Back to 2024 Abstracts
DEVELOPMENT OF AN ARTIFICIAL INTELLIGENCE BASED MODEL TO PREDICT EARLY RECURRENCE OF NEUROENDOCRINE LIVER METASTASIS FOLLOWING RESECTION
Abdullah Altaf
*1, Muhammad Muntazir M. Khan
1, Muhammad Muntazir M. Khan
1, Yutaka Endo
1, Mujtaba Khalil
1, Zayed Rashid
1, Alfredo Guglielmi
2, Luca Aldrighetti
3, Todd W. Bauer
4, Hugo P. Marques
5, Guillaume Martel
6, Vincent Lam
7, Matthew Weiss
8, Ryan C. Fields
9, George A. Poultsides
10, Shishir K. Maithel
11, Itaru Endo
12, Timothy M. Pawlik
11Surgery, The Ohio State Wexner Medical Center, Columbus, OH; 2Universita degli Studi di Verona Scuola di Medicina e Chirurgia, Verona, Veneto, Italy; 3IRCCS Ospedale San Raffaele, Milano, Italy; 4University of Virginia School of Medicine, Charlottesville, VA; 5Hospital Curry Cabral, Lisboa, Lisboa, Portugal; 6University of Ottawa Faculty of Medicine, Ottawa, ON, Canada; 7Westmead Hospital, Westmead, New South Wales, Australia; 8Johns Hopkins Medicine, Baltimore, MD; 9Washington University in St Louis School of Medicine, St Louis, MO; 10Stanford University School of Medicine, Stanford, CA; 11Emory University School of Medicine, Atlanta, GA; 12Yokohama Shiritsu Daigaku Igakubu Daigakuin Igaku Kenkyuka, Yokohama, Kanagawa, Japan
Background: Recurrence of neuroendocrine tumor liver metastasis (NELM) following curative-intent resection occurs in a large subset of patients. Artificial intelligence (AI) may help predict outcomes among patients with cancer. We sought to develop an AI based model to predict early recurrence following curative-intent resection of NELM.
Methods: Patients who underwent curative-intent resection for NELM were identified from an international multi-institutional database. Early recurrence was defined as recurrence within 12 months of surgical resection. Different machine learning (ML) and deep learning (DL) techniques were employed to develop prediction models for early recurrence.
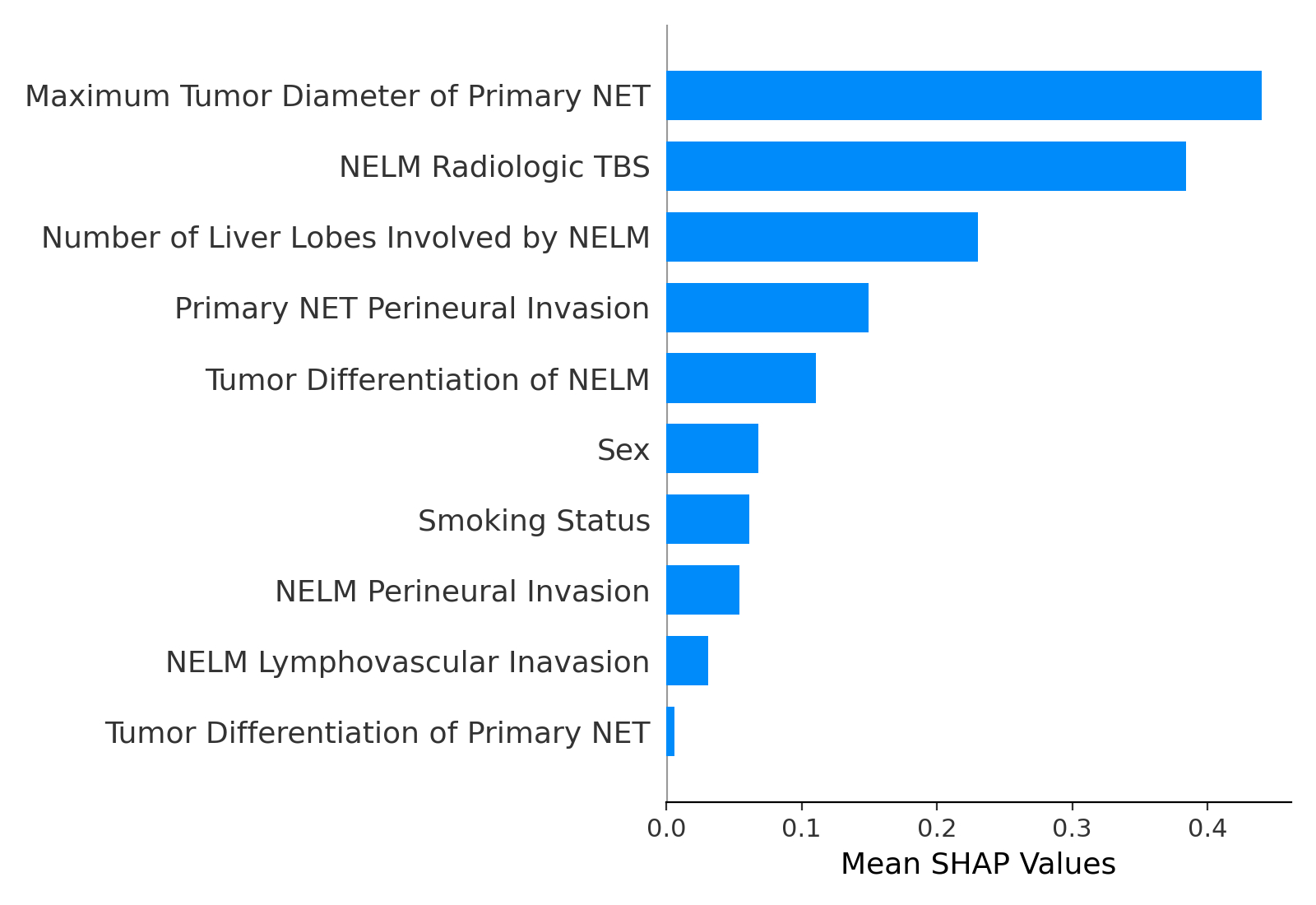
Results: 473 NELM patients were randomized into training (n= 378, 79.9%) and testing (n= 95, 20.1%) cohorts. Among 284 (60.0%) patients who developed NELM recurrence with a median follow-up period of 55 months (IQR, 23-94), 118 (41.5%) patients developed an early recurrence. Ten clinicopathological factors were identified as most strongly correlated with early recurrence on correlation heatmap and were used to train the AI models. Among the different AI techniques, an ensemble model consisting of Multi-Layer Perceptron (MLP) and Gradient Boosting (GB) classifiers demonstrated the highest accuracy with area under receiver operating characteristic curve (AUC) of 0.763 (95% CI, 0.705-0.821) and 0.716 (95% CI, 0.593-0.828) in the training and testing cohorts, respectively. Specifically, maximum diameter of the primary neuroendocrine tumor (NET), NELM radiologic tumor burden score (TBS), and bilateral liver involvement were the factors most strongly associated with risk of early NELM recurrence, as demonstrated on the SHAP summary plot (
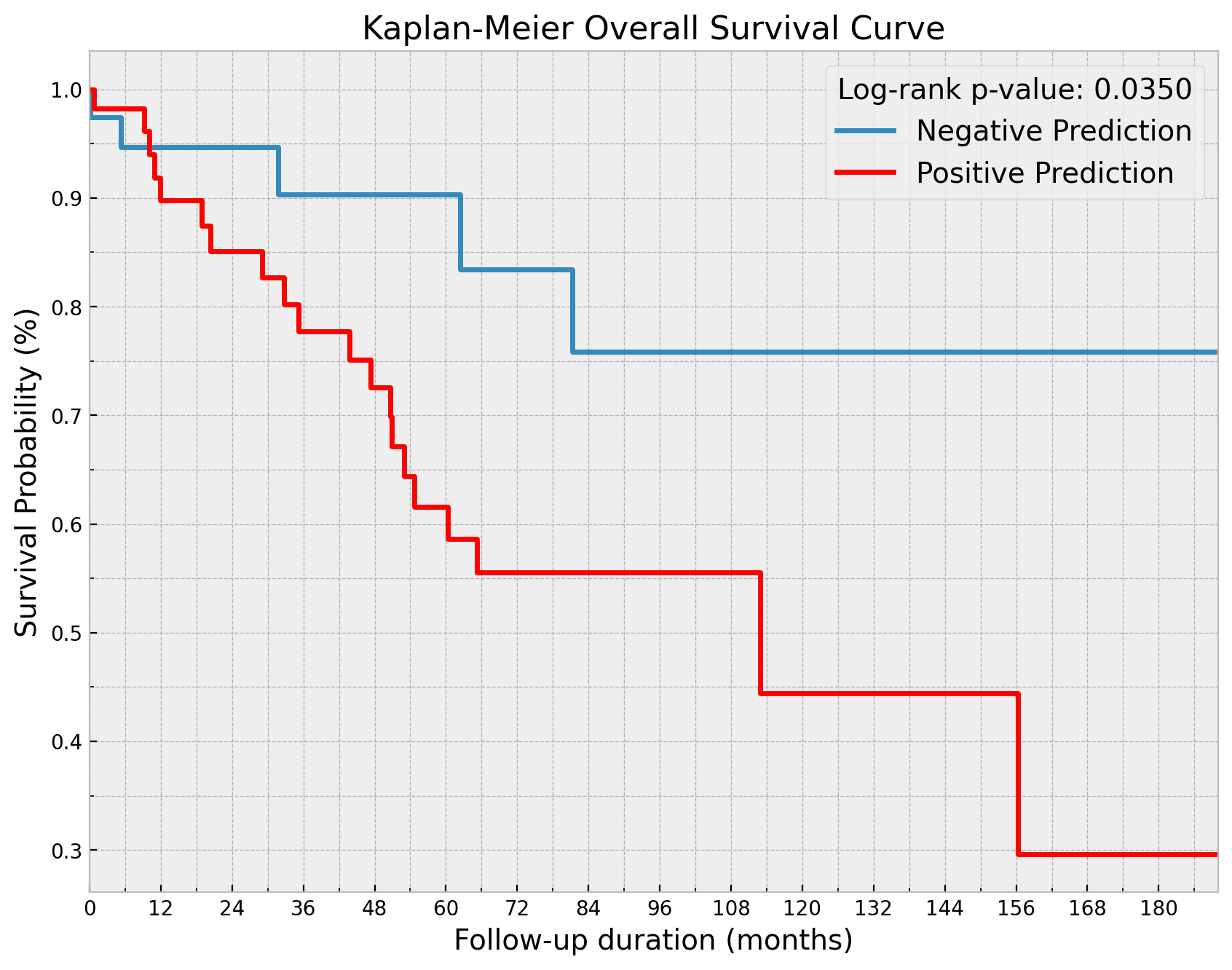
Figure 1). Patients predicted to develop early recurrence had worse 5- (21.4% vs. 37.1%), and 10-year (12.8% vs. 37.1%) recurrence free survival (RFS) versus patients not predicted to recur (p=0.002). Similarly, patients predicted to experience early recurrence had worse 5- (61.6% vs. 90.3%) and 10-year (44.4% vs. 75.8%) overall survival (OS) compared with patients not predicted to recur within 12 months (p=0.03) (
Figure 2).
Conclusion: An AI based model demonstrated very good discrimination to predict early recurrence following resection of NELM. AI models such as the one proposed here may help identify which patients benefit the most from curative-intent resection, as well as inform treatment decisions around surgical versus non-surgical treatment options for patients with NELM.
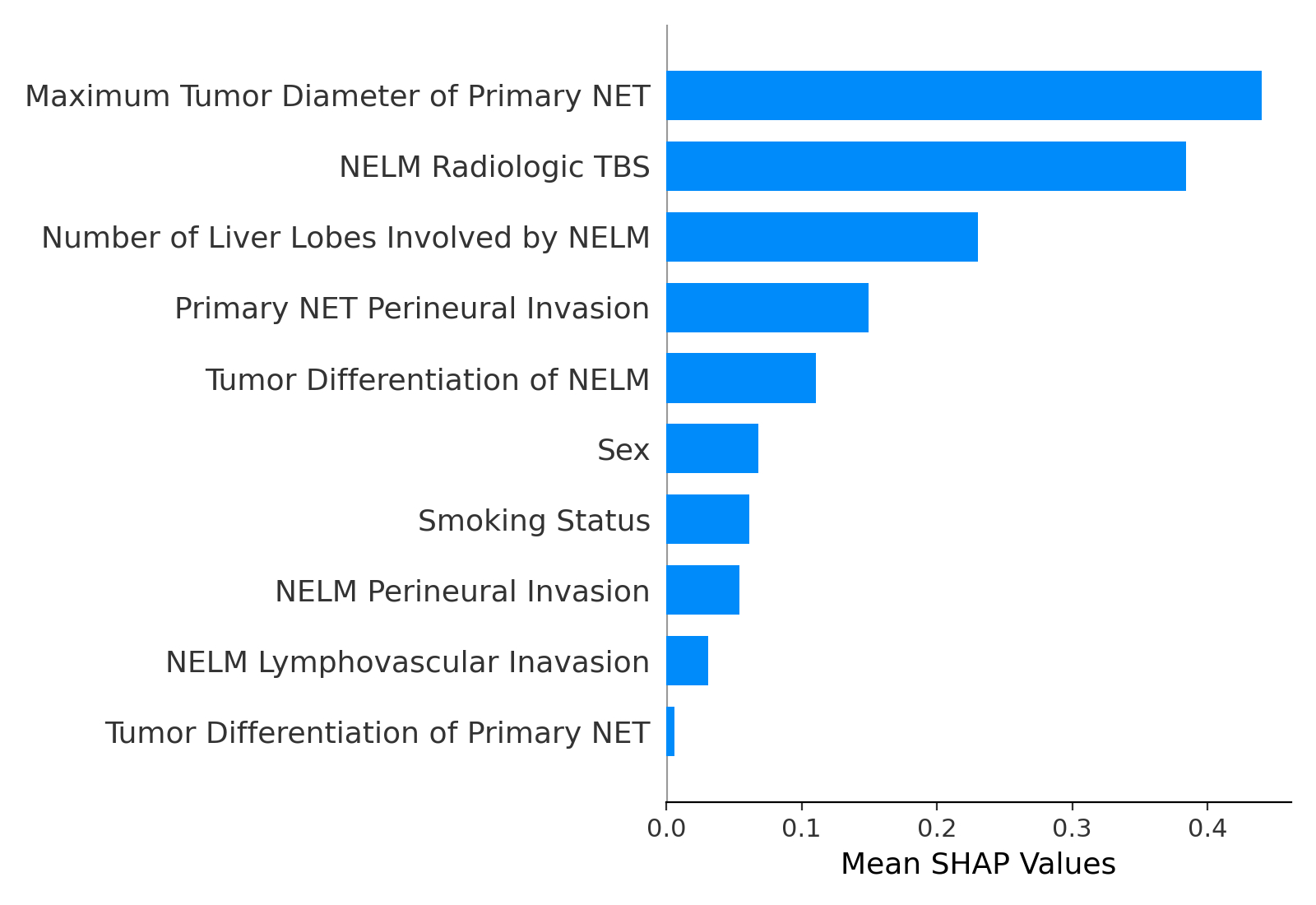
SHAP Summary Plot Showing Factor Weightages
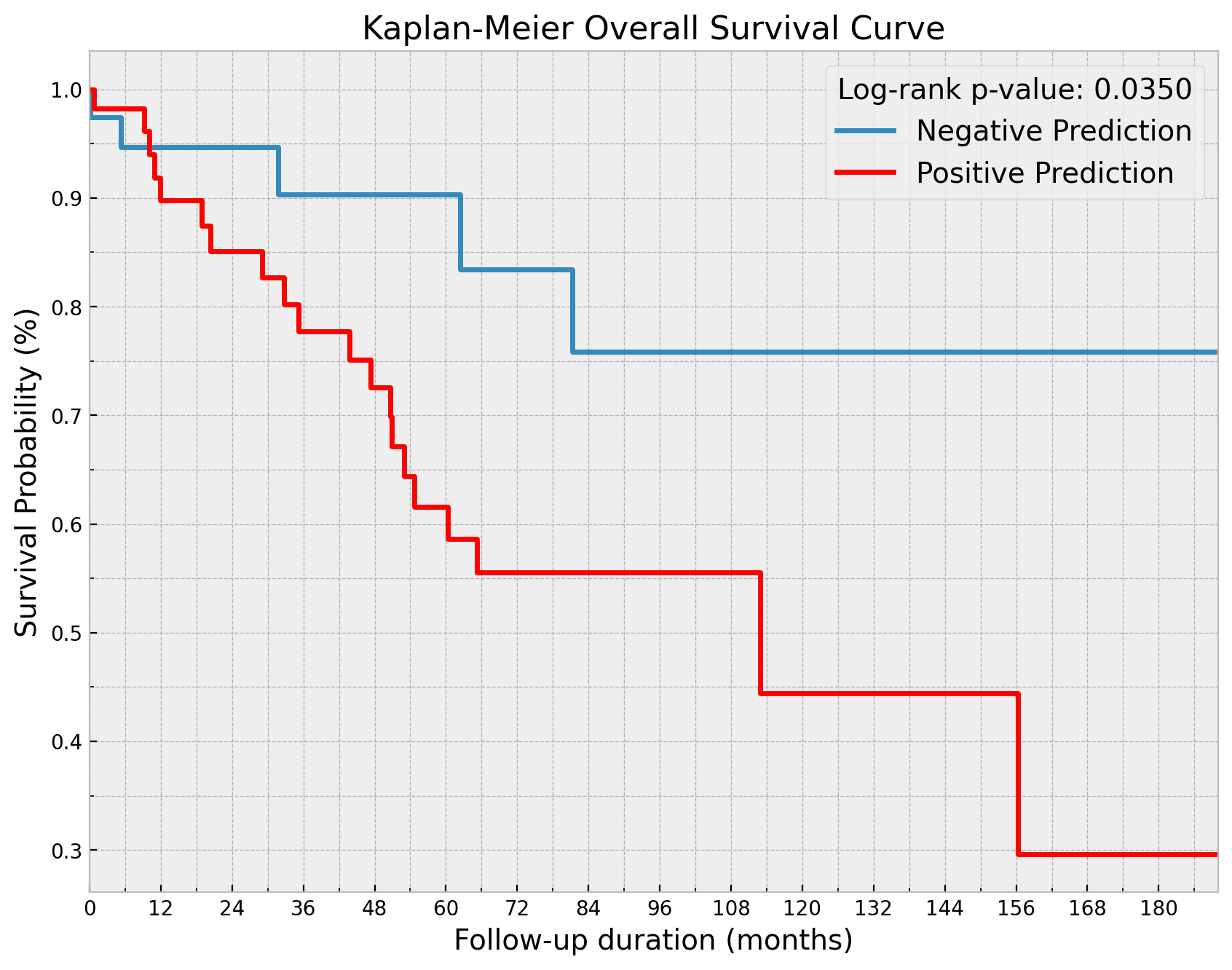
Kaplan Meier Curves for OS
Back to 2024 Abstracts