Back to 2024 Abstracts
PERIOPERATIVE COVID-19 INFECTION IS ASSOCIATED WITH SIGNIFICANT MORBIDITY AND HOSPITAL RESOURCE UTILIZATION FOLLOWING HEPATOBILIARY AND PANCREATIC SURGERY
Terhas Weldelase
*1, Jan Franko
2, Anna Lin
1, Monica Silva
2, Phiwinhlanhla Ndebele-Ngwenya
1, Oluwasegun Akinyemi
1, Quyen Chu
1, May Tee
1,21Surgery, Howard University, Washington, ; 2MercyOne, Des Moines, IA
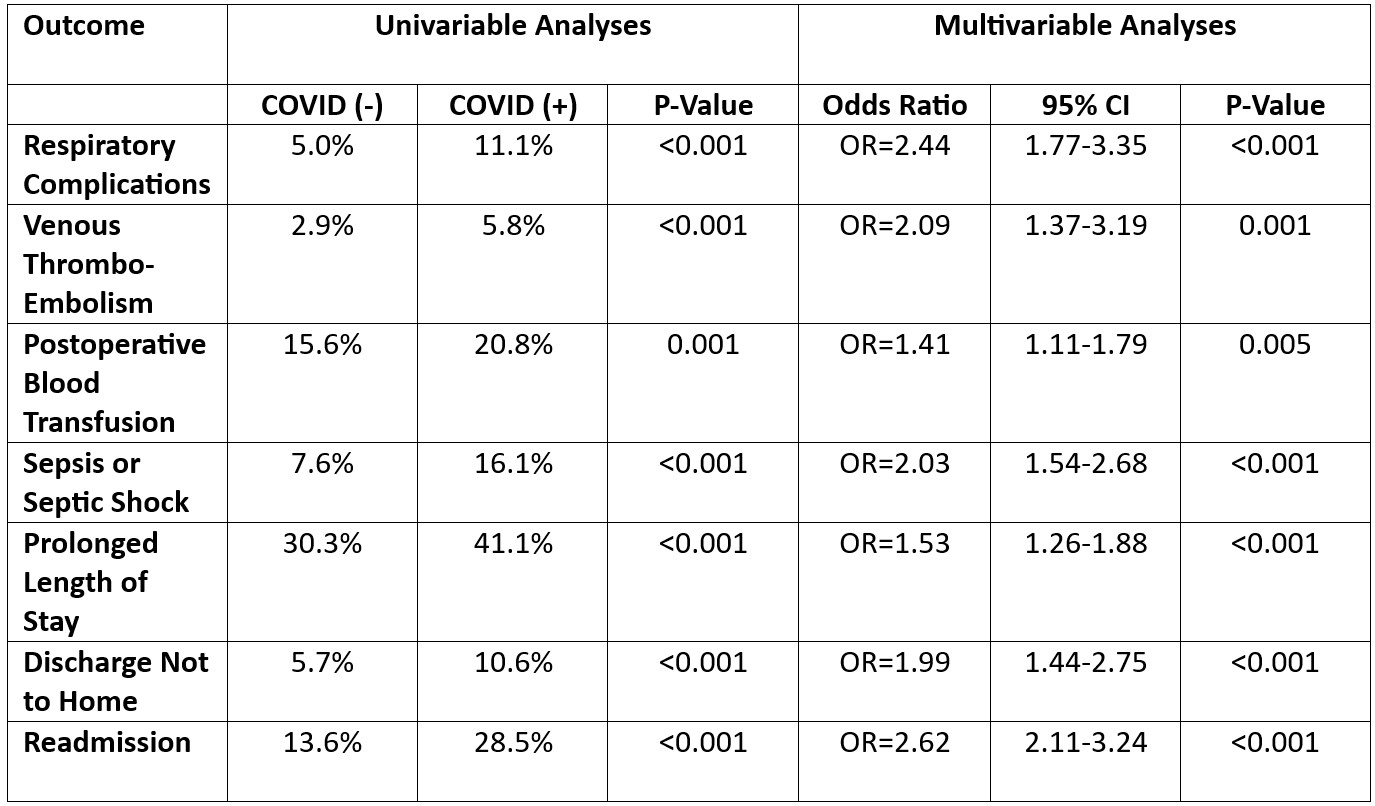
BackgroundPrior studies demonstrate increased postoperative morbidity associated with perioperative COVID-19 infection in patients undergoing elective or emergent major abdominal surgery. For patients undergoing elective hepatobiliary and pancreatic surgery, we sought to determine perioperative outcomes and hospital resource utilization in patients who were diagnosed preoperatively or within 30 days of their operation with COVID-19 infection.
MethodsThe American College of Surgeons (ACS) National Surgical Quality Improvement Project (NSQIP) participant use file was queried from 2021 to 2022 to include major hepatectomy (47120, 47122, 47125, 47130) and pancreatectomy (48120, 48140, 48145, 48146, 48150, 48152-48155, 48160), as defined by Current Procedural Terminology codes. Univariable and multivariable analyses were utilized to examine the association between perioperative COVID-19 infection and 30-day outcomes including respiratory, thromboembolic, bleeding, and septic outcomes. Additionally, the association between perioperative COVID-19 infection and length of stay, readmission, reoperation, discharge to destination other than home, and mortality were examined. All analyses were conducted using Stata v17.
ResultsA total of N=30,121 elective hepatobiliary and pancreatic resections were included for analysis. Univariable and multivariable results are summarized in the
Table below, comparing patients infected with perioperative COVID-19 (COVID+) versus those who were not (COVID-). Prolonged length of stay was defined at ≥ 8 days, the 75
th percentile of the cohort. Composite end points were created for respiratory complications (pneumonia, failure to wean off mechanical ventilation after 48 hours, or unplanned reintubation), venous thromboembolism events (pulmonary embolism or deep vein thrombosis), and sepsis (postoperative sepsis or septic shock). Comparing COVID+ to COVID- patients, there were no differences in 30-day mortality (1.50% vs. 1.59%, P=0.877) or reoperation (5.25% vs. 3.69%, P=0.058).
DiscussionPerioperative COVID-19 infection is associated with a greater than 2-fold odds of respiratory, septic, and venous thromboembolic complications in patients undergoing major hepatobiliary and pancreatic surgery. Moreover, there is significant hospital resource utilization associated with perioperative COVID-19 infection with respect to prolonged length of stay in hospital, discharge to a facility other than home, and unplanned readmission to hospital. Careful attention to respiratory symptoms is warranted for these patients, particularly as routine preoperative COVID-19 testing, and hospital mask mandates are relaxed.
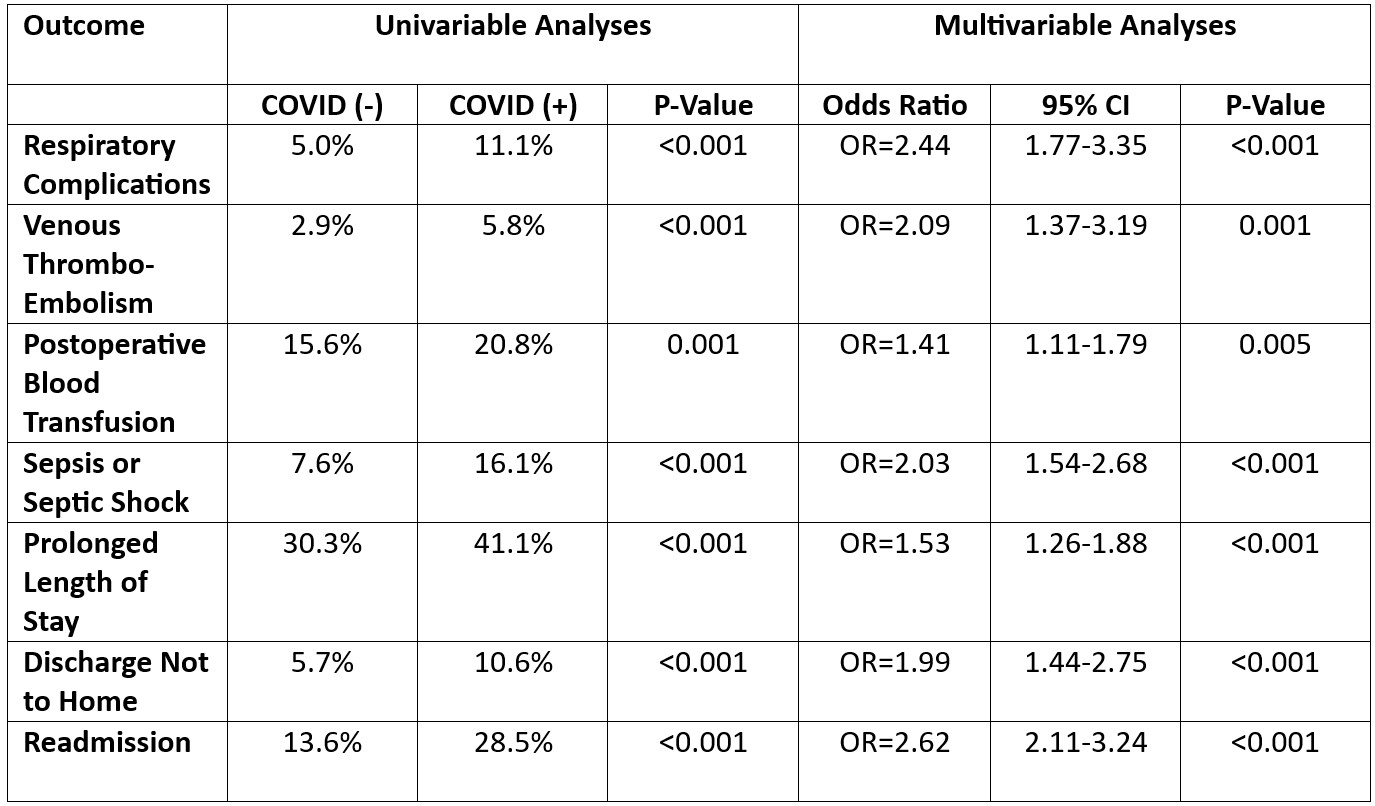 Table
Table
Back to 2024 Abstracts