Back to 2024 Abstracts
TRENDS IN COST SHARING AND CANCER TREATMENT MODALITY UTILIZATION AMONG COMMERCIALLY INSURED PATIENTS WITH GASTROINTESTINAL CANCER
Erryk Katayama
1,2, Selamawit Woldesenbet
1, Diamantis Tsilimigras
1, Muhammad Muntazir M. Khan
1, Yutaka Endo
1, Muhammad Muntazir Mehdi Khan
1, Timothy M. Pawlik
*11Surgery, The Ohio State Wexner Medical Center, Columbus, OH; 2The Ohio State University College of Medicine, Columbus, OH
Introduction: The cost of healthcare is widely recognized as a substantial barrier to access essential medical care. The association of commercial insurance type, out-of-pocket (OOP) cost sharing, and receipt of treatment, particularly the utilization of surgery, remain ill-defined among patients with gastrointestinal cancer.
Methods: The MarketScan commercial insurance claims database was queried to identify patients diagnosed with esophageal, gastric, hepatic, pancreatic, and colorectal cancers between 2013-2020. Patient OOP cost sharing (including coinsurance, deductible, and copay) was analyzed according to insurance plan type (preferred provider organization [PPO], health maintenance organization [HMO], high-deductible health plan [HDHP], consumer-directed health plan [CDHP], noncapitated point of service [POS], capitated point of service [PSC], exclusive provider organization [EPO], and comprehensive [Comp]). Insurance and payment types were examined relative to treatment stratified by modality (surgery, chemotherapy, and radiotherapy) using univariable and multivariable analyses.
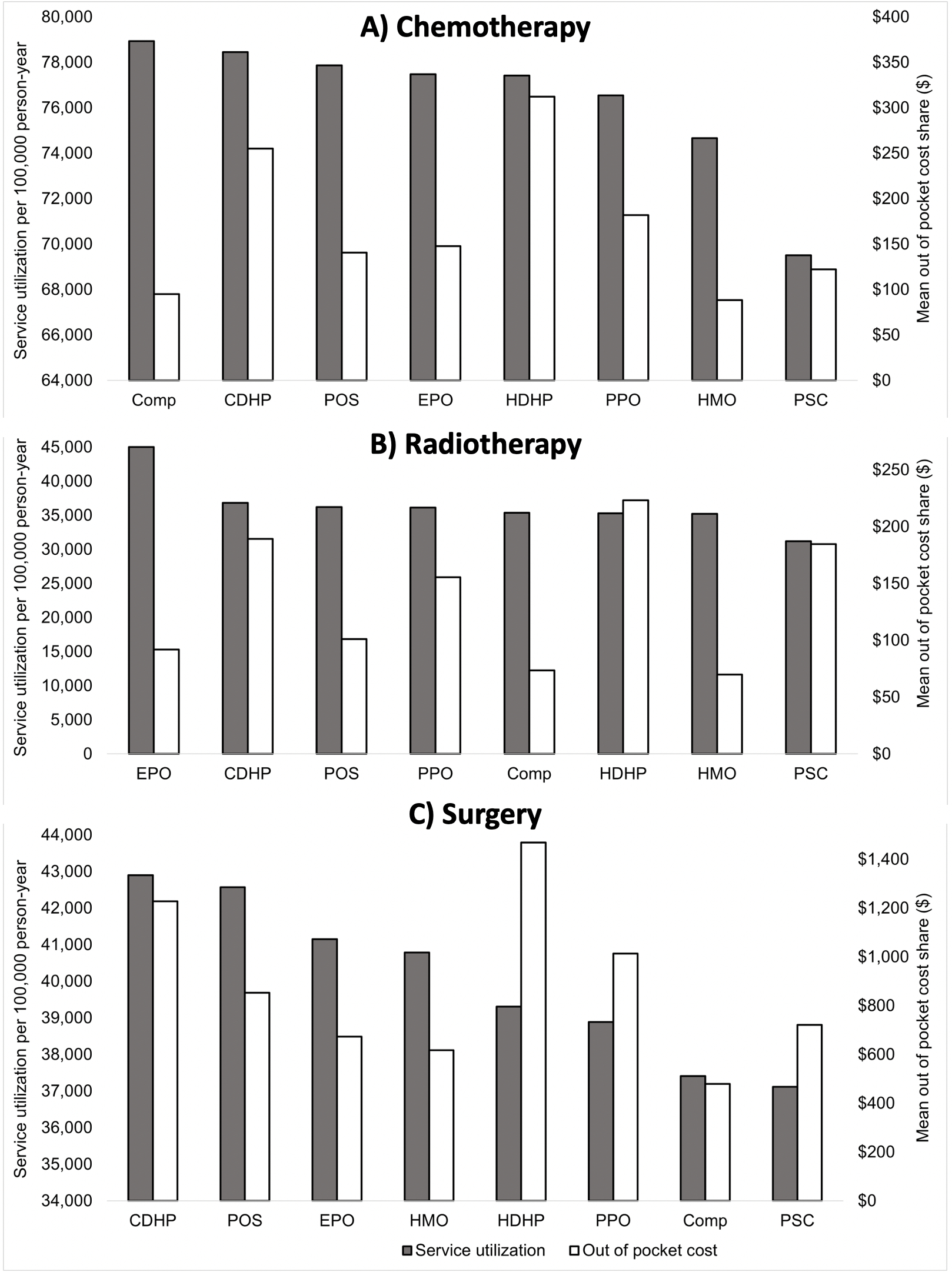
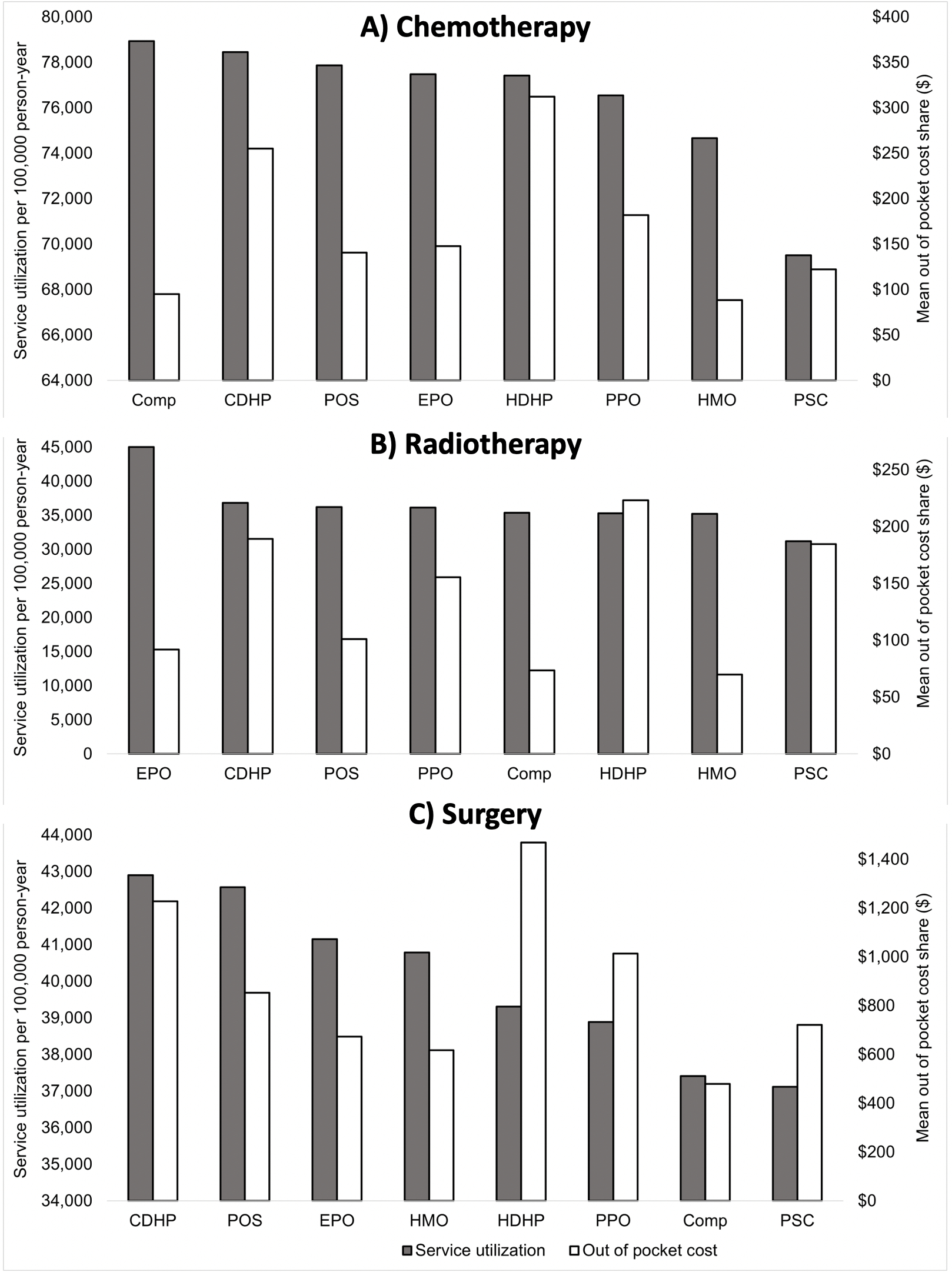
Results: Among 17,104 cancer patients (esophageal: n=564, 3.3%; gastric: n=829, 4.8%; hepatic: n=772, 4.6%; pancreatic: n=1,228, 7.2%; colorectal: n=13,711, 80.1%), insurance plan enrollment varied (PPO: n=9,621, 56.3%; HMO: n=2,002, 11.7%; HDHP: n=1,158, 6.8%; CDHP: n=2,068, 12.1%; POS: n=1,216, 7.1%; PSC: n=140, 0.9%; EPO: n=190, 1.1%; Comp: n=709, 4.1%). Highest OOP costs were associated with HDHP (pre: $2,011; peri: $1,439; post: $5,232), CDHP (pre: $1,792; peri: $1,228; post: $4,419), and PPO (pre: $1,443; peri: $1,014; post: $3,716), while lowest OOP costs were associated with PSC (pre: $566; peri: $721; post: $2,122), HMO (pre: $817; peri: $617; post: $2,257), and EPO (pre: $936; peri: $674; post: $2,419) (all p<0.001). On multivariate analysis, enrollment in PSC (OR 0.67 [95%CI 0.51-0.87]) and HMO (OR 0.86 [0.76-0.97]) were associated with lower odds of receiving chemotherapy. In contrast, enrollment in POS (OR 1.14 [1.01-1.30]) and CDHP (OR 1.16 [1.04-1.30]) were associated with an increased likelihood of surgery; patients enrolled in EPO (OR 1.50 [1.16-1.94]) had higher radiotherapy utilization. Of note, OOP costs were not associated with utilization of chemotherapy, surgery, or radiotherapy (
Figure). Among patients who underwent a procedure, insurance plan was not associated with post-operative outcomes including complications, prolonged length of stay, and readmission within 90-days (all p>0.05).
Conclusion: There was marked variation among gastrointestinal cancer patients across insurance plans. OOP costs were not associated with utilization of chemotherapy, surgery, or radiotherapy. Rather, their insurance type correlated with the relative use of various multi-modality therapies. Insurance status may be a driver of access to comprehensive cancer care.
Back to 2024 Abstracts