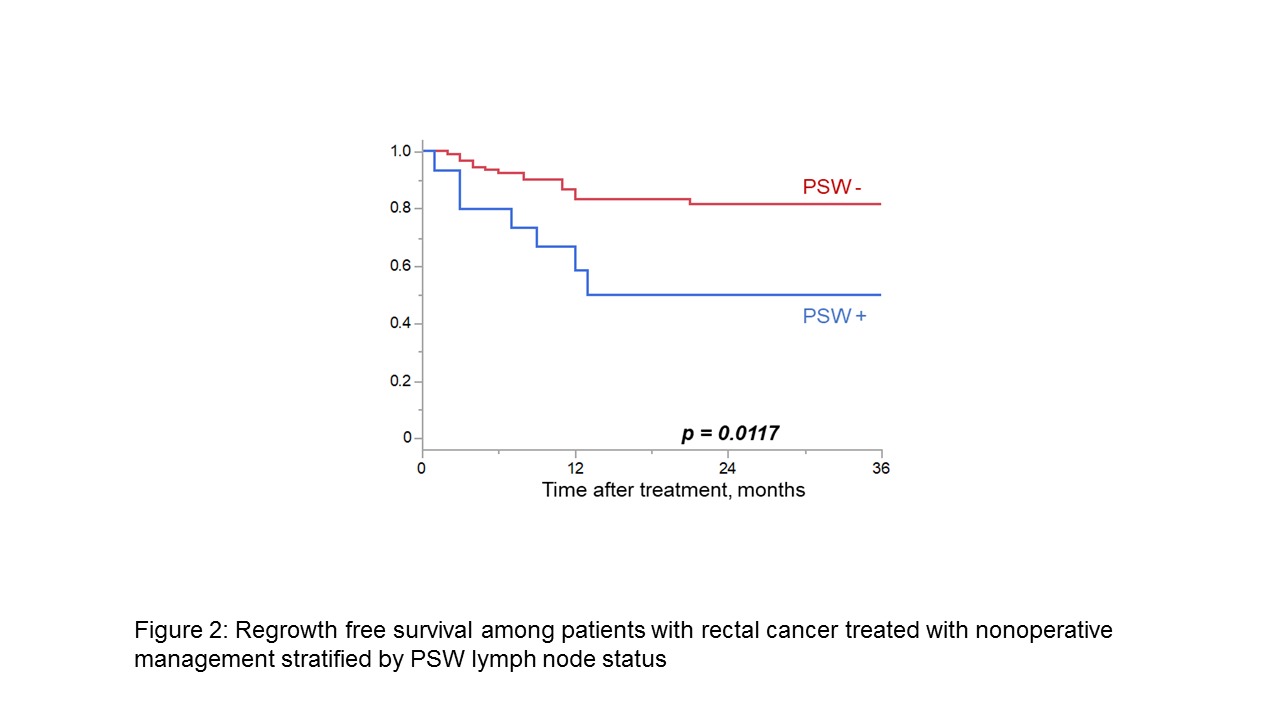
ResultsA total of 131 patients were included in this analysis, of whom 27 (20.6%) experienced local regrowth and 9 (6.9%) experienced distant metastasis at a median follow-up of 27 months (range 1-111 months). Patients with tumors demonstrating extramural vascular invasion (EMVI; Figure 1) or clinically positive pelvic sidewall lymph nodes (PSW; Figure 2) had significantly worse RFS (HR:2.56 [1.12-5.90], p=0.02, HR:2.89 [1.21-6.89], p=0.01, respectively). Pre-treatment clinical T category, node status, tumor distance from the anal verge, or circumferential resection margin were not associated with RFS. Moreover, RFS was similar regardless of chemotherapy receipt (long-course chemoradiation alone versus long-course chemoradiation + chemotherapy versus short-course radiation + chemotherapy; p=0.54). RFS of patients with cCR (n=79, 60.3%) and nCR (n=38, 29.0%) at first endoscopic re-evaluation were similar (HR:1.47 [0.35-1.52], p=0.35). However, among patients without regrowth at 1 year, risk of subsequent regrowth trended toward being lower if initial endoscopy demonstrated cCR (HR 3.96 [0.87-18.1], p=0.076).
Conclusions Patients with rectal cancer high-risk features on MRI, namely EMVI and positive PSW nodes, may be more likely to experience tumor regrowth even after complete or near-complete clinical response to therapy. Patients with a near-complete endoscopic response may be at higher risk of later regrowth. The decision to attempt NOM in this patient population should be carefully weighed against the increased risk of tumor regrowth.
Back to 2024 Abstracts