Back to 2024 Abstracts
IMPACT OF END-ILEOSTOMY VERSUS ILEAL POUCH-ANAL ANASTOMOSIS ON GRAFT-SURVIVAL FOLLOWING LIVER TRANSPLANTATION FOR PRIMARY SCLEROSING CHOLANGITIS
Lukas Schabl
*1,2, Marianna Maspero
1, Stefan D. Holubar
1, Tracy L. Hull
11Department of Colorectal Surgery, Cleveland Clinic, Cleveland, OH; 2Universityhospital Salzburg, Department of General, Visceral and Thoracic Surgery, Salzburg, Salzburg, Austria
Background IBD-PSC patients may require both liver transplantation and ileoanal pouch (IPAA) construction. Recently, concerns have been raised regarding an increased rates of hepatic artery thrombosis, biliary strictures, and graft loss in individuals who underwent IPAA after liver transplantation compared to those who underwent end-ileostomy (EI). We hypothesized that graft survival was not negatively affected by IPAA compared with EI.
Methods A prospectively maintained database from a large tertiary center was searched for patients meeting the inclusion criteria for liver transplantation, primary sclerosing cholangitis, ulcerative colitis, and total colectomy with IPAA or EI. Univariate analysis and Kaplan-Meier survival curves were calculated.
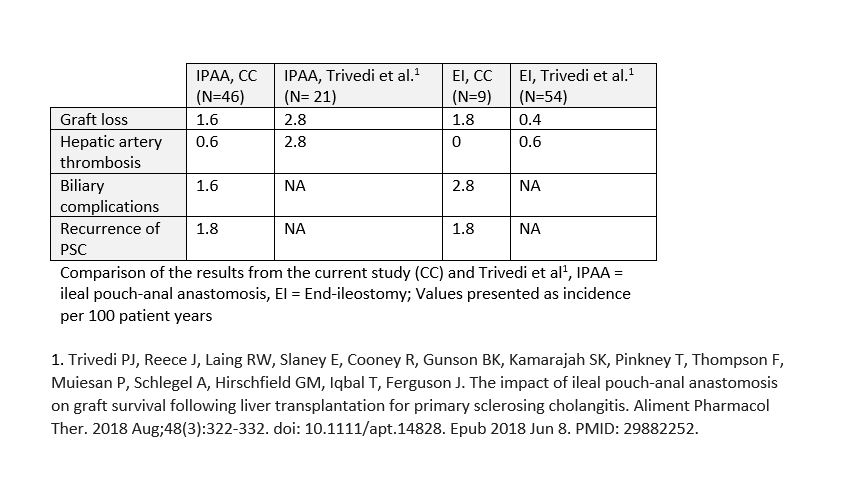
Results Between January 1990 and December 2023, 55 patients met inclusion criteria. Of these, 46 (83.6%) underwent IPAA, and 9 (16.4%) underwent EI. The average age at colectomy (41.7 vs. 45.7 years; p=0.44), sex distribution (female: 26.1% vs. 22.2%, p=1), and MELD score before transplantation (20.3 vs. 14; p=0.06) were comparable between patients with IPAA and EI patients. The rates of re-transplantation (21.7% vs. 22.2%; p=1), hepatic artery thrombosis (8.7% vs. 0; p=1), episodes of acute rejection (32.6% vs. 44.4%; p=0.7), chronic rejection (4.3% vs. 11.1%; p=0.42), recurrence of primary sclerosing cholangitis (23.9% vs. 22.2%; p=1), and biliary complications (21.7% vs. 33.3%; p=0.43) were similar between the IPAA and EI groups, respectively. None of the EI patients developed parastomal varices. Survival analyses for time to re-transplantation (p=0.97), overall survival (p=0.3), and time to graft loss or mortality (p=0.73) were similar.
Conclusion In contrast to a previous study, we observed similar rates of liver transplant graft loss, biliary complications, and recurrent PSC after IPAA compared to those after end-ileostomy. IPAA may be associated with an increased rate of hepatic artery thrombosis.
Back to 2024 Abstracts