Back to 2024 Abstracts
ERCP FOR MANAGEMENT OF POST-CHOLECYSTECTOMY BILE LEAKS IN PATIENTS WITH SUBTOTAL VERSUS TOTAL CHOLECYSTECTOMY: A COMPARATIVE ANALYSIS
Ashley Gao
*1, Sujani Yadlapati
1, Azizullah Beran
1, Benjamin L. Bick
2, Nasir Saleem
1, Mark A. Gromski
1, Evan L. Fogel
1, Aditya Gutta
1, Itegbemie Obaitan
1, James L. Watkins
1, Michael G. House
1, Nicholas J. Zyromski
1, Ryan J. Ellis
1, Eugene P. Ceppa
1, Jeffrey J. Easler
11Gastroenterology, Indiana University School of Medicine, Indianapolis, IN; 2Rockford GI associates, Rockford Gastroenterology Associates, IL
Introduction Laparoscopic subtotal cholecystectomy (STC) is an established approach for difficult cholecystectomy (CCY) and is endorsed by guidelines as a strategy to mitigate risk for complications such as bile duct injury. Incidence of post-CCY bile leak is higher in patients following STC compared to total cholecystectomy (TC). Endoscopic retrograde cholangiopancreatography (ERCP) with biliary sphincterotomy and/or bile duct stent placement is the most effective intervention for bile leaks after CCY. With increasing adoption of STC for complex CCY, a comprehensive understanding of the effectiveness of ERCP for bile leak after STC is imperative. We offer a comparative analysis of the clinical, peri-procedure details and outcomes for patients managed with ERCP for bile leak complications after STC and TC.
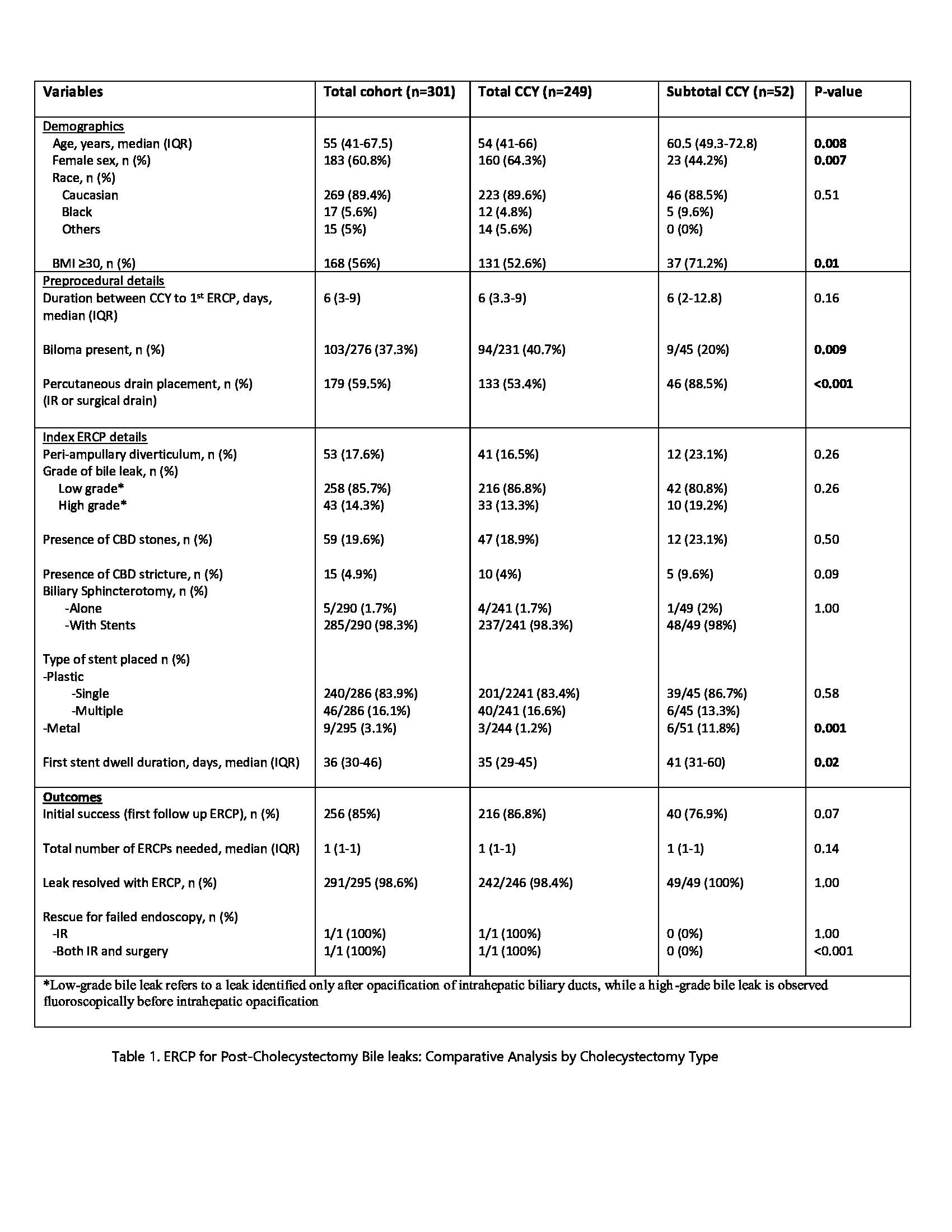
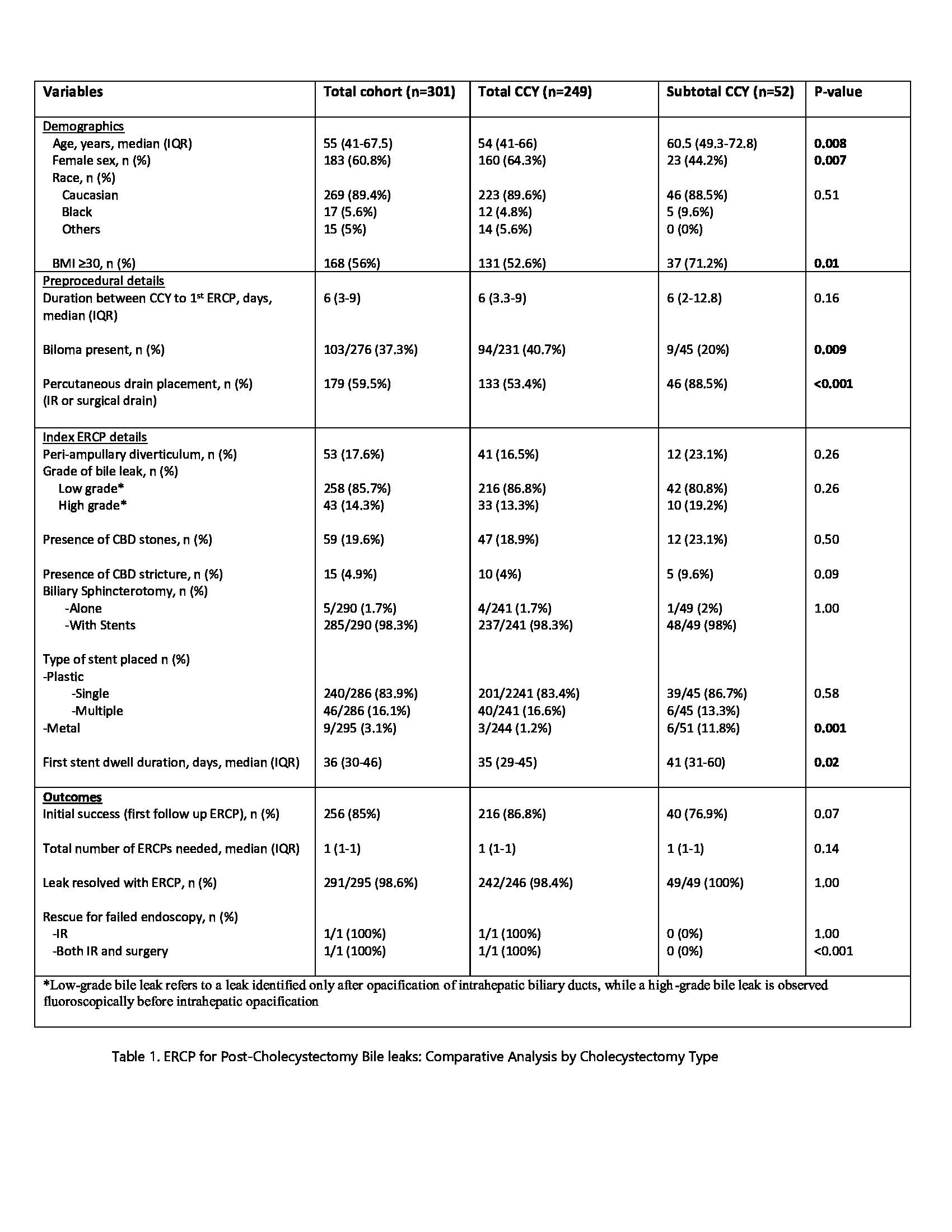
MethodsData on patients referred for ERCP at Indiana University Health (IUH) University Hospital between 2011-21 was collected within a retrospective database. Patients with Strasberg A bile leaks and/or leak from the gallbladder remnant were included in the analysis. Bile leaks with etiologies other than CCY (e.g. hepatectomy, trauma) or additional CCY complications (e.g. bile duct injury) were excluded. Operative reports, ERCP cholangiogram findings and post-CCY cross sectional imaging were reviewed to verify a TC or STC status.Bile leaks classified as high grade were identified before intrahepatic duct opacification. Evaluated outcomes include resolution of bile leak at first follow up ERCP, total number of ERCPs required for resolution and overall success of ERCP for leak resolution.
ResultsAmong bile leak patients, 301 met study criteria. STC patients were older, had a higher BMI and were more often male (Table 1). STC patients more frequently had a drain (p<0.001) and less often a biloma at the time of ERCP (p=0.009). Although no differences were observed in the grade of bile leaks between groups, STC patients were more frequently treated with placement of self-expanding metal biliary stents (SEMS) (p=0.001) and a longer stent dwell time after the index ERCP (41 vs 35 days, p=0.02). Overall success rate for leak resolution was high with ERCP (98%). While a trend for higher rate of leak resolution at first follow up ERCP for TC patients (p=0.07), total number of ERCP procedures and overall success of ERCP for managing post CCY bile leak was no different between the two groups.
ConclusionERCP remains an effective strategy for resolution of bile leak in patients after CCY, including those patients that require a STC. In our cohort, the utilization of strategies such as SEMS and extended stent dwell time was more frequent in patients with STC and was deployed based on the discretion of the ERCP physician. In this context there were no differences in ERCP procedure burden or rates of bile leak resolution between TC and STC patients.
Back to 2024 Abstracts