Back to 2024 Abstracts
USE OF AIR LEAK TEST TO REDUCE BILE LEAKS AND ORGAN SPACE INFECTIONS: A STEP TOWARDS MORE DRAIN-FREE HEPATECTOMY PATIENTS
Laurence P. Diggs
*, Antony Haddad, Elsa M. Arvide, Whitney L. Dewhurst, Anny M. Jin, Timothy E. Newhook, Hop S. Tran Cao, Yun Shin Chun, Jean-Nicolas Vauthey, Ching-Wei D. Tzeng
Surgical Oncology, The University of Texas MD Anderson Cancer Center Division of Surgery, Houston, TX
Introduction: Though still common practice, the indications for surgical drain placement following hepatectomy have been put into question. Bile leak (BL) testing using an air leak test (ALT) or “air cholangiogram� is performed in patients thought to be high-risk for BL and organ space infection (OSI). We examined whether ALT and surgical drain can help reduce BL/OSI post hepatectomy.
Methods: Our department keeps a faculty and advanced practice provider-reviewed prospective quality improvement database that tracks 90-day surgical outcomes for all hepatectomy patients. This was queried from January 2017 to June 2023 for consecutive liver-only cases. Patients were stratified based on complication risk classification, ALT, surgical drain placement, and BL/OSI. BL was defined by international criteria. OSI was defined as abscess or deep surgical site infection. Patients were risk-stratified using the Kawaguchi-Gayet (KG) classification into high-risk vs low-risk depending on whether they underwent KG3 vs KG1-2 resection, respectively.
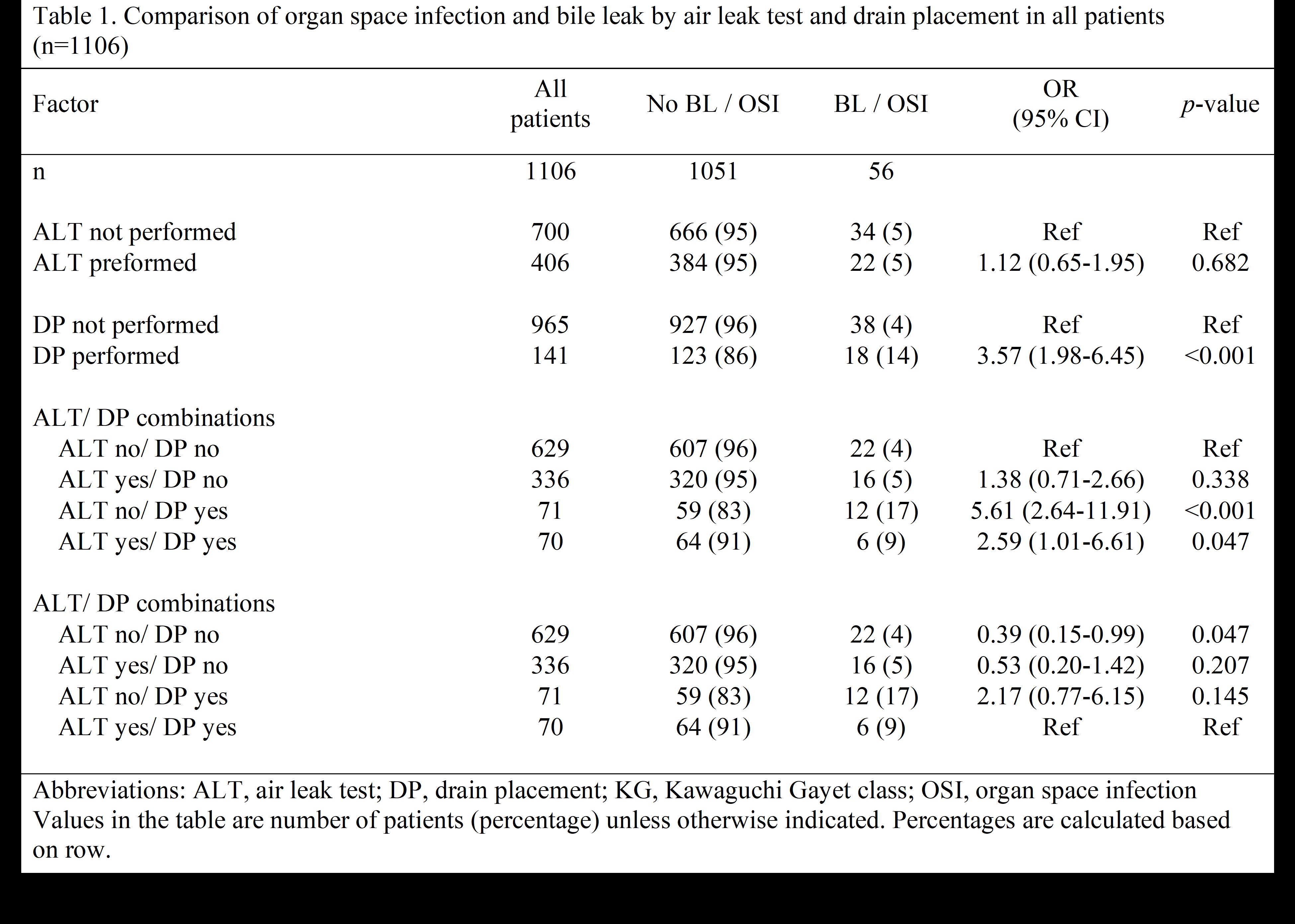
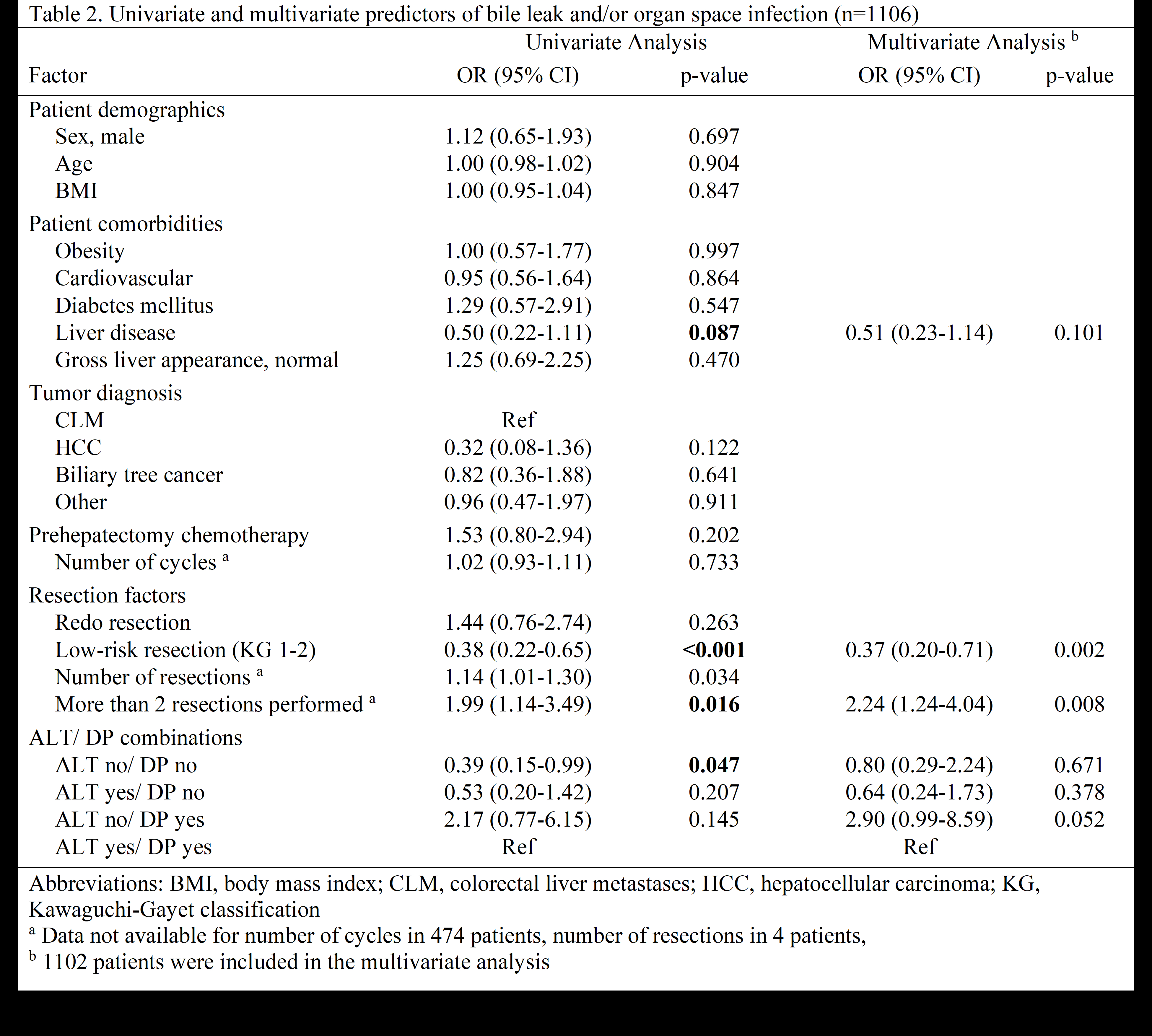
Results: We identified 1106 patients including 401 who underwent high-risk hepatectomies. ALT was performed in 63.1% (253/401) of high-risk vs 21.7% (153/705) of low-risk patients. Surgical drains were placed in 23.7% (95/401) of high-risk vs. 6.5% (46/40) of low-risk cases. BL/OSI was clinical detected in 8.2% (33/401) of high-risk and 3.3% (23/705) of low-risk patients. Surgical drain was associated with increased incidence of BL/OSI in both high-risk and low-risk patients (p=0.027 and p=0.003, respectively). Among all patients who underwent ALT, absence of surgical drain was not associated with increased BL/OSI (OR 0.53, p=0.207) (Table 1). Among patients without ALT, presence of surgical drain was associated with increased incidence of BL/OSI (OR 5.61, p<0.001). On multivariable analysis (Table 2), absence of surgical drain in patients who underwent ALT was not independently associated with an increased incidence of BL/OSI (OR 0.64, p=0.378). Technical factors associated with BL/OSI were performing more than 2 resections (OR 2.24, p=0.008) and low risk resection (OR 0.37, p=0.002).
Discussion: When ALT is performed, surgical drain placement is not associated with changes in BL/OSI rates. Though drain placement may be deemed necessary by the surgeon in certain high-risk patients, ALT can augment the ability to identify occult bile leaks and thus safely increase the number of drain-free patients.
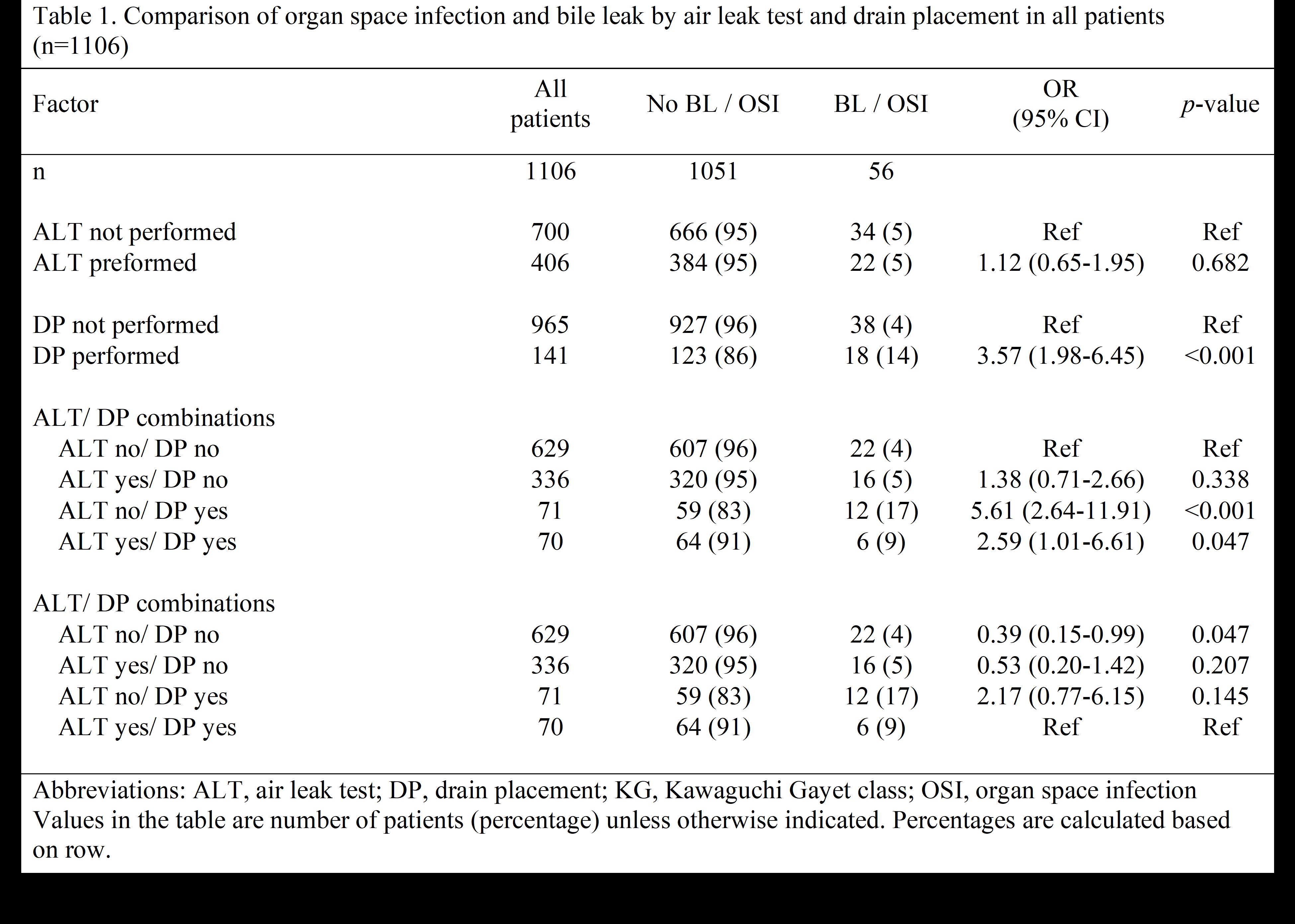
TABLE 1. Comparison of organ space infection and bile leak by air leak test and drain placement in all patients.
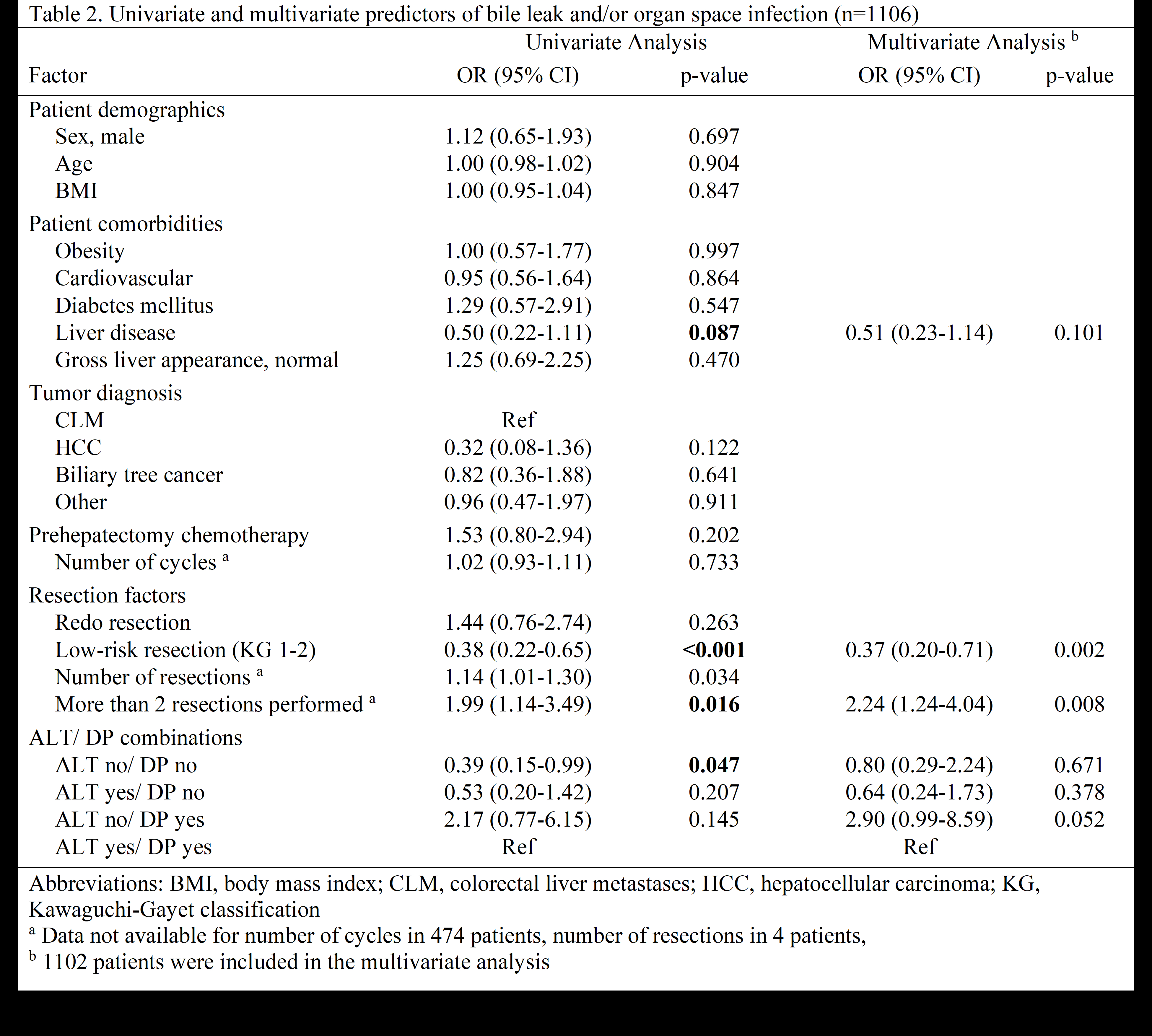
TABLE 2. Univariate and multivariate predictors of bile leak and/or organ space infection.
Back to 2024 Abstracts